Abstract
Background
The purpose of this study was to explore the relationship between infertility-related stress and dyadic coping with quality of life (QoL) in couples with infertility issues, and verify gender differences and dyadic interactions in the associations between them.
Methods
This cross-sectional study included 340 couples who were recruited from the First Affiliated Hospital of Lanzhou University between March 2022 and November 2022. The Fertility Problem Inventory, Dyadic Coping Inventory and FertiQoL were used to measure infertility-related stress, dyadic coping and QoL. The Actor-Partner Interdependence Model was used to analyze the effects of infertility-related stress and dyadic coping on the couple’s own QoL (actor effect) as well as on their partner’s QoL (partner effect).
Results
Female patients perceived significantly lower levels of QoL and dyadic coping than those of husbands. There was no statistically significant difference in the infertility-related stress between wives and husbands. Husbands’ infertility-related stress had actor and partner effects on their own and their wives’ QoL, while wives’ infertility-related stress only had an actor effect on their own QoL. Husbands’ dyadic coping had both actor effect and partner effects on their own and their wives’ QoL, meanwhile wives’ dyadic coping had both actor effect and partner effects on their own and their husbands’ QoL.
Conclusion
Husbands’ QoL was impacted by their own infertility-related stress, dyadic coping and their wives’ dyadic coping. Whereas wives’ QoL was influenced by infertility-related stress and dyadic coping from both their own and their spouses. Therefore, elevating the level of dyadic coping may contribute to improving QoL for both husbands and wives. Moreover, enhancing the ability to cope with infertility-related stress might be useful for husbands and indirectly contribute to wives’ QoL.
Introduction
Infertility refers to the inability to conceive after at least one year of regular unprotected intercourse. It is a reproductive dysfunction in women of childbearing age.Citation1 The prevalence of infertility among women in developed countries ranges from 3.5% to 16.7%, while in developing countries, it ranges from 6.9% to 9.3%.Citation2 In China, the prevalence of infertility is estimated to be between 10.5% and 26.9%.Citation3 Globally, the incidence of female infertility increases by 0.370% annually, while male infertility increases by 0.291% annually.Citation4 The global prevalence and burden of infertility have been continuously rising, making it a significant public health concern worldwide. Infertility is a distressing experience for affected couples, and the long duration of the disease and repeated Assisted Reproductive Technology (ART) treatments can lead to a decrease in their satisfaction with quality of life, imposing a heavy burden on individuals, families, and society.Citation5
Quality of life (QoL), as a multidimensional concept, can comprehensively reflect the individual’s evaluation of their psychological, physical, social, and environmental perception in events that pose a threat to their health.Citation6 Previous studies have confirmed the close relationship between improving QoL with increased pregnancy rates and assisted reproductive outcomes.Citation7 Therefore, the QoL of infertility patients is considered by researchers to be equally important as treatment.Citation8 However, women’s QoL is worse than that of their male partners. They score lower on emotional and physical reactions compared to men.Citation9 Compared to men, women experience a higher level of negative emotional distress.Citation10 Additionally, women experience a higher sense of social isolation and social disorders compared to men.Citation11 About 76.8% of infertile women have experienced violence, which is closely related to the quality of their marital relationships.Citation12
Pregnancy concerns both partners in a marriage, and besides the patient themselves, spouses also experience fertility-related stress with gender differences and mutual influence.Citation13 The adverse impact of infertility-related stress on the patient’s QoL and family relationships has been confirmed.Citation14 Previous research has primarily analyzed the correlation between stress and QoL in infertility patients at the individual level, but there have been few reports on their mutual influence in the family environment where couples live together. Currently, research on the factors influencing the QoL of couple with infertility issues has focused on their individual characteristics including socio-demographic information, personality traits, personal coping, mental health.Citation5,Citation8,Citation15 In contrast, the impact of differences in couples’ coping styles on each other’s QoL has not received enough attention, and even fewer studies have explored the factors influencing the QoL of couples as a whole. Fertility is an event that couples experience together, and the perceived stressors may be consistent and interact with each other.Citation16 Prior studies have ignored the interactions and differences between spouses’ QoL and patients’ QoL.Citation17 Studies on women or men alone could not fully understand the important role played by their spouses. Therefore, it is necessary to further explore the interactive effects that the stress experienced by both patients and their spouses may have on each other’s QoL.
The Transactional Stress and Coping Model (TSCM) posits that the coping strategies individuals employ after perceiving stress have a significant impact on health outcomes.Citation18 TSCM has been demonstrated to be a valuable predictor of health for individuals in various stress contexts, such as those with chronic illnesses and cancer.Citation19,Citation20 Therefore, this study employs TSCM as a theoretical framework to investigate the impact of infertility-related stress on the fertility QoL among couples.
