Abstract
Purpose
To verify whether there is lower incidence of adverse pregnancy outcomes after high-intensity focused ultrasound (HIFU) treatment than loop electrosurgical excision procedure (LEEP) in young women of childbearing age.
Patients and Methods
This retrospective cohort study enrolled 46 patients treated with HIFU and 46 patients treated with LEEP. To compare the differences between the two groups, Fisher’s exact test or the Kruskal–Wallis (K-W/H) test was used in the univariate analysis, while the logistic regression method was applied for further verification.
Results
Basic characteristics showed no differences between the two groups (P > 0.05) except for parity (P < 0.001). Preterm birth rates were 6.52% and 0.00% in patients with cervical high-grade squamous intraepithelial lesions (HSIL) treated with LEEP and HIFU, respectively. The incidence rates of premature rupture of membranes (PROM) were respectively 15.22% and 21.74% in the two groups. There was no significant difference in pregnancy outcomes between the two groups (P > 0.05).
Conclusion
This study is the first to compare the pregnancy outcomes of patients with cervical HSIL who treated with LEEP and HIFU procedures. Both HIFU treatment and LEEP are available options for patients of reproductive age with cervical HSIL. Therefore, it is necessary to conduct prospective single-center or multicenter randomized controlled studies.
Introduction
According to the fifth edition of the WHO Classification of Female Genital Tumors, cervical squamous intraepithelial lesions are classified into two categories, low-grade squamous intraepithelial lesion (LSIL), and high-grade squamous intraepithelial lesion (HSIL). The former is equivalent to cervical intraepithelial neoplasia, grade I (CIN I), while the latter includes CIN II and CIN III.Citation1 In the past few decades, owing to the popularization of cervical cancer screening strategies and the application of the human papilloma virus (HPV) vaccine, the incidence and mortality of cervical cancer have gradually decreased, however, the age of patients suffering from cervical cancer was trending younger.Citation2,Citation3 Extensive researches showed that persistent HPV positivity after treatment would increase the recurrence rate of HSIL,Citation4–6 which could be significantly reduced by HPV vaccination.Citation7–10 As recommended by 2019 American Society for Colposcopy and Cervical Pathology (ASCCP) Risk-Based Management Consensus Guidelines for Abnormal Cervical Cancer Screening Tests and Cancer Precursors, the preferred treatment for HSIL is excisional therapy, including loop electrosurgical excision procedure (LEEP) and cold knife conization (CKC), besides, treatment with ablation can also be acceptable.Citation11 Each of these treatment options has advantages and disadvantages. LEEP has the benefit of decreasing bleeding during the operation and providing histological specimens, which are available to determine whether there are higher grade lesions and provide information on the margin status. However, it reduces the quality of surgical margins to a certain extent, which may influence the accuracy of pathological diagnosis. After treatment with LEEP, cervical incompetence may occur, resulting in an increased risk of miscarriage, premature delivery, preterm premature rupture of membranes (PPROM), and premature rupture of membranes (PROM).Citation12,Citation13 In comparison, cone depth in CKC is longer, and the amount of bleeding during operation is more, which is considered to be connected with increased incidence of preterm delivery and PROM.Citation14,Citation15 The advantage of CKC lies in providing a complete pathological specimen and a high-quality margin status. Ablative therapies, such as high-intensity focused ultrasound (HIFU) treatment, offer advantages such as less traumatic, quick recovery, and low cost without anesthesia and hospitalization. HIFU technology has widely employed in gynecological diseases, such as uterine leiomyomas, adenomyosis, cervicitis and vulvar diseases based on the thermal effect, which locally focused on targeted site.Citation16,Citation17 Yujuan Liu et al reported that HIFU was a safe and effective therapeutic option for cervical HSIL patients with fertility requirement.Citation18 HIFU treatment selectively destroys cervical lesions and keeps the anatomical structure of cervical tissues intact, which seems to reduce the occurrence of the above adverse pregnancy outcomes. Due to the shallow treatment depth, lesions of deep cervix and cervical canal could not be removed. Therefore, the indications and contraindications should be strictly controlled for patients with HSIL. In young women of childbearing age with cervical HSIL, it is particularly important to reduce the risk of disease progression while avoiding adverse pregnancy outcomes. There is currently no study compares the safety and efficacy of LEEP and HIFU treatment for patients with cervical HSIL. Thus, this retrospective cohort study aimed to analyze the differences in pregnancy outcomes after treatment of HIFU and LEEP in patients with cervical HSIL, and to analyze the possible factors influencing these outcomes so as to provide reasonable management recommendations for women of reproductive age.
