Abstract
Objective
To establish and evaluate a nomogram model for predicting the risk of postpartum hemorrhage in second cesarean section.
Methods
A total of 440 parturients who underwent the second cesarean section surgery and were registered in our hospital from August 2019 to July 2021 were selected as the study subjects. They were randomly divided into 220 modeling group and 220 validation group based on simple randomization. The two groups were divided into postpartum hemorrhage group and postpartum non bleeding group according to whether postpartum hemorrhage occurred.
Results
In the modeling group, the incidence of postpartum hemorrhage in the second cesarean section was 15.00%; the Logistic regression model showed that placenta previa, operation time, prenatal anemia, placenta accreta, uterine inertia were the independent risk factors of postpartum hemorrhage in the second cesarean section (P < 0.05). ROC results showed that AUC of predicting the risk of postpartum hemorrhage in the second cesarean section was 0.824. The slope of calibration curve is close to 1, Hosmer-Lemeshow goodness of fit test showed x2= 7.585, P = 0.250. The external verification results show that the AUC is 0.840, and the predicted probability of the calibration curve is close to the actual probability.
Conclusion
Based on the five risk factors of postpartum hemorrhage in the second cesarean section, including placenta previa, operation time, prenatal anemia, placenta accreta and uterine inertia, the nomogram model for predicting the risk of postpartum hemorrhage in the second cesarean section has good accuracy and differentiation.
Cesarean section is currently an important method of childbirth for obstetric women and can save the lives of both mother and baby in critical moments.Citation1 In recent years, with the relaxation of China’s two-child policy, the proportion of women choosing a second cesarean section has been increasing annually, and the incidence of complications following cesarean section is also on the rise.Citation2 Postpartum hemorrhage is the most serious complication during cesarean section and is the leading cause of maternal death.Citation3 Therefore, identifying the risk factors for postpartum hemorrhage after a second cesarean section has significant clinical value. Recent literature indicates that nomogram models play an important role in predicting various clinical adverse events.Citation4,Citation5 In view of this, this study will analyze the clinical data of women undergoing a second cesarean section to explore the influencing factors of postpartum hemorrhage after a second cesarean section. The aim is to establish a nomogram model to predict the risk of postpartum hemorrhage in women undergoing a second cesarean section, which will assist healthcare workers in identifying high-risk pregnant women, thereby reducing the incidence of postpartum hemorrhage in women undergoing a second cesarean section.
Data and Methods
Data
From August 2019 to July 2021, 440 women who were registered in our hospital and underwent the second cesarean section operation were selected as the research objects, and were divided into 220 model group and 220 verification group according to simple randomization method. Modeling group: Ages 22–38 years, gestational weeks 33–42 weeks. Verification group: Age 22–37 years old, gestational weeks 34–42 weeks. The modeling group was divided into a postpartum hemorrhage group (33 cases) and a non-postpartum hemorrhage group (187 cases) based on whether the parturients experienced postpartum hemorrhage. Similarly, the validation group was divided into a postpartum hemorrhage group (31 cases) and a non-postpartum hemorrhage group (189 cases).
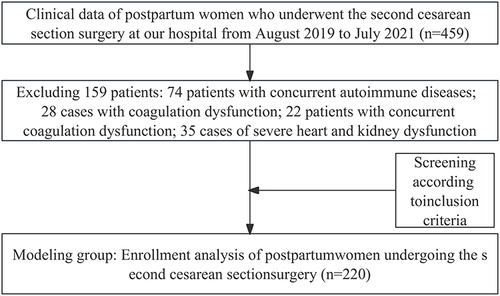
Inclusion criteria: (1) Women undergoing a second cesarean section; (2) Consent for participation in the study was obtained from the parturients and their families, along with a signed consent form; (3) Singleton pregnancy; (4) Complete clinical Data available. Exclusion criteria: (1) Individuals with autoimmune diseases; (2) Those with coagulation disorders; (3) Individuals with severe heart, kidney, or other functional impairments. See .
