Abstract
Background
Posterior uterine wall rupture is extremely uncommon in the absence of any of the commonly recognized risk factors. Even though uterine rupture is more likely in multiparous people, it cannot be believed that the uterus of a primigravid is impervious to rupture. The objective of this case report is to alert obstetricians about atypical posterior uterine wall rupture presentation in the absence of identifiable risk factors and to emphasize the worth of prompt action.
Case Presentation
A 22-year-old primigravid mother with a 12 cm vertical posterior uterine wall rupture of an unscarred uterus at St. Paul's Hospital in Ethiopia was reported to have survived an intrapartum uterine rupture during the latent early stage of labor while taking a low dose of oxytocin. The baby was saved from the abdominal cavity after an emergency laparotomy was performed. Complete hemostasis was achieved when the posterior uterine wall rupture was repaired in two layers. The patient and her baby were discharged on the fifth postoperative day smoothly.
Conclusion
Posterior uterine wall rupture in a primigravid mother with an unscarred uterus is extremely rare, but a high index of suspicion should be kept in mind as expedited intervention is the only way to save the mother and fetus.
Introduction
Uterine rupture is a devastating labor complication with a fetal mortality rate as high as 83% and a virtually 100% newborn fatality rate.Citation1,Citation2 Primary uterine rupture occurs in an intact or unscarred uterus, whereas secondary uterine rupture is related to a previous myometrial incision, damage, or malformation.Citation3
Unscarred pregnancy uterine rupture is an uncommon occurrence that is thought to take place in 1/5700 to 1/20,000 pregnancies.Citation1,Citation4 The anterior lower portion of the uterus is where the majority of ruptures in unscarred uteruses take place; posterior wall ruptures are scarce. Even more atypical is posterior uterine wall rupture, which has only a few instances published in the literature so far.Citation5 One in 42,122 pregnancies has been shown to have an oxytocin-related rupture of the unscarred uterus in primigravid women, which is exceedingly rare.Citation6
However, it is crucial to stress the need for early surgical intervention to avert serious maternal and fetal complications and to urge obstetricians to maintain a high index of suspicion for the unusual presentation of posterior uterine wall rupture.
Here, we describe a highly unusual case of a 22-year-old primigravid woman who, during the first stage of labor, suffered an unscarred posterior uterine wall rupture, had it successfully repaired, and gave birth to a live baby on August 23, 2022 G.C., at St. Paul's Hospital Millennium Medical College, Addis Ababa, Ethiopia.
Case Presentation
A 22-year-old primigravid mother had a routine and uneventful ANC follow-up. She has no significant medical history, such as a uterine operation or procedure. An ultrasound performed during the third trimester revealed a fundal anterior placenta, no obvious congenital anomalies, a cephalic presentation, and an estimated fetal weight of 3.2 kg. She presented with a gush of fluid per vaginum at 41+4/7 weeks of gestation. The pelvis was assessed, and it was clinically adequate. At the start of the induction, the cervix was 2 cm dilated, 50% effaced, soft, anterior, and station-2 (Bishop score of 7), and the liquid was clear.
A low-oxytocin-dose protocol for direct induction was started, with one-to-one midwife monitoring of contractions. The oxytocin infusion rate was increased in 1 ml/min increments every 20 min after the starting rate of 1 ml/min. She was in established labor with oxytocin titrated to uterine activity, regular moderate contractions, and a 3-min pain-free period. During labor follow-up, tachysystole was not documented. There was a record of fetal bradycardia 3 hr after the oxytocin infusion commenced, yet there was still a uterine contraction with mild tenderness and a laterally palpable fetal part. The cervix was 70% effaced and 3 cm dilated; the position of the vertex was occipito anterior at the time, with minimal vaginal bleeding and a highly stationed vertex. The maternal vital signs were stable (blood pressure: 100/60, pulse rate: 96 bpm).
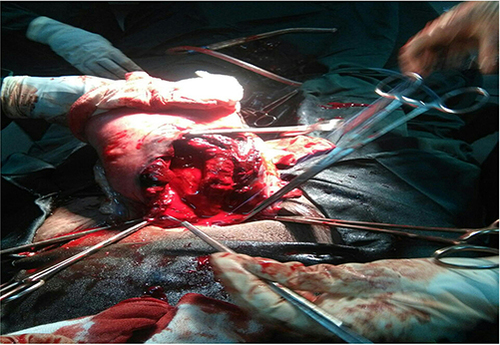
Under general anesthesia, a midline abdominal incision was made after an emergency laparotomy was chosen due to a possible uterine rupture. Overall, 1000 mL of hemoperitoneum, an intact bladder, and an intact anterior uterine wall were all found intraoperatively. A 3.5 kg male alive newborn with Apgar scores of 4, 6, and 8 at the 1st, 5th, and 10th minutes, respectively, was removed from the peritoneal cavity. The infant did not breathe actively, but his heart rate remained above 100 bpm. The bag and mask ventilation method was used twice. The decision on delivery time was 13 min. When the uterus was inspected, the posterior uterine wall on the midline portion ruptured vertically by 12 cm, and there was profuse bleeding but no major blood vessels were involved. The rupture did not extend to the broad ligament or the vagina ().