Materials and Methods
Clinical Study Design and Patients
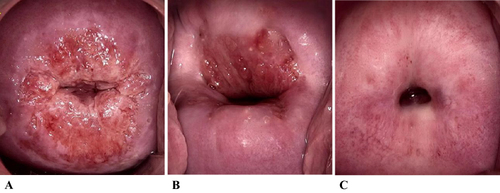
The inclusion criteria were as follows: (1) women who underwent adequate colposcopic examination and had a visible type 1 transformation zone (TZ), as shown in . Adequate for the reason that the examined area was completely and fully exposed, including the complete TZ and lesions, without any inflammation, bleeding or scarring. Type 1, 2, 3 TZ were defined as completely visible, partially visible and invisible squamocolumnar junction, respectively.Citation19 Histopathological examination identified cervical HSIL and was negative for intraepithelial lesions and malignancy of endocervical curettage (ECC) pathology. (2) women had body mass index (BMI) between 18.5 and 30 kg/m2, age between 18 and 40 years old and parity less than or equal to 2, no history of other cervical surgery or cervical laceration. (3) there was no history of preterm birth or late abortions, and no complications of pregnancy this time. (4) no addiction to tobacco or alcohol, and no history of drug abuse.
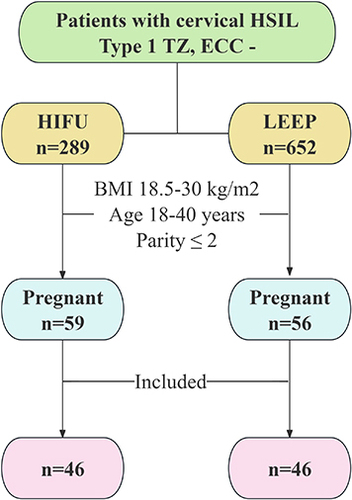
In this retrospective cohort study, among the cervical HSIL patients with type 1 TZ and negative ECC pathological results treated at the Women and Children’s Hospital, School of Medicine, Xiamen University between 2017 and 2021, there were 289 and 652 patients treated with HIFU and LEEP, respectively. Among women with BMI between 18.5 and 30 kg/m2, age between 18 and 40 years old and parity less than or equal to 2, there were, respectively, 59 and 56 patients got pregnant after HIFU treatment and LEEP. Based on other inclusion criteria, 46 patients treated with HIFU and 46 patients treated with LEEP were enrolled in this study, and those who failed to meet the inclusion criteria were excluded ().
Figure 2 Flowchart of patients included in the study.
The follow-up cutoff time was December 2023. All the clinical records were anonymized. This study was approved by the Ethical Committee of the Women and Children’s Hospital, School of Medicine, Xiamen University, Xiamen, China. Because the informed consent process had been provided before treatment and the retrospective study analyzed the clinical history data of patients, written informed consent was formally waived.
Evaluations Before Treatment
All patients underwent evaluations consisting of a detailed medical history, especially a history of menstrual pattern and reproductive history, as well as clinical examinations, routine blood, and vaginal secretion determination. All the patients underwent therapeutic procedures 3–7 days after their menstrual period and were not pregnant. The size of the cervical lesions was confirmed using Schiller’s test.
High-Intensity Focused Ultrasound
A Seapostar ultrasound therapy device (Chongqing Haifu Technology Co. Ltd, Chongqing, China) was used in this study. According to the tutorial, ultrasound energy was produced by a 10-mm-diameter focused ultrasound transducer with a focal length of 4 mm, operating at frequencies of 8–12 MHz, and the acoustic power was 3.5–4.5 W. The handheld ultrasound transducer, which was completely enveloped in a disposable metal cover, was placed in direct close contact with the cervix using a coupling medium. Keeping circular scanning from lesions to over 2 mm normal area surrounding the lesion at speed of 2–5mm/s. The treatment was terminated immediately when the local tissue became dented, hardened, whitened with wrinkled and well-demarcated original squamous columnar junction.
Loop Electrosurgical Excision Procedure
LEEP was performed using the Ellman Surgitron F.F.P.F. EMC device (Ellman International, Inc). The cone circumference was >5 mm outside the lesions and the cone length was 7–10 mm choosing an adequately shaped loop electrode.