Methods
A research team was established to determine the research plan and the specific steps to be implemented during the research process. Before data collection, two nurses with over five years of experience in obstetrics and gynecology from our hospital were selected for professional training and briefed on the research purpose and Methods. All clinical data related to the pregnant women involved in this article were collected and organized by the aforementioned nurses. Double entry of all clinical data for the second cesarean section parturients was performed, followed by multiple verifications to ensure the accuracy of the data in this study.
The collected clinical data mainly included: gestational weeks before cesarean section, age, pre-cesarean body mass index (BMI), presence of gestational diabetes, presence of gestational hypertension, time since the last cesarean section, presence of placenta previa, surgery duration, presence of prenatal anemia, placenta accreta, and uterine atony.
Statistical Methods
In this study, all data were processed using the SPSS 22.0 software package. Count data, such as the number of cases with placenta previa and prenatal anemia, were presented in terms of frequency and proportion, and chi-square tests were conducted. Measurement data, like gestational weeks before cesarean section and time since the last cesarean section, were expressed as mean ± standard deviation (), and t-tests were used for intergroup comparisons. For the modeling group, to determine the risk factors for postpartum hemorrhage following a second cesarean section, Logistic regression analysis was utilized. A nomogram model predicting the risk of postpartum hemorrhage after a second cesarean section was constructed using the rms package in R language (R 3.6.3). To assess the discriminative ability of the nomogram model, the receiver operating characteristic (ROC) curve was used. Calibration curves were drawn using the rms package to assess the model’s accuracy. P<0.05 was considered statistically significant.
Results
Comparison of Clinical Data Between Two Groups in the Modeling Group
In the modeling group, the incidence of postpartum hemorrhage in women undergoing a second cesarean section was 15.00%. In the postpartum hemorrhage group, the gestational weeks before cesarean section, age, pre-cesarean BMI, gestational diabetes, gestational hypertension, and time since the last cesarean section showed no significant difference compared to the non-postpartum hemorrhage group (P > 0.05). The number of cases with placenta previa, prenatal anemia, placenta accreta, and uterine atony was higher in the postpartum hemorrhage group compared to the non-postpartum hemorrhage group (P < 0.05). The surgery time was longer in the postpartum hemorrhage group (P < 0.05). See for details.
Table 1 Comparison of Clinical Data Between Two Groups in the Modeling Group()/[n(%)]
Logistic Regression Analysis of the Risk of Postpartum Hemorrhage After a Second Cesarean Section
Using the occurrence of postpartum hemorrhage in women undergoing a second cesarean section (1 = yes, 0 = no) as the dependent variable, and the variables with statistical significance in the above clinical data comparison analysis as independent variables, Logistic regression analysis was performed. The Results of the Logistic regression analysis indicated that placenta previa, surgery time, prenatal anemia, placenta accreta, and uterine atony are independent risk factors for postpartum hemorrhage in women undergoing a second cesarean section (P < 0.05). The final formula obtained was: Z = 2.022 × placenta previa + 0.035 × surgery time + 1.293 × prenatal anemia + 0.994 × placenta accreta + 2.047 × uterine atony - 6.991. See for details.
Table 2 Analysis of Risk Factors for Postpartum Hemorrhage in Pregnant Women Undergoing the Second Cesarean Section
Establishment of the Nomogram Model for Postpartum Hemorrhage After a Second Cesarean Section
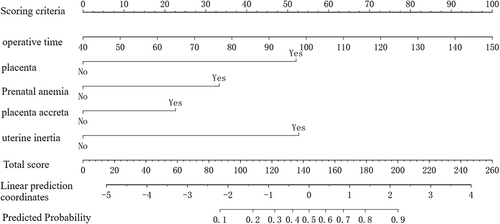
Based on the results of the aforementioned Logistic regression analysis, a nomogram model was created to predict the risk of postpartum hemorrhage following a second cesarean section. The results of the nomogram model indicated that for every 10-minute increase in surgery time, the nomogram model score increased by 9.1 points, with placenta previa scoring 52.1 points, prenatal anemia 32.9 points, placenta accreta 22.6 points, and uterine atony 52.5 points. See for details.
