Abstract
Background
Female condoms are the only currently available woman-initiated option that offers dual protection from pregnancy and sexually transmitted infections, including HIV. The Woman’s Condom is a new female condom designed to provide dual protection and to be highly pleasurable and acceptable.
Objective
We sought to estimate the potential dual health impact and cost-effectiveness of a Woman’s Condom distribution program in 13 sub-Saharan African countries with HIV prevalence rates >4% among adults aged 15–49 years. We used two separate, publicly available models for this analysis, the Impact 2 model developed by Marie Stopes International and the Population Services International disability-adjusted life years (DALY) calculator program. We estimated the potential numbers of pregnancies and DALYs averted when the Woman’s Condom is used as a family planning method and the HIV infections and DALYs averted when it is used as an HIV prevention method.
Results
Programming 100,000 Woman’s Condoms in each of 13 countries in sub-Saharan Africa during a 1-year period could potentially prevent 194 pregnancies and an average of 21 HIV infections in each country. When using the World Health Organization CHOosing Interventions that are Cost-Effective (WHO-CHOICE) criteria as a threshold to infer the potential cost-effectiveness of the Woman’s Condom, we found that the Woman’s Condom would be considered cost-effective.
Conclusion
This was a first and successful attempt to estimate the impact of dual protection of female condoms. The health impact is greater for the use of the Woman’s Condom as an HIV prevention method than for contraception. Dual use of the Woman’s Condom increases the overall health impact. The Woman’s Condom was found to be very cost-effective in all 13 countries in our sample.
Introduction
As governments, donors, and policymakers strive to find the optimal mix of family planning and HIV prevention interventions for their communities, they cannot afford to overlook the female condom. Female condoms are the only woman-initiated method of dual protection against sexually transmitted infections and pregnancy available today. Female condoms were identified by the United Nations Commission on Life-Saving Commodities for Women and ChildrenCitation1 as one of the 13 essential and overlooked lifesaving commodities, and global attention and action are being marshaled toward developing the female condom market and ensuring that products are widely accessible. According to the Reproductive Health Interchange – a harmonized database of contraceptive orders and shipments from major donors and government procurement agencies – more than 73 million female condoms, primarily the FC2 female condom (Female Health Company) were procured and distributed to more than 100 countries in 2013–2014.Citation2 While procurement has increased over the past decade, the cost of female condoms is often cited as a reason why this lifesaving technology is underutilized. Modeling analyses suggest that female condoms can be a highly cost-effective public health intervention when compared to the costs of HIV treatment. One model shows substantial cost savings to the health sector in both South Africa and Brazil based on different use scenarios of the FC2 female condom.Citation3 For example, the model estimated that in South Africa, assuming a low uptake of 4 million (at an estimated unit cost of US$0.77 for product, distribution, training, and education), the female condom would prevent 1,740 HIV infections, with a net savings to the health care system of about US$980,000. Another model estimates that an investment of US$4,000 for female condoms distributed to 1,000 commercial sex workers in rural South Africa would prevent many cases of HIV, syphilis, and gonorrhea, yielding net savings to the health sector of just over US$9,000.Citation4 A retrospective economic evaluation of a female condom promotion program in Washington, DC, estimated that the program (at a cost of US$414,186 to distribute 200,000 female condoms and provide educational services) averted enough HIV infections in the first year alone to save more than US$8 million in future medical care costs (over and above the program).Citation5,Citation6 The additional benefits associated with female condoms, such as prevention of pregnancy and prevention of mother-to-child transmission of HIV, have not been quantified in the referenced models.
This analysis attempts to calculate the benefits of the dual protection offered by the Woman’s Condom, a second-generation female condom. PATH developed the Woman’s Condom through a user-centered process with input from women and couples from four countries representing diverse cultures and contexts (Mexico, South Africa, Thailand, and the US). This process resulted in an innovative female condom designed to provide dual protection and to be highly pleasurable and acceptable. As part of the strategic planning for introduction of the Woman’s Condom into sub-Saharan African countries, we sought to estimate the potential health impact of the Woman’s Condom attributable to its dual use as a family planning method and also an HIV prevention method. We estimated the potential cost-effectiveness of a hypothetical Woman’s Condom distribution program in 13 sub-Saharan African countries.
