Abstract
Background
Medical ethics is not given due priority in obstetric care in many developing countries, and the extent to which patients value compliance with ethical precepts is largely unexplored.
Objective
To describe the expectations and experiences of obstetric patients in South East Nigeria with respect to how medical ethics principles were adhered to during their care.
Methods
This was a cross-sectional, questionnaire-based study involving parturient women followed in three tertiary hospitals in South East Nigeria.
Results
A total of 1,112 women were studied. The mean age of respondents was 29.7 ± 4.1 years. Approximately 98% had at least secondary education. Ninety-six percent considered ethical aspects of care as important. On the average, over 75% of patients expected their doctors to comply with the different principles of medical ethics and specifically, more than 76% of respondents expected their doctors to comply with ethical principles related to information and consent during their antenatal and delivery care. There was a statistically significant difference between the proportions of women who expected compliance of doctors with ethical principles and those who did not (P < 0.001). Multivariate analysis showed that increasing levels of skilled occupation (odds ratio [OR] 9.35, P < 0.001), and residence in urban areas (OR 2.41, P < 0.001) increased the likelihood of patients expecting to be informed about their medical conditions and their opinions being sought. Although the self-reported experiences of patients concerning adherence to ethical principles by doctors were encouraging, experiences fell short of expectations, as the level of expectation of patients was significantly higher than the level of observed compliance for all the principles of medical ethics.
Conclusion
The level of practice of medical ethics principles by doctors during obstetric care in South East Nigeria was encouraging but still fell short of the expectations of patients. It is recommended that curriculum-based training of doctors and medical students should be implemented, and hospital policy makers should do more to promote ethical aspects of care, by providing official written guidelines for adherence to medical ethical principles during obstetric care.
Keywords:
Introduction
Despite the existence of a code of medical ethics published by the regulatory authority for Medical Ethics in Nigeria (the Medical and Dental Council of Nigeria), there is practically no formal curriculum-based training for doctors and medical students on medical ethics.Citation1 Empirical observations suggest that the observance of ethical precepts by health workers is often a matter of individual attitude to work, rather than compliance with enacted rules. Communication between doctor and patient is still heavily driven by the doctor, and patient participation often depends entirely on prompting by the doctor. This attitude to medical ethics has festered unabated, mainly because of many other overarching factors related to the provision, access, and utilization of medical care in developing countries.Citation2
First among these concerns is the unavailability of adequate manpower and resources for health care, resulting in many health facilities and communities being under served.Citation2 Added to this, there are cultural inhibitions and widespread ignorance among the populace, especially on health issues, resulting in poor utilization of many rural health facilities, the inability of patients to assert their rights to free communication with their doctors,Citation3 and the possibility of the misinterpretation (by patients and their relations) of western-style informed consent practices as evidence that the doctor “does not know what to do.”Citation4 Besides these, there are also high population-to-doctor ratios, which result in work overload for doctors.
In the midst of these scenarios, it has become debatable whether it is worthwhile to promote western-style medical ethics in developing countries, where basic health care is still not available to many.Citation2 Consequently, medical ethics is evolving rather slowly in Nigeria, and even physicians are unsure of the direction it should take.Citation5 For instance, approximately 73% of surgeons surveyed in a recent study in Nigeria agreed that informed consent “was alien to the African psyche.”Citation5 There remains substantial doubt about whether western-style medical ethics practices are sustainable in Africa, given the cultural and socioeconomic differences between the two societies.Citation2,Citation4–Citation7
In relation to obstetrics practice, anecdotal evidence shows that many patients feel that they are not treated with respect and dignity in many public hospitals in Nigeria, reinforcing the existence of inadequate attention of health workers to the ethical aspects of care. The current high rate of patronage of unskilled providers for antenatal and delivery care in Nigeria appears to be fanned, at least in part, by a lack of trust in public hospitals. The prevalent high maternal mortality rates in Nigeria are blamed largely on the low rate of deliveries attended by skilled attendants.Citation8 Promoting respectful and dignified treatment could therefore be useful in addressing the problem of poor utilization of skilled attendants in public hospitals.Citation9
We found scant literature on the ethical aspects of obstetric care in Nigeria.Citation10–Citation13 In order to contribute to the debate on whether medical ethics should be emphasized in developing countries, we sought to explore patients’ perspectives on the observance and practice of ethical precepts during obstetric care. The aims of this study were therefore to describe patients’ expectations and experiences of the ethical conduct of their physicians during obstetric care in three university teaching hospitals in South East Nigeria.