Internal Validation of the Nomogram Model for Postpartum Hemorrhage After a Second Cesarean Section
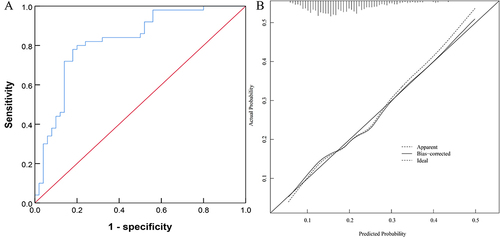
The ROC results showed that the area under the curve (AUC) for predicting the risk of postpartum hemorrhage after a second cesarean section was 0.824 (95% CI: 0.740~0.907), as detailed in . This indicates that the nomogram model has good discriminative ability. The slope of the calibration curve was close to 1, as shown in , and the Hosmer-Lemeshow goodness-of-fit test x2=7.585, P=0.250, indicating good consistency and calibration of the nomogram model.
External Validation of the Nomogram Model for Postpartum Hemorrhage After a Second Cesarean Section
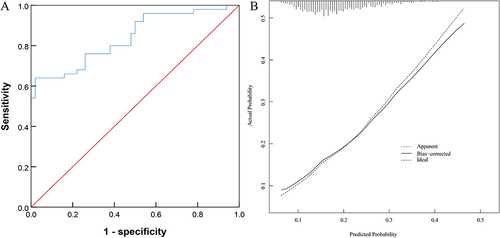
In the validation group, the incidence of postpartum hemorrhage in women undergoing a second cesarean section was 14.09%. The number of cases with placenta previa, prenatal anemia, placenta accreta, and uterine atony in the postpartum hemorrhage group was higher than in the non-postpartum hemorrhage group (P < 0.05), and the surgery time was longer (P < 0.05), as detailed in . External validation of the prediction model was conducted using the data from the validation group. The ROC results showed an AUC of 0.840 (95% CI: 0.762~0.917), as seen in , indicating good discriminative ability of the prediction model. The calibration curve showed that the predicted probabilities closely matched the actual probabilities, demonstrating good consistency of the prediction model, as detailed in .
Table 3 Comparison of Clinical Data Between Two Groups in the Validation Group()/[n(%)]
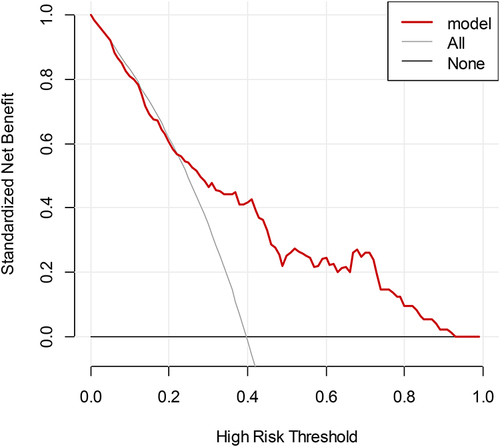
Decision Curve Analysis (DCA) of the Nomogram Model
Using the high-risk threshold probability as the horizontal axis and the net benefit rate as the vertical axis, the clinical utility of applying this nomogram model to predict postpartum hemorrhage after a second cesarean section is higher when the high-risk threshold probability ranges between 0.06 and 0.8. See for details.