Statistical Analysis
The SPSS software for Windows (version 22.0, IBM Corporation, Armonk, NY, USA) was used in this study. Owing to the different methods of statistical descriptions, all the data were divided into categorical data and quantitative data. The normal test of continuous variables was performed using the Kolmogorov–Smirnov Z test. Continuous data fit the normal distribution were described as mean ± SD (standard deviation), on the contrary, as median (interquartile range/IQR). Categorical data were described as frequencies and percentages. To compare the differences between the two groups, Fisher’s exact test or the Kruskal–Wallis (K-W/H) test was used in the univariate analysis, while the logistic regression method was applied for further verification and correction of confounding factors. Statistical significance was set at P < 0.05.
Results
Baseline Characteristics
The basic characteristics including age, height, pre-pregnancy weight, weight gain during pregnancy, BMI pre-delivery, interval from post-treatment to delivery, gravidity, parity, and grade of CIN, showed no differences between the two groups (P > 0.05) except for parity (P < 0.001). For patients treated with LEEP and HIFU procedures, the ages ranged from 25 to 40 years and 20 to 40 years, respectively, and the mean age of those patients was respectively 30.54±3.59 years and 29.09±3.64 years. Before treatment, 78 patients (84.78%) were diagnosed with CIN II and 14 patients (15.22%) were diagnosed with CIN III ().
Table 1 Baseline Clinical Features and Univariate Correlation Analysis
The Impact on Preterm Outcome
As shown in , the preterm birth rate was 6.52% in cervical HSIL patient treated with LEEP, and no children were born prematurely in the HIFU group. However, there was no significant difference in preterm outcomes between the two groups (P > 0.05). After correcting for confounding factors, no statistically significant differences were observed (P = 0.070). All basic characteristics, including age, height, pre-pregnancy weight, weight gain during pregnancy, BMI pre-delivery, interval from post-treatment to delivery, gravidity, parity, and grade of CIN showed no difference (P > 0.05) ().
Table 2 Multivariate Logistic Analysis of the Differences in Preterm Outcome (P = 0.070)
The Impact on PROM Outcome
No difference was found in PROM outcomes between patients treated with LEEP and HIFU procedure, as shown in (P > 0.05), the incidence rates of PROM were 15.22% and 21.74% respectively. Similarly, the groups showed no significant differences after correcting for confounding factors by multivariate logistic analysis (P = 0.179), which did not show statistical differences in any of the basic characteristics, including age, height, pre-pregnancy weight, weight gain during pregnancy, BMI pre-delivery, interval from post-treatment to delivery, gravidity, parity, and grade of CIN (P > 0.05) ().
Table 3 Multivariate Logistic Analysis of the Differences in PROM Outcome (P = 0.179)
Discussion
Principal Findings
The main findings of this retrospective cohort study were as follows: (1) Nulliparous patients tended to choose high-intensity focused ultrasound treatment. (2) There was no significant difference in the incidence rate of preterm birth and PROM in cervical HSIL patients treated with LEEP and HIFU procedures. That is, for women with cervical HSIL of reproductive age, both treatment with LEEP and HIFU are available options, but if the latter, the indications and contraindications are rigorous. As recommended by the ASCCP and WHO, LEEP is preferred and treatment with ablation is acceptable.Citation11,Citation20
A retrospective cohort study including 65,527 women with cervical HSIL found that the rates of histopathological recurrence and virological clearance were similar in patients treated with LEEP and ablation, however, LEEP was associated with more complications including preterm birth, infection, and bleeding.Citation21 Ablative therapies have selective effects on pathologically altered tissues, which preserve the normal anatomical and functional characteristics of the cervix. Several studies have shown that treatment with ablation has no significant adverse effects on pregnancy outcomes, including preterm birth and PROM.Citation22,Citation23 Although it is important to protect fertility, reducing the persistence or recurrence of precancerous lesions is equally important. Some research suggests that persistence of HPV infection and positive endocervical margins are risk factors for the persistence or recurrence of CIN, and there is no significant association with the type of therapy.Citation24,Citation25 As mentioned before, the indications for HIFU therapy are strictly controlled, it is not suitable for cervical HSIL patients with ECC-positive biopsy and type 2 or 3 transformation zone, who should adopt more active treatment, and the conization depth should be properly increased to prevent positive postoperative margins.Citation26
Strengths and Limitations
High-intensity focused ultrasound (HIFU) treatment is an ablation therapy. Our study compared the pregnancy outcomes of patients with cervical HSIL treated with LEEP and HIFU for the first time. In addition, the inclusion criteria were rigorous to eliminate other possible influences. Our study had an important limitation, it was a retrospective study with a small sample sizes, which is probably why the results did not show a statistical difference. For further verification, it is necessary to conduct a prospective single-center or multicenter randomized controlled study.