Methods
The following countries were included in our analysis: Botswana, Cameroon, Kenya, Lesotho, Malawi, Mozambique, Namibia, South Africa, Swaziland, Tanzania, Uganda, Zambia, and Zimbabwe. We selected these countries because our introduction strategy for the Woman’s Condom is to target those sub-Saharan African countries whose HIV prevalence rates are greater than 4% among adults aged 15–49 years.Citation7
We used two separate models that are publicly available online to estimate the potential impact of the Woman’s Condom. We used the Impact 2 model (v2–1) developed by Marie Stopes InternationalCitation8 to estimate the potential impact of using the Woman’s Condom as a family planning method. We estimated the impact that could be achieved by distributing 100,000 Woman’s Condoms over a 1-year period in each of the countries in our analysis. We assumed that distribution of this product volume could be achieved over 1 year in a given country where a new female condom is being introduced. Distribution of 100,000 units is a typical product volume for initial introduction efforts. We assumed the same quantity of units would be distributed in all the countries, and this assumption enabled intercountry comparison so that we could identify where the condoms would have the greatest impact as measured by the disability-adjusted life years (DALYs) averted. In addition, we chose a 1-year time frame for the analysis because we assumed that the condoms would be used in the same year they are distributed and hence the benefits would occur in that year.
The Impact 2 model and related documentation are available for download from the Marie Stopes International website.Citation9 Briefly, the Impact 2 model is a publicly available tool for estimating the impact of reproductive health programs. It is pre-populated with data for all developing countries, and it can be used to estimate the health and economic impact of family planning products. Its outputs include the estimated pregnancies, births, maternal deaths, child deaths, and DALYs averted and also the health care costs saved for the specified service provision level.
We used the Population Services International (PSI) DALY calculatorCitation10 to estimate the potential impact of using the Woman’s Condom as an HIV prevention method. The underlying model for the estimates from the PSI DALY calculator that are referenced in this analysis is the PSI HIV Heterosexual Transmission Health Impact Estimation Sub-Model. The methodology document for this sub-model can be found on the PSI website.Citation11 The calculator estimates the number of DALYs and deaths averted for the specified level of sales of health products.
Inputs for our analysis
Service provision levels: we explored the impact of distributing 100,000 condoms annually in each country.
Costs to deliver services per client: the program costs for a Woman’s Condom distribution program include the costs of distribution, education, and promotion. For our analysis, we used the program costs data reported by PSI programs.Citation12 Average program costs per condom were available for only six of the countries in our sample, as shown in . For the countries where the program costs were not reported, we used the average cost for the six countries (US$1.27 in 2007) as the program costs. The average costs were used as a way to assign costs to countries that did not have any cost data. The program costs were then updated to 2012 US$ using the consumer price index.Citation13
Table 1 Estimated program costs per condom distributed
We estimated that the price for our product would be US$1.41 during introduction, as we assume demand and manufacturing volume would be low, and this price would gradually fall to US$0.80 as demand increases.
The total cost of distributing the condoms was calculated as the sum of the program costs per condom and price per condom multiplied by the number of condoms distributed (100,000).
We report the estimated numbers of pregnancies and DALYs averted when the Woman’s Condom is used as a family planning method. For the potential impact as an HIV prevention method, we report the estimated HIV infections and DALYs averted. We calculated the costs per DALY averted by dividing the total costs by the estimated number of DALYs averted for each country. We present the cost per DALY averted using the low-volume price (US$1.41 per condom) and high-volume price (US$0.80). We estimated the cost per DALY averted from dual use of the condom.
We also report the estimated direct health care costs saved, which is an output from the Impact 2 model. These direct health care costs saved are an estimate of the money that would have been spent by the health care system for pregnancy care, safe delivery, and treatment of complications if the pregnancy had occurred. Prevention of HIV also averts medical costs for the diagnosis and management of HIV. We used published data on the average costs of antiretroviral therapy (ART) to estimate the costs that could be saved by using the Woman’s Condom as an HIV prevention method. We assumed that ART costs $839 per patient-yearCitation14 and assumed that an HIV-infected person remains on treatment for 5 years, a conservative estimate. We also explored the impact if each person remained on treatment for 10 years. We then estimated the net costs (total costs less the health care costs saved) and re-estimated the cost per DALY averted.