Methods
Study area/centers
South East Nigeria is made up of five states and has a combined population of about 20 million, based on the 2006 Nigeria national census.Citation14 The area is served by ten tertiary teaching hospitals. The study took place at three of these centers in Enugu and Ebonyi states namely, the University of Nigeria Teaching Hospital Enugu; the Federal Medical Centre, Abakaliki, Ebonyi State; and the Enugu State University Teaching Hospital, Enugu. These hospitals cater to a combined population of about 5 million urban and rural dwellers.
Study population
The study population included parturient women who had antenatal care and/or delivery at the study hospitals during the study period. The obstetric clients in these hospitals are usually self-referred, pregnant women who desire to receive care under specialist obstetricians and/or in a facility with modern facilities for obstetric care, and women with complicated pregnancies who have been referred from surrounding lower-level health facilities. In all three hospitals, women who had normal deliveries were usually observed in the hospital for 48 hours before discharge, while those that had cesarean delivery were usually discharged on the fifth to seventh postoperative day.
Study period
The study covered the period from July 1, 2010 to June 30, 2011.
Study design
This was a cross-sectional, questionnaire-based study involving booked parturient women followed in three tertiary maternity hospitals in South East Nigeria.
Sampling technique
A convenience sample of the three teaching hospitals was selected from the eleven teaching hospitals in the South East geopolitical zone of Nigeria. Sampling of study participants was purposive and involved enrolment of consecutive consenting women who delivered during the study period.
Data collection
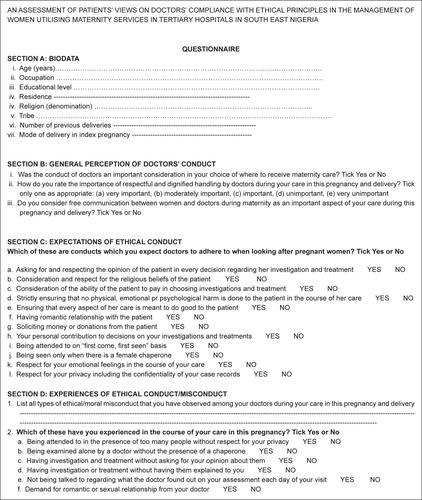
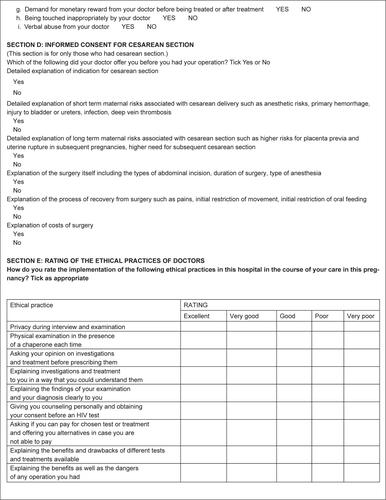
In each of the three selected hospitals, 500 consecutive consenting women who delivered during the study period were administered anonymized, semistructured, pretested questionnaires developed for the study. The questionnaires were self-administered when the woman was sufficiently literate to understand it or otherwise, were interviewer-administered. For literate patients, the questionnaire was administered in the English language, whereas for semiliterate women, the questionnaire was administered by the interviewer, in the Igbo language. The questions were based on their experiences in the “index” pregnancy. The questionnaire was organized in three parts, with the first two parts involving open-ended questions. The first part dwelt on obstetric and demographic data, while the second part explored what the women perceived to be ethical misconduct and their expectations regarding the practice of ethical principles by doctors; the third part contained closed-ended questions that elicited the experiences of patients concerning how their doctors observed specific aspects of the ethical principles of autonomy, justice, beneficence, and nonmaleficence.Citation15 The questionnaire was designed to yield semiquantitative data, with participants’ responses recorded on binary (Yes/No) or Likert scales. For patients who had uncomplicated vaginal deliveries, the questionnaire was administered on the second postpartum day, whereas for those that had cesarean delivery, it was administered on the fifth postpartum day (Supplementary figure).