Discussion
Postpartum hemorrhage is one of the more urgent conditions that can occur during childbirth, characterized by clinical manifestations such as secondary anemia and vaginal bleeding, which can seriously affect the safety of the mother’s life.Citation6 The risk of postpartum hemorrhage is greatly increased in a second cesarean section due to the increased difficulty and complexity of the surgery, and excessive blood loss can lead to maternal death.Citation7,Citation8 Therefore, exploring the risk factors for postpartum hemorrhage after a second cesarean section is crucial for improving the safety of maternal surgery. Studies show that nomograms, with their unique advantages such as being intuitive and specific, have been widely used in recent years in predicting the risk of adverse clinical events.Citation9–11 In this study, through Logistic regression analysis of the clinical data of women undergoing a second cesarean section, it was found that placenta previa, surgery time, prenatal anemia, placenta accreta, and uterine atony are independent risk factors for postpartum hemorrhage in these women. Based on these five factors, a nomogram model was established to predict postpartum hemorrhage after a second cesarean section. This model can provide valuable references for clinical analysis of various influencing factors on the risk of postpartum hemorrhage in these women, helping to identify high-risk pregnant women, take effective measures, and reduce the incidence of postpartum hemorrhage after a second cesarean section.
Previous studies have shown that placenta previa is one of the risk factors for postpartum hemorrhage in pregnant women.Citation12 Research by DeBolt et alCitation13 found that placenta accreta and placenta previa are independent risk factors for postpartum hemorrhage in parturients. Our study results indicate that placenta accreta and placenta previa are independent risk factors for postpartum hemorrhage in women undergoing a second cesarean section, with placenta accreta contributing 22.6 points and placenta previa 52.1 points in the nomogram model. The likely reason is that placenta accreta can cause damage to the function of uterine smooth muscle, decrease in cell count, leading to uncoordinated uterine contraction, thereby increasing the risk of postpartum hemorrhage. Studies have shown that postpartum hemorrhage in women undergoing cesarean section is associated with prolonged surgery time. Our study results show that surgery time is an independent risk factor for postpartum hemorrhage in women undergoing a second cesarean section, with every 10-minute increase in surgery time adding 9.1 points to the nomogram model score. Coleman et alCitation14 found that uterine atony is an independent risk factor for postpartum hemorrhage in parturients. Our study results indicate that uterine atony is an independent risk factor for postpartum hemorrhage in women undergoing a second cesarean section, contributing 52.5 points in the nomogram model. The possible reason is that uterine atony leads to ineffective compression of blood vessels by uterine muscle fibers, increasing the risk of postpartum hemorrhage. Our study results also show that prenatal anemia is an independent risk factor for postpartum hemorrhage in women undergoing a second cesarean section, contributing 32.9 points in the nomogram model. The likely reason is that prenatal anemia significantly increases the occurrence of uterine atony, thereby increasing the risk of postpartum hemorrhage. Moreover, the internal and external validation results show that the AUC for predicting postpartum hemorrhage risk after a second cesarean section is 0.824 and 0.840, respectively, with the calibration curve’s slope close to 1, and Hosmer-Lemeshow goodness-of-fit test x2= 7.585, P = 0.250, indicating good calibration and discriminative ability of the predictive model. Further, the DCA curve shows that the clinical utility of using this nomogram model to predict postpartum hemorrhage after a second cesarean section is higher when the high-risk threshold probability ranges between 0.06 and 0.8, allowing clinical healthcare workers to predict the risk of postpartum hemorrhage after a second cesarean section based on various factors and intervene early.
In summary, this study, based on five risk factors affecting postpartum hemorrhage in women undergoing a second cesarean section, including placenta previa, surgery time, prenatal anemia, placenta accreta, and uterine atony, has constructed a nomogram model predicting the risk of postpartum hemorrhage after a second cesarean section with good accuracy and discriminative ability. However, this study lacks external validation of the postpartum hemorrhage nomogram, which should be a focus for further in-depth research.
Ethics Approval
This study involving human participants was in accordance with the ethical standards of the Medical Ethics Committee of the Wenzhou Central Hospital and with the 1964 Helsinki Declaration. And obtain the informed consent form of the patient or their guardian, and sign on the informed consent form.