Figure 1 A photograph showing a 12cm vertical rupture of unscarred posterior uterine wall (August 23, 2022).
The true conjugate was 11 cm, and no congenital uterine anomalies were found. The uterus was then repaired using Vicryl in two interrupted layers, and the hemostasis was secured. The surgery was followed by vaginal exploration to rule out any undetected vaginal extensions. The estimated total blood loss was 1400 mL. The mother received one unit of packed red blood cells intraoperatively, followed by another unit postoperatively. After being resuscitated, the newborn was taken to the neonatal intensive care unit (NICU). The newborn’s HGB level was 16 g/dl. With an HGB of 8.5 g/dl, the mother was stable after surgery. The operating surgeon carefully explained the events, including the timing and mode of delivery.
Once provided with an implanon and once her male baby’s overall status in the NICU had fully improved, the mother was discharged on day 5.
Discussion
With an incidence of 0.5–2.0/10,000, uterine rupture in an unscarred uterus is extremely rare and is mostly limited to laboring multiparas.Citation7 However, there are few occurrences of uterine rupture in primigravid mothers.Citation8,Citation9 According to studies conducted over 13 years with 30,874 deliveries in facilities where high-dose oxytocin augmentation is routine care for primigravidal labor, there was no rupture of the primigravidal uterus during the laboring process.Citation10
Grand multiparty, inappropriate misoprostol/oxytocin use, uterine instruments and manipulation, neglected labor, severe fundal uterine pressure, congenital anomalies of the uterus, and difficult forceps delivery are possible causes of uterine rupture in unscarred or intact uteruses.Citation4,Citation8,Citation11,Citation12 It has been observed that fetal malposition, such as occipitoposterior position and malpresentation with a transverse line, can cause posterior uterine ruptures.Citation8
Clinical manifestations of uterine rupture may include acute or abnormal maternal abdominal pain, tachycardia, vaginal bleeding with shock, loss of uterine contractility, and sometimes blood-tinged urine.Citation4,Citation5,Citation13 Often, the earliest signs of uterine rupture are prolonged, late, or recurring variable decelerations or fetal bradycardias.Citation4,Citation14 Because posterior uterine rupture is so uncommon, typical symptoms might not be present.Citation8
In almost every case, the development of hemorrhagic shock in the patient necessitates immediate laparotomy, urgent resuscitation with rapid infusion of crystalloid solutions, and whole-blood transfusion.Citation15
Perinatal mortality and hypoxic-ischemic encephalopathy associated with uterine rupture occur at rates of 1/20 and 1–2/100, respectively.Citation16 Preventing major fetal morbidity and mortality requires delivering the fetus between 10 and 37 min after uterine rupture.Citation17
Recurrence of uterine rupture after repair ranges from 4% to 19% in subsequent pregnancies.Citation2
One of the rarest case reports that we have not even seen in published literature is posterior uterine wall rupture in primigravid mothers within 3 hr of oxytocin initiation during early labor. In our case, rupture was diagnosed early and a live baby was delivered within 13 min of diagnosis. Considering her parity and site of rupture, the repair was tried and it was successful. This woman had no identifiable risk factors, and we suppose that her posterior uterine rupture may have resulted from an intrinsic impairment in collagen synthesis weakening the connective tissue of the uterine wall. This might be the reason for posterior rupture in early labor.
The lack of a complete investigation into the potential cause of this rare uterine rupture, the unavailability of similar case reports for comparison, and the missing picture of the repaired uterus were the main case-related limitations.
Conclusion
Posterior uterine wall rupture in a primigravid mother with an unscarred uterus is extremely rare. Prompt surgical intervention is mandatory for successful uterine rupture repair as well as favorable newborn outcomes. Therefore, a high index of suspicion should be kept in mind, as conventional warning signs may not be present and the lack of any major risk factors at all is not a guarantee.
Availability of Supporting Data and Materials
All supporting documents have been submitted along with the case report.
Ethics Approval and Consent to Participate
As per our institutional standards, this case report requires patient consent to participate, which has been filed in the patient chart for our records. Research ethics committee approval was not required.