Family, as the primary living environment of patient’s, the emotions, attitudes, and behaviors of spouse can potentially impact the patient’s recovery and QoL. Dyadic Coping (DC) is a form of stress management within a marriage that emphasizes the interdependence of the stress experiences of both spouses.Citation21 Infertility, as a stressor deeply rooted in the marital relationship, is influenced not only by individual differences but also by the dynamics of the specific couple’s relationship. The coping strategies of both spouses can potentially influence each other.Citation22 Research indicates that when couples engage in mutual coping, they can create a supportive environment for each other, which can enhance treatment outcomes, ultimately improving their QoL.Citation23 Thus, it is evident that when both partners perceive support and encouragement from each other facing with infertility, it can foster a positive cycle of behavior. Therefore, this study aims to focus on dyadic coping variables at the marital level to explain the impact of infertility-related stress and coping strategies on the QoL among both spouses.
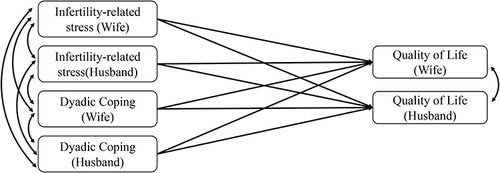
The predictive role of stress on the QoL among infertile women has been extensively studied and validated, but the stress of the spouse and the interaction between spouses have been less reported. Therefore, our study explores the relationships between couples’ stress, coping, and QoL. The hypotheses of this study are listed as follows: (a) Infertility-related stress would be associated with the couple’s own QoL as well as their spouse’s QoL. (b) Dyadic coping would be associated with the couple’s own QoL as well as their spouse’s QoL ().
Materials and Methods
Participants and Recruitment
A total of 340 couples who sought assisted reproductive assistance at the Reproductive Center of Lanzhou University First Hospital between March 2022 and November 2022 were included in this study and convenience sampling was adopted. The study was approved by the ethics committee of the Nursing School, Lanzhou University, Lanzhou, China (LZUHLXY20210053). This study complied with the Declaration of Helsinki. The written informed consents were obtained from participants. The inclusion criteria for wives were: (1) clinical diagnosis of infertility, (2) awareness of the disease condition and provision of informed consent, and (3) normal language communication ability and voluntary participation. The inclusion criteria for husbands were: (1) awareness of the patient’s condition and normal communication ability, (2) provision of informed consent, and (3) absence of male infertility factors. Exclusion criteria included: (1) previous history of diagnosed mental disorders or use of antidepressants in the past 6 months, and (2) presence of other serious physical illnesses or major life stress events in the past 6 months.
In this study, the number of observed variables in the model was used to estimate the sample size, and the ratio of sample size to observed variables was at least 10:1.Citation24 A total of 20 variables were included in this study, including 11 variables of general data (age, education level, etc)., 9 measurements of FertiQoL, infertility-related stress and dyadic coping. The calculated number of subjects was not less than 200 couples.
The survey team consisted of two trained investigators, including the author. They provided couples with standardized instructions and requirements for completing the questionnaires. All surveys were conducted with the full awareness of the attending physician and the couples. Surveys were conducted face-to-face, and both partners independently completed the questionnaires, which were later coded and collected by investigators. We conducted on-site checks to ensure completeness. Samples with missing key indicators and outliers were removed during data organization. For example, only one partner filled out the questionnaire, both partners completed the questionnaire but there were issues such as incomplete responses or consistently selecting the same option, or there were patterns in the responses. For the data with missing information < 30% of the data was imputed by multiple imputation.
Measures
Fertility Quality of Life Questionnaire (FertiQoL)
The FertiQoL is an international tool developed by European Society of Human Reproduction and Embryology (ESHRE) and American Society for Reproductive Medicine (ASRM) specifically focusing on QoL related to infertility.Citation25 It has been validated in multiple countries and translated into various languages. The questionnaire consists of two main sections: the Core FertiQoL and the Treatment FertiQoL, comprising a total of 36 items. The Core FertiQoL includes 24 items organized into four domains: emotional domain, mind/body domain, relationship domain, social domain. The treatment FertiQoL consists of two items related to treatment environment and treatment tolerance, designed to evaluate patients’ thoughts and feelings directly related to fertility treatment, including 10 items in total. Each item is scored on a scale of 0–4 points (with 5 levels), where a higher score indicates a better QoL. In our study, the Cronbach’s α of male sample and female sample were 0.822, and 0.802.
Fertility Problem Inventory (FPI)
The FPI was developed in Canada in 1999 and is specifically designed to assess fertility-related stress.Citation26 The Mandarin version of the Fertility Problem Inventory (M-FPI) was translated by Peng et al.Citation27 It consists of 46 items organized into five dimensions: Social concern, Sexual concern, Relationship concern, Need for parenthood, and Rejection of childless lifestyle. Each item is rated on a Likert-6 scale, ranging from 1 to 6 points, where 1 indicates complete disagreement and 6 indicates complete agreement. The total score on the M-FPI can range from 46 to 276 points, with higher scores indicating higher levels of fertility-related stress. The internal consistency reliability of the questionnaire is assessed using Cronbach’s α coefficient in our study, with an overall value of male sample and female sample were 0.907, and 0.891, and sub-dimensions including Social concern at 0.74, Sexual concern at 0.71, Relationship concern at 0.70, Need for parenthood at 0.75, and Rejection of childless lifestyle 0.71. These values indicate good internal consistency and reliability for the M-FPI questionnaire.