Data analysis
The statistical analysis was done using SPSS statistical software version 17.0 for Windows (SPSS Inc., Chicago, IL, USA), using descriptive and inferential statistics. We related the conduct that patients expected or experienced from doctors to medical ethics principles and then interpreted which ethical principle each behavior represented. The main outcome measures were the proportions of respondents who expected specified ethical behaviors by their doctors and the proportions of women who experienced or observed compliance with ethical principles. The frequencies of different responses were expressed as percentages. Tests of significance for the differences between categorical variables were done with the Chi-square test. Bivariate logistic regression was used to determine the predictability of the expectations of patients. Those who expected compliance were coded as “Yes” (1), while those who did not were coded as “No” (0). The results were reported as adjusted odds ratios and 95% confidence intervals. A P-value ≤ 0.05 was considered significant.
Ethical clearance
Ethical clearance for the study was obtained from the Research Ethics Committees of the three hospitals.
Results
A total of 1,500 questionnaires were distributed, out of which 1,420 were returned. Of these, 1,112 (74.1%) were fully completed, and these were used for analysis. A total of 320 of the 1,112 respondents were from University of Nigeria Teaching Hospital, 309 from the Federal Medical Centre Abakaliki, while 483 were from the Enugu State University Teaching Hospital.
Sociodemographic characteristics
The mean age of respondents was 29.7 ± 4.1 years. Approximately 98% had at least secondary education, with about 58% possessing a postsecondary certificate. shows the demographic and obstetric characteristics of the respondents.
Table 1 The demographic and obstetric characteristics of respondents
Expectations of obstetric patients and factors that predict expectations
Approximately 89% (990/1,112) of respondents considered free communication between doctors and patients as a very important aspect of care, and 80% (890/1,112) of respondents stated that the conduct of doctors and other health workers was an important consideration that informed their choice of where to receive maternity care. On a six-point scale, 66% (734/1,112) considered ethical aspects of care as very important, 20% (222/1,112) as moderately important, 10% (111/1,112) as important, and 4% (45/1,112) as unimportant; no woman considered respectful and dignified treatment as moderately unimportant or very unimportant.
summarizes the distribution of respondents, based on the ethical practices they expected from doctors. Approximately 78% (867/1,112) expected to be fully informed about their conditions, while 76% (845/1,112) expected their opinions and consent to be sought for investigations and treatment that they were to undergo.
Table 2 The comparison of the numbers of patients who expected compliance with ethical principles by their doctors
summarizes the results of bivariate logistic regression to determine which patient characteristics predicted the type of expectation of patients, with respect to autonomy-related conduct. Occupation, age, residence, and religious denomination were all predictors of patients who would expect information and consent for investigations and treatment plans. Increasing levels of skilled occupation and residence in urban areas increased the likelihood of patients expecting to be informed about their medical conditions and their opinions being sought. However, increasing age and being Roman Catholic decreased the likelihood. Educational level, parity, mode of delivery, and tribal group were not significant predictors of the likelihood of expecting to have information and having the patient’s consent sought.
Table 3 Results of the binary logistic regression for predicting the expectation of patients, with respect to the compliance of doctors with ethical principles
With respect to the expectation of justice-related conduct, being a low skilled worker, age, residence, and tribe were significant predictors of the expectations of the patient. Low-skilled occupation, urban residence, and being of the Igbo tribe increased the likelihood of a patient’s expectation that the doctor give consideration for their ability to pay for investigations and treatment, while increasing age decreased the likelihood. Educational status, being a Catholic (or not), parity, and mode of delivery did not have a statistically significant ability to predict the expectation of women with respect to justice-related conduct.