Conclusions
In summary, for cervical HSIL patients of reproductive age who met the rigorous criteria, the incidence rate of adverse pregnancy outcomes after both high-intensity focused ultrasound (HIFU) treatment and loop electrosurgical excision procedure (LEEP) were not significantly different. In other words, both types of therapeutic regimens were available. However, further studies are required to provide a more accurate basis for selection.
Abbreviation
HIFU, High-Intensity Focused Ultrasound; LEEP, loop electrosurgical excision procedure; HSIL, high-grade squamous intraepithelial lesion; LSIL, low-grade squamous intraepithelial lesion; CIN, cervical squamous intraepithelial lesion; HPV, human papilloma virus; CKC, cold knife conization; PROM, premature rupture of membrane; PPROM, preterm premature rupture of membranes; TZ, transformation zone; ECC, endocervical curettage; BMI, body mass index; SD, standard deviation; IQR, interquartile range.
Ethics Approval
This study complies with the Declaration of Helsinki, which was approved by the Ethical Committee of the Women and Children’s Hospital, School of Medicine, Xiamen University, Xiamen, China.(Approval No.KY-2024-005-K01)
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas: took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgment
Xiao-Ling Shen and Zhuo-Yi Li are co-first authors for this study. The authors acknowledge the case management system in the medical record room of Women and Children’s Hospital, School of Medicine, Xiamen University, for providing substantial clinical data for the included patients.
Additional information
Funding
References
- WHO Classification of Tumours Editorial Board. WHO classification of tumours. In: Female Genital Tumours. 5th. Lyon: IARC Press; 2020:1–632.
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
- Singh D, Vignat J, Lorenzoni V, et al. Global estimates of incidence and mortality of cervical cancer in 2020: a baseline analysis of the WHO Global Cervical Cancer Elimination Initiative. Lancet Glob Health. 2023;11(2):e197–e206. doi:10.1016/S2214-109X(22)00501-0
- Fan A, Wang C, Han C, Wang Y, Xue F, Zhang L. Factors affecting residual/recurrent cervical intraepithelial neoplasia after cervical conization with negative margins. J Med Virol. 2018;90(9):1541–1548. doi:10.1002/jmv.25208
- Zang L, Hu Y. Risk factors associated with HPV persistence after conization in high-grade squamous intraepithelial lesion. Arch Gynecol Obstet. 2021;304(6):1409–1416. doi:10.1007/s00404-021-06217-1
- Bogani G, Sopracordevole F, Ciavattini A, et al. HPV persistence after cervical surgical excision of high-grade cervical lesions. Cancer Cytopathol. 2024;132(5):268–269. doi:10.1002/cncy.22760
- Bogani G, Raspagliesi F, Sopracordevole F, et al. Assessing the long-term role of vaccination against HPV after loop electrosurgical excision procedure (LEEP): a propensity-score matched comparison. Vaccines. 2020;8(4):717. doi:10.3390/vaccines8040717
- Kechagias KS, Kalliala I, Bowden SJ, et al. Role of human papillomavirus (HPV) vaccination on HPV infection and recurrence of HPV related disease after local surgical treatment: systematic review and meta-analysis. BMJ. 2022;378:e070135. doi:10.1136/bmj-2022-070135
- Eriksen DO, Jensen PT, Schroll JB, Hammer A. Human papillomavirus vaccination in women undergoing excisional treatment for cervical intraepithelial neoplasia and subsequent risk of recurrence: a systematic review and meta-analysis. Acta Obstet Gynecol Scand. 2022;101(6):597–607. doi:10.1111/aogs.14359
- Dvorak V, Petras M, Dvorak V, et al. Reduced risk of CIN2+ recurrence in women immunized with a 9-valent HPV vaccine post-excision: retrospective cohort study. Hum Vaccin Immunother. 2024;20(1):2343552. doi:10.1080/21645515.2024.2343552