Dyadic Coping Inventory (DCI)
The DIC is a questionnaire designed to measure dyadic coping in one or both partners in an intimate relationship under stressful conditions. The inventory consists of 37 items. The DCI includes 6 dimensions: stress communication, supportive coping, delegated coping, joint coping, negative coping, and coping quality evaluation. According to the Systemic Transactional Model (STM) by Bodenmann,Citation28,Citation29 DC refers to the positive and negative strategies, namely positive and negative DC.Citation28,Citation30 Positive DC includes open communication, and supportive, delegated, and common DC.Citation28,Citation30 The questionnaire is scored using a Likert-5 scale, with ratings ranging from 1 (very rare) to 5 (very frequent). It’s important to note that negative coping support is reverse-scored, and two items related to coping quality evaluation are not included in the total score. The scoring interpretation typically ranges from 35 to 175, where higher scores indicate a greater presence of supportive coping behaviors in the couple and a better dyadic coping situation. The Chinese version of the questionnaire has demonstrated good internal consistency among infertility patients, with a Cronbach’s α coefficient of 0.881.Citation31 In our study, the Cronbach’s α of male sample and female sample were 0.939, and 0.845.
Demographic and Infertility-Related Information
The general information questionnaire for couples with infertility includes age, occupation, educational level, place of residence, birth history, per capita monthly income of the family, infertility years, marriage age, marital type, assisted pregnancy cycle, infertility type, and family type.
Data Analysis
The data were analyzed using SPSS 25.0 and Amos 26.0. P<0.05 is considered statistically significant. The data of this study conform to normal distribution, the quantitative data were expressed by means, standard deviation, and the qualitative data were statistically described by frequencies and percentage. Paired sample t-tests were used to compare the scores of various dimensions of dyadic coping, fertility-related stress, and QoL in couples, employing R 4.1.3 and “pwr” package for power analysis. Pearson correlation analysis was used to analyze the correlation between all variables. The Actor-Partner Interdependence Model (APIM) is widely used for studying the interdependence between members of dyadic members while simultaneously estimating the influence of individual and partner characteristics on outcome variables.Citation32 Amos 26.0 was applied to construct APIM to analysis the relationship between dyadic coping, fertility-related stress, and QoL in couples with infertility issues, and to examine the actor effect and partner effect.
Results
Preliminary Analyses
A total of 340 couples experiencing infertility completed the survey. Among them, 58.5% of infertility patients and 64.4% of spouses were aged between 30–35 years. Additionally, 60.3% of patients and 70.6% of spouses had stable employment. The majority of couples (67.4%) resided in urban or town areas. Furthermore, 34.7% of wives and 37.9% of husbands had a college degree or higher. The highest proportion of families (47.9%) had an average monthly income per person ranging from 3000 to 5000 yuan. Approximately 37.4% of women had been experiencing infertility for 3–5 years. A large percentage, 81.2% of patients, and 80.9% of spouses had no history of prior pregnancies. The proportion of primary infertility was 57.6%. Additionally, 57.1% of infertility couples had no prior experience with assisted reproduction. The majority of couples (66.5%) did not live with their parents ().
Table 1 Demographic and Fertility Characteristics of the Couples (n=340 Couples)
Gender-based comparisons revealed significant differences (). Wives exhibited significantly lower levels of fertility-related quality of life and dyadic coping scores compared to husbands (p<0.001). Among subscale scores, wives scored significantly lower than their spouses in both the Core FertiQoL and Treatment FertiQoL (p<0.001). In the comparison of dyadic coping dimensions, husbands exhibited significantly higher levels of negative coping than wives (p<0.001). When assessing the dimensions of fertility-related stress, wives scored significantly higher than their spouses in the Rejection of childless lifestyle and Need for parenthood dimensions (p<0.001).
Table 2 FertiQoL, Infertility-Related Stress and Dyadic Coping Scores According to Gender (n=340 Couples)
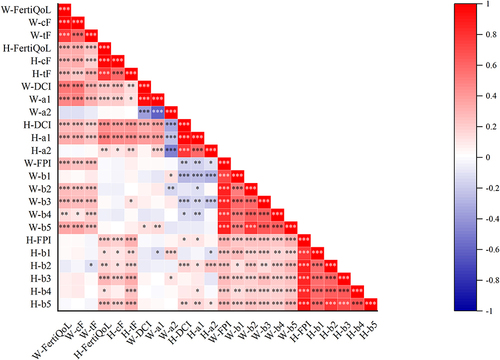
shows the results of the correlation analysis among fertility quality of life, infertility-related stress and dyadic coping in couples with infertility issues. For wives, there was a significant positive correlation between FertiQoL scores and FPI scores (r = 0.282, p < 0.01), as well as between FertiQoL scores and DCI scores (r = 0.523, p < 0.01). However, there was no significant correlation between DCI scores and FPI scores. For husbands, FertiQoL scores were positively correlated with FPI scores (r = 0.234, p < 0.01) and with DCI scores (r = 0.445, p < 0.01). Additionally, FPI scores were positively correlated with DCI scores (r = 0.111, p < 0.01) in husbands. There was a positive correlation between husbands’ FPI scores and wives’ FPI scores (r = 0.308, p < 0.01), as well as between husbands’ FertiQoL scores and wives’ FertiQoL scores (r = 0.327, p < 0.01), and husbands’ DCI scores and wives’ DCI scores (r = 0.320, p < 0.01). Husbands’ FertiQoL scores were positively correlated with wives’ DCI scores (r = 0.254, p < 0.01). However, there was no significant correlation between husbands’ FertiQoL scores and wives’ FPI scores. In the case of wives, there was a significant positive correlation between their FertiQoL scores and husbands’ DCI scores (r = 0.270, p < 0.01), but no correlation between wives’ FertiQoL scores and husbands’ FPI scores.