Patients’ experiences of medical ethics practices of their doctors
The distribution of patients based on their experiences with respect to the medical ethics practices of doctors is summarized in . Approximately 78.4% (872/1,112) of respondents reported experiencing at least one instance where the doctor’s conduct could be interpreted as a failure to comply with medical ethics principles, in the course of their care in the index pregnancy.
Table 4 Comparison of the experiences of women concerning medical ethics practices
Informed consent for cesarean section
One hundred and fifty-two women who had a cesarean section responded to questions about their experiences with the process of obtaining their consent for surgery. Of these, 124 had a primary cesarean section, while 28 had a repeat cesarean section. For 36 women (23.7%), the consent was signed by the woman’s husband, and all of these cases were for emergency cesarean sections. summarizes the content of the informed consent for cesarean section, as reported by patients.
Table 5 Self-reported content of counseling for cesarean section
Comparison of expectations with experiences
summarizes the comparison of expectations with the experiences of patients, with respect to the medical ethics practices of doctors. The expectations of patients differed significantly from their actual experiences with respect to privacy, the provision of information to patients, the solicitation of patients’ opinions and consent, regular and punctual attendance to appointments, fairness in attending to patients in clinics (ie, on a “first come, first seen” basis), and consideration of cost when issuing prescriptions.
Table 6 Showing the comparison of expectations and the actual experiences of compliance with ethical principles by doctors
Rating of doctors’ compliance with ethical principles
summarizes patients’ rating of the ethical principles practiced by doctors. Favorable rating of the ethical principles practiced by doctors ranged from 41.65% to 69.4%. The highest rating was for the provision of information to patients, while the lowest rating was that of fairness in the order of attending to patients. Approximately 41% felt that doctors were poor in obtaining their consent for interventions.
Table 7 Rating of ethical practices of doctors
Discussion
The study shows that an overwhelming proportion of women considered free communication between doctors and patients to be important and that there were significantly greater proportions of respondents who valued and expected their doctors to exhibit conduct in keeping with the cardinal principles of medical ethicsCitation13 than proportions who did not. This suggests a high level of expectations of ethical practice from doctors. Given the demographics of the studied population, it would therefore appear that among the urban patient population in this developing-country setting, many value the ethical aspects of care.
The remaining discussion of the findings of this study will address the principles of medical ethics enunciated by Beauchamp and Childress.Citation15
Patient autonomy
The ethical principle of patient autonomy determines the appropriate attitude of doctors to foster patients’ right to information, primacy in decision making, and confidentiality and privacy. The basic quality of primacy in making decisions is the basis for the requirement of informed consent.Citation2,Citation9,Citation10 In this study, a high proportion of respondents (76%) expected doctors to explain diagnoses and options of management and to seek their opinions and consent during their care. This is less than the 97% found by Chung et al, in a study of a nonobstetric inpatients in the US but higher than the 23.9% found by Cetin et al, in a general patient population in a military hospital in Turkey.Citation16,Citation17 The highly selective nature of the patient population in this study might explain this contrast, and it will remain to be seen whether similar findings can be obtainable in the general patient populations.
The study also showed that the proportion of patients who expected adequate information and respect for their opinions was significantly greater than the proportion who acknowledged experiencing these practices. This suggests a gap between expectations and practice and could mean that although the level of ethical practices may be encouraging, doctors need to do more to satisfy the expectations of this patient population. In contrast to a recent survey that showed that surgeons in South West Nigeria considered informed consent to be “alien to African psyche,”Citation5 the findings in this study show that urban women in the South East Nigeria value information and respect for their opinions. The differences in the two studies may be due to the study populations (doctors versus pregnant women), but it may also suggest that doctors may need to begin to modify their attitude towards medical ethics in developing societies, like Nigeria.