Consent for Publication
Written informed consent was obtained from the patient for publishing this report and the associated photographs. The chief editor of this Journal has access to a copy of the written consent for evaluation.
Author Contributions
All authors made substantial contributions to the conception and design, acquisition of data, or analysis and interpretation of data; took part in either drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
Acknowledgments
The authors would like to thank the staffs of St. Paul’s Hospital, who have been involved in the management of the mother and the neonate.
Additional information
Funding
References
- Dow M, Wax JR, Pinette MG, Blackstone J, Cartin A. Third-trimester uterine rupture without previous cesarean: a case series and review of the literature. Am J Perinatol. 2009;26(10):739–744. doi:10.1055/s-0029-1223287
- Abbas AM, Michael A, Nagy M. A rare case of posterior uterine rupture with neonatal survival during trial of vaginal birth after cesarean section. Proc Obstetr Gynecol. 2017;7(3):1–6.
- Jain A, Tiwari A, Kellogg A. Posterior uterine rupture–A devil with many faces. N Indian J OBGYN. 2017;3:108–110. doi:10.21276/obgyn.2017.3.2.9
- Nanda K, Singh S, Dhama V, Choudhary R, Azad R. A rare case of spontaneous posterior wall rupture in an unscarred uterus during labor. Int J Reprod Contracept Obstetr Gynecol. 2016;6(9):4128.
- Nishikawa S, Shibata T, Kato H, Kotsuji F, Nakago S. Complete rupture of unscarred uterus with delayed symptoms: case report and possible mechanism. J Obstetrics Gynaecol Res. 2020;46(8):1456–1459. doi:10.1111/jog.14261
- Catanzarite V, Cousins L, Dowling D, Daneshmand S. Oxytocin-associated rupture of an unscarred uterus in a primigravida. Obstetr Gynecol. 2006;108(3):723–725. doi:10.1097/01.AOG.0000215559.21051.dc
- Ofir K, Sheiner E, Levy A, Katz M, Mazor M. Uterine rupture: risk factors and pregnancy outcome. Am J Clin Exp Obstet Gynecol. 2003;189(4):1042–1046. doi:10.1067/S0002-9378(03)01052-4
- Navaratnam K, Ulaganathan P, Akhtar M, Sharma S, Davies M. Posterior uterine rupture causing fetal expulsion into the abdominal cavity: a rare case of neonatal survival. Case Rep Obstetr Gynecol. 2011;2011:1–3. doi:10.1155/2011/426127
- Varras M, Akrivis C. Posterior uterine wall rupture of an unscarred gravid uterus at 37 weeks of gestation experience of a rare case with a review of the literature. Am J Case Rep. 2010;11:20–23.
- Cahill DJ, Boylan PC, O’Herlihy C. Does oxytocin augmentation increase perinatal risk in primigravid labor? Am J Clin Exp Obstet Gynecol. 1992;166(3):847–850. doi:10.1016/0002-9378(92)91346-C
- Nikolaou M, Kourea HP, Antonopoulos K, Geronatsiou K, Adonakis G, Decavalas G. Spontaneous uterine rupture in a primigravid woman in the early third trimester attributed to adenomyosis: a case report and review of the literature. J Obstetrics Gynaecol Res. 2013;39(3):727–732. doi:10.1111/j.1447-0756.2012.02042.x
- Walsh CA, Baxi LV. Rupture of the primigravid uterus: a review of the literature. Obstetrical Gynecol Surv. 2007;62(5):327–334. doi:10.1097/01.ogx.0000261643.11301.56
- Hoffman BL, Williams JW. Williams Gynecology. Univerza v Ljubljani, Medicinska fakulteta; 2020.
- Revicky V, Muralidhar A, Mukhopadhyay S, Mahmood T. A case series of uterine rupture: lessons to be learned for future clinical practice. J Obstetr Gynecol India. 2012;62(6):665–673. doi:10.1007/s13224-012-0328-4
- Landon MB. Uterine rupture in primigravid women. Obstetr Gynecol. 2006;108(3):709–710. doi:10.1097/01.AOG.0000236128.43970.aa
- Landon MB, Hauth JC, Leveno KJ, et al. Maternal and perinatal outcomes associated with a trial of labor after prior cesarean delivery. N Engl J Med. 2004;351(25):2581–2589. doi:10.1056/NEJMoa040405
- Qudsia Q, Akhtar Z, Kamran K, Khan AH. Women’s health; uterus rupture, its complications, and management in teaching hospital Bannu, Pakistan. Maedica. 2012;7(1):49.