Figure 2 Correlation analysis among fertility quality of life, infertility-related stress and dyadic coping in couples with infertility issues. *P < 0.05; **P < 0.01, ***P < 0.001.
APIM
Using infertility-related stress and dyadic coping as predictor variables and the quality of life for wives and husbands as outcome variables, an APIM was constructed as shown in . The initial model’s fit was assessed using various goodness-of-fit indices, and the results are presented in . Nine commonly used fit indices were reported, and it was observed that the χ2/df, TLI, and RMSEA did not meet the acceptable standards. Therefore, modifications were needed for the initial model.
Table 3 Fitting Indicators of the Initial Structural Equation Model
Following model modification principles and guidance from AMOS 23.0 software (), path coefficients were sequentially removed as follows: 1. Wife’s infertility-related stress → Wife’s dyadic coping (p = 0.492). 2. Husband’s infertility-related stress → Wife’s dyadic coping (p = 0.889). The adjusted model fit results are presented in . All nine commonly used fit indices reported were within acceptable standards, indicating that the modified hypothetical model was valid.
Table 4 Fitting Indicators of the Corrected Structural Equation Model
Figure 3 Unstandardized parameter estimates of actor and partner effects of the wife’s and husband’s infertility-related stress and dyadic coping on quality of life. *P < 0.05; ***P < 0.001.
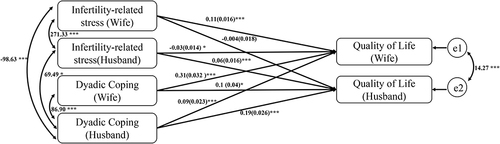
Infertility related stress in couples has a positive impact on their own quality of life, with a significant subjective effect (βWife=0.11, βHusband=0.06, p<0.001). Dyadic Coping in couples has a positive impact on their own quality of life, that is, the main effect is significant (βWife=0.31, βHusband=0.19, p<0.001). At the same time, Dyadic Coping in couples also has a positive impact on the quality of life of the other spouse, with a significant object effect (βWife=0.1, βHusband=0.09, p<0.001). The husband’s infertility related stress has a negative impact on the wife’s quality of life, that is, the object effect is significant (βHusband=−0.03, p<0.05). However, the wife’s infertility related stress has no significant impact on the husband’s quality of life.
Discussion
This study, conducted within the framework of the TSCM and the dyadic coping paradigm, examined the actor and partner effects of fertility-related stress on the life quality of couples. The primary objective of this research was to investigate gender differences in the life quality of couples experiencing infertility and the impact of infertility-related stress and dyadic coping on their life quality. The results of the actor and partner effects analysis partially align with our hypotheses. Husbands’ QoL is influenced by their own infertility-related stress, dyadic coping, and their wives’ dyadic coping. On the other hand, wives’ QoL is influenced by infertility-related stress and dyadic coping from both themselves and their spouses.
Our study found that, in couples experiencing infertility, wives reported lower overall levels of quality of life compared to husbands, which is consistent with previous research findings.Citation9 However, in this study, both wives and husbands had lower FertiQoL scores compared to research data from regions such as India, Germany, the Netherlands, but similar to research data from Taiwan.Citation25,Citation33–35 This could be attributed to cultural differences, economic levels, and social environments among different countries. Although quality of life scores for couples experiencing infertility differ across countries, it appears that wives tend to have worse quality of life, possibly due to the predominant role of women in fertility events and receiving assisted reproductive treatments. In the comparison of subscales, wives scored lower than husbands in both the Core and Treatment FertiQoL, likely due to significant physical and emotional changes that women experience during the disease and treatment process.Citation9 Wives are the primary recipients of treatment and are affected by factors such as medications, physical examinations, and disruptions to work or daily activities. Compared to husbands, wives experience greater physical and psychological impacts.Citation36 Additionally, women often face more blame and shame due to their condition, leading them to endure more suffering than men.Citation37 Some studies suggest that women may view sexual activity as a part of the treatment process, leading to reduced sexual satisfaction, which can result in dissatisfying emotions and marital relationships, further contributing to a decline in quality of life.Citation38
Furthermore, in the comparison of dyadic coping scores, we found that wives had lower dyadic coping levels than husbands. Additionally, dyadic coping scores were significantly positively correlated with quality of life. In other words, higher levels of dyadic coping led to higher quality of life. This is because mutual support and coping together can reduce stress and improve the physical and mental health of couples.Citation39 Positive communication between spouses helps convey stress to the partner and express distress.Citation40 In this study, infertility-related stress did not differ by gender within couples, but there was a correlation between wives’ stress and husbands’ stress. Furthermore, infertility-related stress between couples was also related to dyadic coping. As fertility is an event experienced jointly by couples, the perceived stress by both parties may be consistent and mutually influential.Citation16 When a family is troubled by infertility, stress from various sources such as society, parents, and sexuality can severely affect the quality of life.Citation25 However, in this study, stress could positively predict quality of life, indicating that moderate stress may act as a protective factor. Existing research has shown a positive correlation between moderate stress stimulation and psychological resilience, emotional regulation, and stress resistance. These psychological resources can help individuals better cope with stress and reduce negative impacts.Citation13 Moreover, stress can activate adaptation mechanisms and enhance cognitive functions.Citation41 Furthermore, the way couples cope with stress also affects their stress levels. Infertility, as a stressor, positive coping strategies can negatively predict fertility-related stress, while negative coping strategies can positively predict fertility-related stress.Citation42