Our comparator for the cost-effectiveness analysis was no contraceptive use. All costs were reported in 2012 US$. We also obtained per capita gross domestic product (GDP) for each countryCitation15 and used this to benchmark the estimated cost per DALY averted, as per the World Health Organization CHOosing Interventions that are Cost-Effective (WHO-CHOICE) criteria.Citation16 The criteria states that an intervention can be considered as very cost-effective if the estimated cost per DALY averted is less than the per capita GDP, cost-effective if this ratio is between one and three times the per capita GDP, and not cost-effective if it is equal to or greater than three times the per capita GDP.
Results
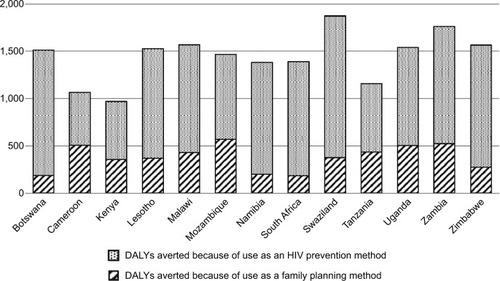
We estimated that programming the distribution of 100,000 Woman’s Condoms in each country during a 1-year period could potentially prevent 194 pregnancies and prevent an average of 21 HIV infections in each of these countries. The country-specific estimates of the DALYs averted for each use are shown in . The estimated DALYs averted because of the use of the Woman’s Condom as a family planning method ranged from 182 in South Africa to 569 in Mozambique, while for its use as an HIV prevention method, the estimates ranged from 558 for Cameroon to 1,499 for Swaziland. A total of approximately 19,000 DALYs could be averted because of the dual use of the Woman’s Condom in these 13 countries, of which 74% of the DALYs averted could be due to use as an HIV prevention method. Given that all the countries included in the analysis have relatively high HIV prevalence rates, the impact of the Woman’s Condom as an HIV prevention method is higher than its impact as a family planning method.
Figure 1 Estimated health impact from distributing 100,000 Woman’s Condoms in each country.
For the low-volume scenario, which assumes that the price for each condom is US$1.41, the estimated cost per DALY averted ranged from US$146 for Zimbabwe to US$303 for Mozambique, as shown in . As expected, with the lower price associated with higher volumes, the condom becomes more cost-effective, and we estimated that the cost per DALY averted for dual use would range from US$107 to US$261. Using the WHO-CHOICE criteria, the Woman’s Condom is very cost-effective in all of the 13 countries for both the low- and high-volume pricing scenarios because the estimated costs per DALY averted are less than the GDP per capita for all of these countries.
Table 2 Estimated costs and cost per DALY averted for the low- and high-volume scenarios
presents the estimated direct health care costs that the health care systems could potentially save by distributing 100,000 condoms as a family planning method. From the 194 pregnancies that could be prevented in each country, we estimated that they would save between US$13,000 and US$19,000 in health care costs in each country. Averting the average of 21 HIV infections could save approximately US$46,000–126,000 in treatment costs in each country.
Table 3 Estimated health care system costs saved and cost per DALY averted
As expected, when we estimated the cost per DALY averted using the net costs as the numerator, this made the program even more cost-effective (). Using net costs reduced the cost per DALY averted by at least one-third when compared to the costs per DALY averted when not incorporating these health care cost savings. Also, if we assumed that a person remains on ART treatment for 5 years, we found that the Woman’s Condom distribution program is highly cost-effective in all countries, and if we assumed that a person remained on ART treatment for 10 years, then the Woman’s Condom would be cost saving in five of the countries (net costs are negative, ie, the cost savings exceed the sum of the program costs and cost of goods).