With respect to the practice of informed consent before a cesarean section, this study found that although efforts were made to obtain consent for both emergency and elective cesarean section, the contents of counseling for such consent appeared to be scanty. In most cases, counseling involved a brief explanation of the indication for the surgery. A previous study of surgical patients in this center alluded to the possibility that scanty content of counseling for surgery might be due to the fear that patients could misinterpret a detailed explanation of risks as a sign that the doctor was incompetent, a throwback to the possibility that patients in this area could easily question the doctors’ conduct, including competence. The scanty content of counseling for informed consent defeats the purpose of such counseling, which should be to provide sufficient information for the patient to make up her mind about the procedure. The findings from this study therefore demonstrate the need for the improvement of presurgical counseling during obstetric care in the study centers.
Nonmaleficence
In this study, the perception by patients that strike actions by doctors constituted ethical misconduct was rife. Similarly, patients perceived lateness to clinics and absence from clinics as ethical misconduct. Whether this conduct constitutes ethical or professional misconduct is debatable. However, the feelings of patients about strike actions need to be taken seriously in view of the need to sustain the patronage of skilled birth attendants by these women. This is necessary to avert recourse to unskilled attendants, which has adverse implications for maternal morbidity and mortality.Citation11 That many women go elsewhere to deliver after attending antenatal care in teaching hospitals has severally been attributed to dissatisfaction with health workers’ conduct in these teaching centers. Other inappropriate conduct allegedly experienced by pregnant women included verbal abuse, sexual overtures, including inappropriate touching, as well as the demand for financial gratification. Although the proportion of women who experienced these practices ranged from 2%–7%, the fact that this inappropriate conduct existed at tertiary levels of care in this country suggests that more needs to be done to protect patients, and one way of doing this is through the enactment of and strict compliance with hospital policies mandating the use of female chaperones for every examination.
Justice
Justice with respect to obstetric care is related to fair choices regarding investigations and treatment, especially with respect to cost. It can also be related to fairness in attending to patients in clinics, such as seeing patients on a “first come, first seen” basis. The highest proportions of respondents that expected compliance with justice-related ethical principles were, however, found among those who expected doctors to consider cost, efficacy, and their ability to pay for investigations and treatment. This underlines the important place of health care financing in obstetric care in these centers. The ethics of health care financing in developing countries is made more pertinent by the fact that well-structured health insurance schemes either do not exist or are not well developed. Although the recently introduced national health insurance scheme in Nigeria covers antenatal care and normal deliveries, the proportion of the population covered by the insurance scheme is presently very limited.
Predicting patients’ expectations
Although all patients should receive due consideration for the ethical aspects of care, irrespective of their levels of awareness, predicting the specific expectation of patients may assist in laying the appropriate emphases. The study showed that certain demographic features could predict the expectations of patients in this obstetric population. Higher-skilled occupation increased the likelihood of expecting detailed information and informed consent. This may be due to the greater economic and social empowerment of highly skilled workers compared with low-skilled ones. Similarly, residence in urban area also increased this likelihood, perhaps for reasons related to awareness and empowerment. Conversely, increasing age and being Roman Catholic decreased the likelihood that patients would expect their doctors to give them detailed information and also seek their opinions on their management. On its own, increasing level of education had no significant effect on the expectation of detailed information and patients’ opinions. These findings are similar to the findings by Chung et al, in the US, that increasing age was a predictor of patients leaving medical decisions to the doctor but is contrary to their findings that university education predicted patients’ desire to have more control over their medical decisions.Citation16
Strengths and weaknesses of study
The major strengths of this study include the large sample size and the multicenter design, which broadened the spread of respondents and may have enhanced the external validity of the findings. The major drawbacks were the hospital-based nature of the study and the use of semistructured questionnaires, both of which might have biased the responses of women, who might have wanted to please the interviewers with favorable responses. Evaluating the expectations of ethical conduct after delivery exposed the study to recall bias. Also, the fact that focus-group discussions were not done excluded a detailed evaluation of the feelings of patients. Finally, the choice of a highly specific patient population means that the findings cannot be generalized to the general patient population in this area.