In our study, wives’ and husbands’ QOL were affected by their own infertility-related stress and dyadic coping (actor effect), which is in line with our hypothesis. The association between women’s stress responses and fertility potential remains a subject of debate.Citation43 However, stress stimuli activate the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic-adrenal-medullary (SAM) axis, leading to neuroendocrine changes that may affect fertility.Citation44 Moreover, as women are the primary participants in the fertility process, they not only endure the pain caused by treatment but also face stigmatization from the external world.Citation38,Citation45 Women’s attitudes toward fertility are carefully planned, much like their attitudes toward careers, marriages, or other significant life events. Becoming a mother is a way for women to fulfill their gender roles and gain family and social status. However, the inability to meet these expectations can create stress for women and impact their quality of life.Citation15
In addition to the main effects, a significant finding in this study is the partner effects of infertility-related stress and dyadic coping in couples on their QoL, which confirms the viewpoint of mutual interdependence between partners as suggested by the TSCM.Citation23 Specifically, husbands’ life quality is influenced by their own infertility-related stress, dyadic coping, and their wives’ dyadic coping. On the other hand, wives’ life quality is influenced by both their own infertility-related stress and dyadic coping, as well as their husbands’ infertility-related stress and dyadic coping. This could be attributed to the fact that women tend to be more sensitive to external influences, especially from their partners, due to their emotionally sensitive nature.Citation46 Women may also have a lower adaptability to infertility-related events compared to men. Additionally, men often play a dominant role in decision-making regarding family events as the heads of households.Citation47 Patients’ primary living environment is typically their family, and spouses play a crucial role in the treatment process, observing symptoms, and managing daily life tasks. In the face of infertility-related stress, husbands’ emotions, attitudes, behaviors, and coping strategies can significantly impact their wives’ coping patterns and overall well-being.Citation48 Research has shown that stress from any source has a greater impact on wives’ lives than on husbands. It affects their self-satisfaction and overall happiness more than marital or health satisfaction and indirectly influences their quality of life through marital factors.Citation15 Previous studies have overlooked the interactions and differences between the quality of life in the context of infertility between spouses.Citation17 In reality, partners’ perceptions of fertility issues have a cross-partner impact on the patients’ emotional, physical, and relational quality of life.Citation34 A better quality of life for women was predicted by a better partner’s ability to identify and describe emotions, as well as by a better quality of life for men, who were more externally oriented thinking than their spouses.Citation49 Moreover, spousal support and coping together can significantly improve patients’ psychosocial adjustment.Citation46
We found significant differences in the relationship between infertility-related stress, dyadic coping, and quality of life between husbands and wives. According to the TSCM, the impact of infertility-related stress on quality of life in this study may be related to gender differences in cognitive appraisal and coping strategies.Citation19,Citation20 TSCM categorizes coping into problem-focused and emotion-focused strategies. Problem-focused coping refers to the regulatory strategies individuals employ to address stressors, while emotion-focused coping pertains to strategies individuals use to regulate emotional changes. The former is considered a positive coping mechanism, whereas the latter is viewed as a negative coping strategy.Citation50 When facing their wives’ illness-related stress, men tend to employ problem-focused or emotion-focused coping strategies and fewer avoidance strategies,Citation51 which results in better dyadic coping and quality of life for husbands. However, due to differences in coping strategies, women may struggle to deal with negative life events.Citation52 As a result, men achieve better quality of life, while women are more likely to experience negative emotions and poorer quality of life.
Patients and their spouses are interdependent and mutually influence each other in the family environment, and the fertility-related life quality of wives can also be influenced by their spouse’s stress or coping strategies. Therefore, during the infertility treatment process, it is important to pay attention to the fertility-related stress and dyadic coping of couples, taking into account gender differences. Considering the interactive effects of stress and dyadic coping in infertile couples, healthcare professionals should provide interventions and guidance with a focus on the couple, in addition to standard treatments and routine care. Group psychological therapy and couples coping enhancement training can be conducted within the couples facing fertility problems to address these issues effectively.