Discussion
This is the first use of publicly available models to estimate the potential health impact and cost-effectiveness of the dual use of the Woman’s Condom. No previously published analyses have explored the cost-effectiveness of the female condom from the dual protection perspective. The results of this analysis suggest that the Woman’s Condom can be cost-effective and, as such, offers a viable option for couples who wish to protect themselves from unintended pregnancy and sexually transmitted diseases.
Despite their widespread availability and low cost, male condoms are not used as often or consistently as needed, especially among married couples or those in intimate partner relationships. Furthermore, many women are unable to negotiate use of a male condom when her partner refuses. Female condoms offer an alternative, cost-effective option in these cases. Because female condoms are woman initiated, they provide women with a tool to negotiate safer sex. Qualitative studies have shown that some women are able to use the female condom in situations where they cannot negotiate male condom use.Citation17 Moreover, studies in several countries have found that levels of protected sex increase when female condoms are added to the method mix, potentially reducing the risk of HIV infection and unwanted pregnancies. When both types of condoms are available, consistent users often switch between female and male condom use, indicating that female condoms are not a substitute for male condoms but rather a complement.Citation18–Citation24 In other words, the net level of protection achieved by offering the two methods is typically greater than through male condom distribution alone.
Most female condoms are purchased by a few international donors who have great influence on how female condoms are perceived and programmed. Product cost is often cited as a stumbling block to procuring large orders and/or sustaining programs that use female condoms. We are hopeful that the results of this study may assist in alleviating donor concerns about cost as well as support our collective moral obligation to provide protection options for women.
This study has several limitations. First, because we were estimating the impact for multiple countries, we did not develop country-specific models but used models that are publicly available and pre-populated with data. In particular, the Impact 2 model is not preloaded with information on the current methods used in each country; therefore, our analysis assumed that the condoms would be targeted to women who were currently not using any contraceptives. For example, we cannot assume that adding female condoms to an existing hormonal method to ensure protection would still be cost-effective. Second, because the Woman’s Condom is currently being distributed on a limited basis and data from other programs on costs for distributing female condoms are lacking, we used data published by another program that is more than 5 years old. Third, we made simplified assumptions on some data, such as assuming the same costs for ART across all the countries in our sample. These costs may differ by country, but we did not find country-specific data during the literature search. In spite of these limitations, this analysis contributes to the literature as it can be used to inform product introduction decisions and give indications of countries where the product may have the greatest dual impact.
Conclusion
This was a first and successful attempt to estimate the impact of dual protection of female condoms. The Woman’s Condom was found to be very cost-effective in all 13 countries in our sample. The health impact is greater for the use of the Woman’s Condom as an HIV prevention method than for contraception. Dual use of the Woman’s Condom increases the overall health impact.
Acknowledgments
The abstract of this paper was presented at the 2013 International Conference on Family Planning in Addis Ababa, Ethiopia, as a poster presentation with interim findings. The abstract from the poster was published on the International Conference on Family Planning website, available at: http://www.xcdsystem.com/icfp2013/program/index.cfm?aID=2079&seID=413. The actual paper, however, has never been published.
PATH is an international, nonprofit, nongovernmental organization that drives innovation to save lives and improve health, especially among women and children (www.path.org). PATH designed and developed the Woman’s Condom with support from other donors and is the owner of patents for the Woman’s Condom. In 2008, PATH licensed the Woman’s Condom technology for commercialization to Shanghai Dahua Medical Apparatus Co. Ltd.
Disclosure
The authors report no conflicts of interest in this work.