Disclosure
All authors report no conflicts of interest in this work.
Data Sharing Statement
Data and material are available on request from the corresponding author.
References
- Swarnamani K, Smits LS, Palmer K, Mol BW, Davies-Tuck M. Is Cesarean section the right outcome for induction of labor trials? Impact of sample size and primary outcomes. Ultrasound Obstet Gynecol. 2020;56(5):645–646. doi:10.1002/uog.22044
- Farid Mojtahedi M, Sepidarkish M, Almukhtar M, et al. Global incidence of surgical site infections following caesarean section: a systematic review and meta-analysis. J Hosp Infect. 2023;139:82–92. doi:10.1016/j.jhin.2023.05.019
- Obore N, Liuxiao Z, Haomin Y, Yuchen T, Wang L, Hong Y. Intraoperative cell salvage for women at high risk of postpartum hemorrhage during cesarean section: a systematic review and meta-analysis. Reprod Sci. 2022;29(11):3161–3176. doi:10.1007/s43032-021-00824-8
- He C, Zheng F, Lin J, et al. A nomogram to predict the risk of scar pregnancy after caesarean section. J Obstet Gynaecol. 2023;43(1):2142767. doi:10.1080/01443615.2022.2142767
- Li H, Sheng W, Cai M, et al. A predictive nomogram for a failed trial of labor after cesarean: a retrospective cohort study. J Obstet Gynaecol Res. 2022;48(11):2798–2806. doi:10.1111/jog.15398
- Wei Q, Xu Y, Zhang L. Towards a universal definition of postpartum hemorrhage: retrospective analysis of Chinese women after vaginal delivery or cesarean section: a case-control study. Medicine. 2020;99(33):e21714. doi:10.1097/MD.0000000000021714
- Vitner D, Bleicher I, Levy E, et al. Differences in outcomes between cesarean section in the second versus the first stages of labor. J Matern Fetal Neona. 2019;32(15):2539–2542. doi:10.1080/14767058.2018.1440545
- Lauterbach R, Justman N, Ginsberg Y, et al. The impact of extending the second stage of labor on repeat cesarean section and maternal and neonatal outcome. Int J Gynaecol Obstet. 2023;163(2):594–600. doi:10.1002/ijgo.14855
- Zhou H, Gu N, Yang Y, Wang Z, Hu Y, Dai Y. Nomogram predicting cesarean delivery undergoing induction of labor among high-risk nulliparous women at term: a retrospective study. BMC Preg Childbirth. 2022;22(1):55. doi:10.1186/s12884-022-04386-8
- Chen B, Zhang L, Wang D, et al. Nomogram to predict postpartum hemorrhage in cesarean delivery for women with scarred uterus: a retrospective cohort study in China. J Obstet Gynaecol Res. 2020;46(9):1772–1782. doi:10.1111/jog.14354
- Wang Y, Xiao J, Hong F. A risk prediction model of perinatal blood transfusion for patients who underwent cesarean section: a case control study. BMC Preg Childbirth. 2022;22(1):373. doi:10.1186/s12884-022-04696-x
- Dang X, Fan C, Cui F, et al. Interactions between ultrasonographic cervical length and placenta accreta spectrum on severe postpartum hemorrhage in women with placenta previa. Int J Gynaecol Obstet. 2023;161(3):1069–1074. doi:10.1002/ijgo.14641
- DeBolt CA, Rosenberg HM, Pruzan A, et al. Patients with resolution of low-lying placenta and placenta previa remain at increased risk of postpartum hemorrhage. Ultrasound Obstet Gynecol. 2022;60(1):103–108. doi:10.1002/uog.24825
- Coleman JR, Fabbri S, Anderson M, et al. Beyond uterine atony: characterizing postpartum hemorrhage coagulopathy. Am J Obstet Gynecol MFM. 2023;5(3):100822. doi:10.1016/j.ajogmf.2022.100822