This study employed a cross-sectional research method, which cannot describe the trajectories of stress-related changes in patients and their spouses. It is unable to determine the critical threshold or range at which fertility-related stress shifts from being a protective factor to a detrimental one. The lack of evaluation of data on medical outcome and the exclusion of couples with male infertility problems that limit the generability. Therefore, future research should involve longitudinal follow-up, monitoring stress levels in these couples and evaluating medical outcome data throughout their entire treatment journey. Additionally, utilizing a latent difference score model to examine dynamic changes in stress and their impact on quality of life can help identify stress levels or ranges that are beneficial to the life quality of these couples. This information can provide robust evidence for the development and implementation of clinical intervention programs.
Conclusion
Husbands’ life quality is influenced by their own infertility-related stress, dyadic coping, and their wives’ dyadic coping. On the other hand, wives’ life quality is affected by infertility-related stress and dyadic coping from both themselves and their husbands. Therefore, infertility-related stress and dyadic coping in couples with infertility issues can serve as valuable indicators for predicting quality of life. The findings may also have relevant implications for ART clinical staff. This study indirectly supports the relationship between good psychological well-being and couples’ quality of life, highlighting the importance of early couples’ interventions. Focusing on the gender differences in stress and coping among these couples, and promoting positive coping styles may assist healthcare professionals in improving the quality of life for couples undergoing infertility treatment.
Abbreviations
QoL, quality of life; ART, Assisted Reproductive Technology; ESHRE, European Society of Human Reproduction and Embryology; ASRM, American Society for Reproductive Medicine; TSCM, Transactional Stress and Coping Model; DC, Dyadic Coping, APIM, Actor-Partner Interdependence Model; FertiQoL, Fertility Quality of Life Questionnaire; FPI, Fertility Problem Inventory; DCI, Dyadic Coping Inventory; STM, Systemic Transactional Model; HPA, hypothalamic-pituitary-adrenal; SAM, sympathetic-adrenal-medullary.
Ethics Approval and Consent to Participate
The study was approved by the ethics committee of the Nursing School, Lanzhou University, Lanzhou, China (LZUHLXY20210054). The written informed consents were obtained from participants.
Consent for Publication
All participants agree the publication of this study.
Disclosure
The authors declare no conflicts of interest in this work.
Acknowledgments
We would like to thank all the couples participating in our study and all the clinical staffs for their guidance and support.
Data Sharing Statement
All data generated or analysed during this study are included in this published article.
Additional information
Funding
References
- LoGiudice JA, Massaro J. The impact of complementary therapies on psychosocial factors in women undergoing in vitro fertilization (IVF): a systematic literature review. Appl Nurs Res. 2018;39:220–228. doi:10.1016/j.apnr.2017.11.025
- Carson SA, Kallen AN. Diagnosis and management of infertility: a review. JAMA. 2021;326(1):65–76. doi:10.1001/jama.2021.4788
- Wang Y, Fu Y, Ghazi P, et al. Prevalence of intimate partner violence against infertile women in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Glob Health. 2022;10(6):e820–e830. doi:10.1016/S2214-109X(22)00098-5
- Sun H, Gong TT, Jiang YT, Zhang S, Zhao YH, Wu QJ. Global, regional, and national prevalence and disability-adjusted life-years for infertility in 195 countries and territories, 1990–2017: results from a global burden of disease study, 2017. Aging. 2019;11(23):10952–10991. doi:10.18632/aging.102497
- De Rose M, Melamed R, Braga D, Setti A, Iaconelli A, Borges Junior E. The role of the duration of infertility on the of quality of life and psychological health in infertile couples. Hrod Sci. 2021;14(1):3–10.
- Zurlo MC, Cattaneo Della Volta MF, Vallone F. Predictors of quality of life and psychological health in infertile couples: the moderating role of duration of infertility. Qual Life Res. 2018;27(4):945–954. doi:10.1007/s11136-017-1781-4
- Kalaitzaki AE, Mavrogiannaki S, Makrigiannakis A. A prospective, cross-sectional study of the protective and risk psychological factors of successful in vitro fertilisation outcome: preliminary results in a Greek sample. J Obstet Gynaecol. 2020;40(3):382–387. doi:10.1080/01443615.2019.1631766
- Renzi A, Di Trani M, Solano L, Minutolo E, Tambelli R. Alexithymia, infertility-related stress and quality of life in women undergoing an assisted reproductive treatment. Stress Health. 2020;36(5):654–662. doi:10.1002/smi.2967
- Wadadekar GS, Inamdar DB, Nimbargi VR. Assessment of impact of infertility & its treatment on quality of life of infertile couples using fertility quality of life questionnaire. J Hum Rep. 2021;36(7):1862–1870.
- Pasch L, Holley S, Bleil M, Shehab D, Katz P, Adler N. Addressing the needs of fertility treatment patients and their partners: are they informed of and do they receive mental health services? Fertil Sterility. 2016;106(1):209–215.e202. doi:10.1016/j.fertnstert.2016.03.006
- Thyagaraju C, Naidu A. P–510 Psychological distress and quality of life in infertile women attending Infertility clinic at tertiary care center: a pilot study. Hum Reprod. 2021;36(Supplement_1). doi:10.1093/humrep/deab130.509
- Çambel B, Akköz Çevik S. Prevalence of intimate partner and family violence among women attending infertility clinic and relationship between violence and quality of life. J Obstetrics Gynaecol. 2022;42(6):2082–2088. doi:10.1080/01443615.2021.2024156
- Zhang X, Deng X, Mo Y, Li Y, Song X, Li H. Relationship between infertility-related stress and resilience with posttraumatic growth in infertile couples: gender differences and dyadic interaction. Hum Reprod. 2022;37(Supplement_1):1862–1870.