References
- The Partnership for Maternal Neonatal and Child Health (PMNCH)A Global Review of the Key Interventions Related to Reproductive, Maternal, Newborn and Child Health (RMNCH)Geneva, SwitzerlandPMNCH2011 Available from: http://www.who.int/pmnch/topics/part_publications/essential_interventions_18_01_2012.pdfAccessed December 5, 2014
- AccessRH [webpage on the Internet]Review RHInterchange Data: Global and National Contraceptive Order Information Available from: http://www.myaccessrh.org/rhi-homeAccessed December 5, 2014
- DowdyDWSweatMDHoltgraveDCountry-wide distribution of the nitrile female condom (FC2) in Brazil and South Africa: a cost-effectiveness analysisAIDS200620162091209817053355
- MarseilleEKahnJGBillinghurstKSabaJCost-effectiveness of the female condom in preventing HIV and STDs in commercial sex workers in rural South AfricaSoc Sci Med200152113514811144911
- HoltgraveDRMaulsbyCKharfenMCost-utility analysis of a female condom promotion program in Washington, DCAIDS Behav20121651115112022434283
- Johns Hopkins Bloomberg School of Public Health and DC Department of HealthDC Female Condom program highly effective in preventing HIV infections [press release]Washington, DCJohns Hopkins Bloomberg School of Public Health and DC Department of Health2012326
- The World Bank [webpage on the Internet]Prevalence of HIV, total (% of population ages 15–49) Available from: http://data.worldbank.org/indicator/SH.DYN.AIDS.ZSAccessed December 5, 2014
- Marie Stopes International [webpage on the Internet]Impact 2 Available from: http://www.mariestopes.org/impact-2Accessed December 5, 2014
- WeinbergerMPozo-MartinFBolerTFryKHopkinsKImpact 2: An Innovative Tool for Estimating the Impact of Reproductive Health Programmes: Methodology PaperLondon, UKMarie Stopes International2012 Available from: http://mariestopes.org/sites/default/files/Impact%202_Methodology%20and%20Assumptions_(2012%2007%2017)%20FINAL.pdfAccessed December 5, 2014
- Population Services International [webpage on the Internet]Impact Calculator Available from: http://impactcalculator.psi.org/Accessed December 5, 2014
- YangHPSI HIV Heterosexual Transmission Health Impact Estimation Sub-ModelWashington, DCPopulation Services International2008
- MarseilleEKahnJGSmarter Programming of the Female Condom: Increasing Its Impact on HIV Prevention in the Developing WorldFSG2008 Available from: http://www.fsg.org/Portals/0/Uploads/Documents/PDF/Female_Condom_Impact.pdfAccessed December 5, 2014
- Unites States Bureau of Labor Statistics [homepage on the Internet] Available from: www.bls.govAccessed December 5, 2014
- GalarragaOWirtzVJFigueroa-LaraAUnit costs for delivery of antiretroviral treatment and prevention of mother-to-child transmission of HIV: a systematic review for low- and middle-income countriesPharmacoeconomics201129757959921671687
- The World Bank [webpage on the Internet]GDP per capita (current US$) Available at: http://data.worldbank.org/indicator/NY.GDP.PCAP.CDAccessed December 5, 2014
- World Health Organization [webpage on the Internet]Cost effectiveness and strategic planning (WHO-CHOICE) Available at: http://www.who.int/choice/cost-effectiveness/en/Accessed December 5, 2014
- HatzellTFeldblumPJHomanRKGmachRDThe female condom: is “just as good” good enough?Sex Transm Dis200330544044212916136
- HokeTHFeldblumPJVan DammeKTemporal trends in sexually transmitted infection prevalence and condom use following introduction of the female condom to Madagascar sex workersInt J STD AIDS200718746146617623503
- LatkaMGollubEFrenchPSteinZMale-condom and female-condom use among women after counseling in risk-reduction hierarchy for STD preventionSex Transm Dis200027843143710987447
- BarbosaRMBerquoEKalckmannSAcceptability of the Female Condom in Different Social Contexts: Final Research ReportBrasilia, BrazilMinistry of Health, Secretariat for Health Policies, National STD/AIDS Coordinating Office2000
- ArtzLMacalusoMBrillIEffectiveness of an intervention promoting the female condom to patients at sexually transmitted disease clinicsAm J Public Health200090223724410667185
- MacalusoMDemandMArtzLFemale condom use among women at high risk of sexually transmitted diseaseFam Plann Perspect200032313814410894260
- MusabaEMorrisonCSSunkutuMRWongELLong-term use of the female condom among couples at high risk of human immunodeficiency virus infection in ZambiaSex Transm Dis19982552602649587178
- GollubELFrenchPLatkaMRogersCSteinZAchieving safer sex with choice: studying a woman’s sexual risk reduction hierarchy in an STD clinicJ Womens Health Gend Based Med200110877178311703890