Conclusion
We conclude that most obstetric patients in the urban centers studied valued the ethical aspects of care and that levels of expectations were high. The current levels of adherence to ethical principles by doctors are encouraging, although they fall short of the expectations of patients. There is a need, therefore, for obstetricians to do more to meet the ethical expectations of patients, in this study population. The findings of this study suggest that medical ethics could become an important aspect of obstetric care in Nigeria as literacy levels and female empowerment improve among the population. Undergraduate and postgraduate medical schools should therefore develop curriculum-based training on medical ethics for doctors and medical students. Hospital policy makers need to provide written and official guidelines for adherence to medical ethical principles during obstetric care, including a more elaborate process for obtaining informed consent for surgeries. We recommend a further study on a general patient population in this area, to determine the applicability of the findings in this study to the general patient population in this resource-constrained setting.
Acknowledgments
We acknowledge the contributions of the Labor ward staff of the study hospitals as well as Drs Blanche Ngaitu, Emeka Onyia, Emeka Okonkwo, Ugochukwu Ezenyirioha, Sunday Mba, and Chioma Emegoakor, who all assisted with the data collection for this study.
Disclosure
The authors declare no conflicts of interest in this work.
Reference
- Medical and Dental Council of Nigeria [MDCN]Code on Medical Ethics in Nigeria: Rules of Professional Conduct for Medical and Dental PractitionersLagosMDCN2004
- OlwenyCBioethics in developing countries: ethics of scarcity and sacrificeJ Med Ethics19942031691747996563
- EzeomeERMarshallPAInformed consent practices in NigeriaDev World Bioeth20099313814818452553
- AguKAInformed consent policy and surgeons in South East NigeriaNigeria J Surg20033941
- OgundiranTOAdebamowoCASurgeons’ opinions and practice of informed consent in NigeriaJ Med Ethics2010361274174520940174
- IraborDOOmonzejelePLocal attitudes, moral obligation, customary obedience and other cultural practices: their influence on the process of gaining informed consent for surgery in a tertiary institution in a developing countryDev World Bioeth200991344219302568
- OsamorPEKassNDecision-making and motivation to participate in biomedical research in southwest NigeriaDev World Bioeth2012122879522708614
- OnahHEOkaroJMUmehUChigbuCOMaternal mortality in health institutions with emergency obstetric care facilities in Enugu State, NigeriaJ Obstet Gynaecol200525656957416234142
- JoffeSManocchiaMWeeksJCClearyPDWhat do patients value in their hospital care? An empirical perspective on autonomy centred bioethicsJ Med Ethics200329210310812672891
- OsimeOCOkojieOOsadolorFMohammedSCurrent practices and medico-legal aspects of pre-operative consentEast Afr Med J200481733133515490703
- BakoBUmarNGarbaNKhanNInformed consent practices and its implication for emergency obstetrics care in azare, north-eastern NigeriaAnn Med Health Sci Res20111214915723209969
- FadareJOSome ethical issues in the prenatal diagnosis of sickle cell anemiaAnnals of Ibadan Postgrad Med2009722628
- AduduOPAduduOGTherapeutic non-disclosure of adverse health information to an obstetric patient: case reportEast Afr Med J200885525325618814537
- National Population Commission (NPC) [Nigeria] and ICF MacroNigeria Demographic and Health Survey 2008AbujaNational Population Commission2009
- BeauchampTLChildressJFPrinciples of Biomedical Ethics6th edOxfordOxford University Press2009
- ChungGSLawrenceRECurlinFAAroraVMeltzerDOPredictors of hospitalised patients’ preferences for physician-directed medical decision-makingJ Med Ethics2012382778221697296
- CetinMUcarMGüvenTAtacAOzerMWhat do patients expect from their physicians? Qualitative research on the ethical aspects of patient statementsJ Med Ethics201238211211621690229