- Lei A, You H, Luo B, Ren J. The associations between infertility-related stress, family adaptability and family cohesion in infertile couples. Sci Rep. 2021;11(1):24220. doi:10.1038/s41598-021-03715-9
- Palomba S, Daolio J, Romeo S, Battaglia FA, Marci R, La Sala GB. Lifestyle and fertility: the influence of stress and quality of life on female fertility. Reprod Biol Endocrinol. 2018;16(1):113. doi:10.1186/s12958-018-0434-y
- Kim JH, Shin HS, Yun EK. A dyadic approach to infertility stress, marital adjustment, and depression on quality of life in infertile couples. J Holist Nurs. 2018;36(1):6–14. doi:10.1177/0898010116675987
- Abulizi M, Xu H, Abuduguli A, Zhao W, He L, Zhang C. Dual mediating effects of social support and fertility stress on mindfulness and fertility quality of life in infertile men: a case-control study. Front Psychol. 2023;14:1138282. doi:10.3389/fpsyg.2023.1138282
- Lazarus RS, Folkman S. Transactional theory and research on emotions and coping. Eur J Person. 1987;1(3):141–169. doi:10.1002/per.2410010304
- Pereira M, Moreira CS, Nogueira-Silva C, Izdebski P, Pereira MG. Breast cancer post-surgical impact on women s quality of life during chemotherapy treatment: a structural equation modelling approach. Eur J Cancer Care. 2021;30(1):e13349. doi:10.1111/ecc.13349
- Stormon N, Sexton C, Ford PJ, Eley DS. Understanding the well-being of dentistry students. Eur J Dent Educ. 2022;26(1):1–10. doi:10.1111/eje.12666
- Bodenmann G, Perrez M. Experimentell induzierte Spannung in dyadischen Wechselwirkungen. Vorstellung des EISI (Experimentell induzierte Spannung in dyadischen Wechselwirkungen) Experiment [Experimentally-induced stress in dyadic interactions. Presentation of the EISI (experimentally-induced stress in dyadic interactions) experiment]. Zeitschrift fur klinische Psychologie Psychopathologie und Psychotherapie. 1992;40(3):263–280. German.
- Peterson CRN BD, Rosen KH, Rosen KH, et al. Dyadic coping processes of men and women in infertile couples and their relationship to infertility stress, marital adjustment, and depression. Fertil Sterility. 2004;82(7):104. doi:10.1016/j.fertnstert.2004.07.263
- Ştefănuţ A, Vintilă M, Sârbescu P. Perception of disease, dyadic coping and the quality of life of oncology patients in the active treatment phase and their life partners: study protocol of an approach based on the actor-partner interdependence model. Eur J Cancer Care. 2021;30(6):e13374. doi:10.1111/ecc.13374
- Cormier SM, Suter GW, Fernandez MB, Zheng L. Adequacy of sample size for estimating a value from field observational data. Ecotoxicol Environ Saf. 2020;203:110992. doi:10.1016/j.ecoenv.2020.110992
- Aarts JW, van Empel IW, Boivin J, Nelen WL, Kremer JA, Verhaak CM. Relationship between quality of life and distress in infertility: a validation study of the Dutch FertiQoL. Hum Reprod. 2011;26(5):1112–1118. doi:10.1093/humrep/der051
- Newton CR, Sherrard W, Glavac I. The Fertility Problem Inventory: measuring perceived infertility-related stress. Fertil Steril. 1999;72(1):54–62. doi:10.1016/S0015-0282(99)00164-8
- Peng T, Coates R, Merriman G, Zhao Y, Maycock B. Testing the psychometric properties of Mandarin version of the fertility problem inventory (M-FPI) in an infertile Chinese sample. J Psychosom Obstet Gynaecol. 2011;32(4):173–181. doi:10.3109/0167482X.2011.609950
- Bodenmann G, Falconier M, Randall AK. Systemic-transactional model of dyadic coping. In: Chambers A, Breunlin D, editors. Encyclopedia of Couple and Family Therapy. Cham: Springer; 2017.