- Perkins RB, Guido RS, Castle PE, et al. 2019 ASCCP risk-based management consensus guidelines for abnormal cervical cancer screening tests and cancer precursors. J Low Genit Tract Dis. 2020;24(2):102–131. doi:10.1097/LGT.0000000000000525
- Kacerovsky M, Musilova I, Baresova S, Kolarova K, Sengpiel V, Jacobsson B. Cervical excisional treatment increases the risk of intraamniotic infection in subsequent pregnancy complicated by preterm prelabor rupture of membranes. Am J Obstet Gynecol. 2023;229(1):51e51–51e13. doi:10.1016/j.ajog.2022.12.316
- Maina G, Ribaldone R, Danese S, Lombardo V. Obstetric outcomes in patients who have undergone excisional treatment for high-grade cervical squamous intra-epithelial neoplasia. Eur J Obstet Gynecol Reprod Biol. 2019;236:210–213. doi:10.1016/j.ejogrb.2019.02.025
- Obut M, Iskender CT, Kindan A, et al. Factors affecting obstetric outcomes in patients who underwent cold-knife and loop electrosurgical excision procedure conization due to CIN 2 or CIN 3. J Turk Ger Gynecol Assoc. 2023. doi:10.4274/jtgga.galenos.2023.2023-1-15
- Gao Y, Wang H, Xiao Y. The effect of cold-knife conization on pregnancy outcomes in patients with cervical lesions. PLoS One. 2022;17(12):e0278505. doi:10.1371/journal.pone.0278505
- Zhang L, Wang Z, Wang Z, Wang Z, Wang Z. Ultrasound-guided high intensity focused ultrasound for the treatment of gynaecological diseases: a review of safety and efficacy. Int J Hyperthermia. 2015;31(3):280–284. doi:10.3109/02656736.2014.996790
- Zhang X, He N, Zhang L, et al. Application of high intensity focused ultrasound combined with nanomaterials in anti-tumor therapy. Drug Deliv. 2024;31(1):2342844. doi:10.1080/10717544.2024.2342844
- Liu Y, Wang W, Zhang M, et al. High-intensity focused ultrasound for patients with cervical intraepithelial neoplasia 2/3: a prospective one-arm study. Ultrasound Med Biol. 2023;49(1):375–379. doi:10.1016/j.ultrasmedbio.2022.09.020
- Bosze P, Girardi F, Haefner H. 2011 colposcopic terminology of the international federation for cervical pathology and colposcopy. Obstet Gynecol. 2012;120(1):166–172. doi:10.1097/AOG.0b013e318254f90c
- WHO guidelines: use of cryotherapy for cervical intraepithelial neoplasia. Geneva: World Health Organization; 2011. Available from: http://www.ncbi.nlm.nih.gov/books/NBK138476/. Accessed July 26, 2024.
- Hughes KC, Herring TA, Song JN, et al. Cervical high-grade squamous intraepithelial lesion burden and standard of care treatment effectiveness and safety in the United States, 2008–2018: the each-woman project. J Low Genit Tract Dis. 2023;27(2):105–112. doi:10.1097/LGT.0000000000000719
- Samoilova S, Petukhova N, Efendiev K, et al. Analysis of the results of severe intraepithelial squamous cell lesions and preinvasive cervical cancer phototheranostics in women of reproductive age. Biomedicines. 2022;10(10):2521.
- Yao Y, Wang W, Liu Y. Efficacy and pregnancy outcomes of focused ultrasound for cervical high-grade squamous intraepithelial lesions. Int J Hyperthermia. 2023;40(1):2250936. doi:10.1080/02656736.2023.2250936
- Bittencourt DD, Zanine RM, Sebastiao APM, Ribas CM. Risk factors for persistence or recurrence of high-grade cervical squamous intraepithelial lesions. Rev Col Bras Cir. 2023;50:e20233537. doi:10.1590/0100-6991e-20233537-en
- Durand N, Ghorab Z, Gien LT, Osborne R, Vicus D, Kupets R. Role of HPV in the prediction of persistence/recurrence after treatment for cervical precancer. J Obstet Gynaecol Can. 2023;45(10):102171. doi:10.1016/j.jogc.2023.06.006
- Sijing L, Ying J, Jing W, Xiaoge L, Ming L, Zhaoning D. Additional role of ECC in the detection and treatment of cervical HSIL. Front Med. 2023;10:1206856. doi:10.3389/fmed.2023.1206856