- Bodenmann G, Falconier M, Randall A. Editorial: dyadic coping. Fronti Psychol. 2019;10:1498. doi:10.3389/fpsyg.2019.01498
- Falconier M, Jackson J, Hilpert P, Bodenmann G. Dyadic coping and relationship satisfaction: a meta-analysis. Clinic Psychol Rev. 2015;42:28–46. doi:10.1016/j.cpr.2015.07.002
- Tang N, Jia Y, Zhao Q, et al. Influencing factors of dyadic coping among infertile women: a path analysis. Front Psychiatry. 2022;13:830039. doi:10.3389/fpsyt.2022.830039
- Turcotte S, Robitaille H, Blair L, Légaré F. The actor-partner interdependence model in shared decision-making: an illustrative example of its application to the physician-patient dyad in primary care consultations. J Clin Epidemiol. 2019;108:132–139. doi:10.1016/j.jclinepi.2018.11.027
- Desai HJ, Gundabattula SR. Quality of life in Indian women with fertility problems as assessed by the FertiQoL questionnaire: a single center cross sectional study. J Psychosom Obstet Gynaecol. 2019;40(1):82–87. doi:10.1080/0167482X.2017.1405257
- Sexty RE, Griesinger G, Kayser J, et al. Psychometric characteristics of the FertiQoL questionnaire in a German sample of infertile individuals and couples. Health Qual Life Outcomes. 2018;16(1):233. doi:10.1186/s12955-018-1058-9
- Hsu PY, Lin MW, Hwang JL, Lee MS, Wu MH. The fertility quality of life (FertiQoL) questionnaire in Taiwanese infertile couples. Taiwan J Obstet Gynecol. 2013;52(2):204–209. doi:10.1016/j.tjog.2013.04.009
- Vatanparast M, Yasini Ardekani SM, Anvari M, Kalantari A, Yaghmaie F, Royani Z. Resilience as the predictor of quality of life in the infertile couples as the most neglected and silent minorities. J Reprod Infant Psychol. 2022;40(3):216–227. doi:10.1080/02646838.2020.1843613
- Peronace LA, Boivin J, Schmidt L. Patterns of suffering and social interactions in infertile men: 12 months after unsuccessful treatment. J Psychosom Obstet Gynaecol. 2007;28(2):105–114. doi:10.1080/01674820701410049
- Bose S, Roy B, Umesh S. Marital duration, and fertility-related stress as predictors of quality of life: gender differences among primary infertile couples. J Hum Reprod Sci. 2021;14(2):184–190. doi:10.4103/jhrs.jhrs_233_20
- Busch A, Fringer A. Psychosocial impact of multiple sclerosis on couples: relationship between anxiety, depression, and stress communication of both partners. J Prim Care Commun Health. 2022;13:21501319221119142. doi:10.1177/21501319221119142
- Molgora S, Fenaroli V, Acquati C, De Donno A, Baldini M, Saita E. Examining the role of dyadic coping on the marital adjustment of couples undergoing Assisted Reproductive Technology (ART). Fronti Psychol. 2019;10:415. doi:10.3389/fpsyg.2019.00415
- Lee EH, Park JY, Kwon HJ, Han PL. Repeated exposure with short-term behavioral stress resolves pre-existing stress-induced depressive-like behavior in mice. Nat Commun. 2021;12(1):6682. doi:10.1038/s41467-021-26968-4
- Truong QL, Nguyen TT, Luong BT, Dang QV. Coping styles among Vietnamese people with infertility diagnosis: does type of infertility-related stress really matter? J Reprod Infant Psychol. 2022;40(1):1–12. doi:10.1080/02646838.2021.2020977
- Biringer E, Howard LM, Kessler U, Stewart R, Mykletun A. Is infertility really associated with higher levels of mental distress in the female population? Results from the North-Trondelag Health Study and the Medical Birth Registry of Norway. J Psychosom Obstet Gynaecol. 2015;36(2):38–45. doi:10.3109/0167482X.2014.992411
- Ulrich-Lai YM, Herman JP. Neural regulation of endocrine and autonomic stress responses. Nat Rev Neurosci. 2009;10(6):397–409. doi:10.1038/nrn2647
- Zhao Q, Huangfu C, Li J, Liu H, Tang N. Psychological resilience as the mediating factor between stigma and social avoidance and distress of infertility patients in China: a structural equation modeling analysis. Psychol Res Behav Manag. 2022;15:391–403. doi:10.2147/PRBM.S354803
- Zhang J, Yu NX, Zhou M, Zhang J. Dyadic effects of resilience on well-being in Chinese older couples: mediating role of spousal support. J Fam Psychol. 2017;31(3):273–281. doi:10.1037/fam0000250
- Hiew DN, Halford WK, van de Vijver FJ, Liu S. Communication and relationship satisfaction in Chinese, Western, and intercultural Chinese-Western couples. J Fam Psychol. 2016;30(2):193–202. doi:10.1037/fam0000144
- Chaves C, Canavarro MC, Moura-Ramos M. The role of dyadic coping on the marital and emotional adjustment of couples with infertility. Fam Process. 2019;58(2):509–523. doi:10.1111/famp.12364
- Renzi A, Fedele F, Di Trani M. Assisted reproductive treatments, quality of life, and alexithymia in couples. Healthcare. 2023;11(7):1026.
- Folkman S. Stress: appraisal and Coping. In: Gellman MD, Turner JR, editors. Encyclopedia of Behavioral Medicine. New York: Springer New York; 2013:1913–1915.
- Yu Y, Peng L, Chen L, et al. Resilience and social support promote posttraumatic growth of women with infertility: the mediating role of positive coping. Psychiatry Res. 2014;215(2):401–405. doi:10.1016/j.psychres.2013.10.032
- Kim JE, Song IH, Lee SH. Gender differences of stressful life events, coping style, symptom severity, and health-related quality of life in patients with panic disorder. J Nerv Ment Dis. 2017;205(9):714–719. doi:10.1097/NMD.0000000000000696