Abstract
Objective
Rebamipide ophthalmic suspension was developed for the treatment of dry eyes and for other corneal diseases, promoting the secretion of both mucin in tear fluid and membrane-associated mucin, increasing the number of goblet cells, and restoring the barrier function of the corneal epithelium. We report a case of a persistent corneal epithelial defect in a patient with diabetes treated with topical application of rebamipide ophthalmic suspension.
Case presentation
A 73-year-old woman had a history of type 2 diabetes for 35 years and nonproliferative diabetic retinopathy for 23 years. She presented to our department with discharge and ophthalmalgia in the left eye. A corneal ulcer was detected, and culture of corneal scrapings was performed, with Staphylococcus aureus and Streptococcus canis being isolated. The infection was treated with levofloxacin eye drops and ofloxacin ophthalmic ointment based on the sensitivity profile of the isolate. However, a corneal epithelial defect persisted for approximately 2 months despite continuing treatment with 0.1% hyaluronic acid ophthalmic suspension and 0.3% ofloxacin eye ointment. Her hemoglobin A1c was 7.3%. The persistent corneal epithelial defect showed improvement at 2 weeks after treatment with rebamipide unit dose 2% ophthalmic suspension, and it did not recur even when vitrectomy was subsequently performed for vitreous hemorrhage due to progression of diabetic retinopathy.
Conclusion
This is the first report about efficacy of rebamipide unit dose 2% ophthalmic suspension for presenting persistent corneal epithelial defect in a patient with diabetes. In the present case, the suggested mechanisms are the following: improving the corneal barrier function, stabilization of mucin on the keratoconjunctival epithelium, and improving the wettability and stability of the tear film, which resulted in the promotion of healing of the corneal epithelial defect in a short time period.
Introduction
Ocular complications of diabetes include diabetic retinopathy, diabetic cataract, diabetic ocular motility disorder, neovascular glaucoma, secondary glaucoma, diabetic optic neuropathy, uveitis, and diabetic keratopathy.Citation1,Citation2 Among them, diabetic keratopathy is unlikely to be associated with irreversible visual impairment, but it can lead to persistent corneal epithelial damage that is difficult to treat.Citation3 Moreover, there is the risk that corneal epithelial disorder could increase susceptibility to bacterial or fungal infections.Citation4 In patients with diabetes, attention must be paid to the general increased risk of infection, which is not only a problem for the eyes.
Rebamipide was developed in the 1990s as an oral agent for the treatment of gastric ulcer and gastritis.Citation5–Citation7 In recent years, its mucosal-protective effect has also been applied to protect the keratoconjunctival epithelium,Citation8,Citation9 following the development of ophthalmic rebamipide products for the treatment of dry eyes.Citation8–Citation11 Rebamipide ophthalmic suspension has been reported to exhibit multiple pharmacological effects, such as promoting the secretion of both mucin in tear fluid and membrane-associated mucin, increasing the number of goblet cells,Citation8,Citation9 restoring the barrier function of the corneal epithelium,Citation12,Citation13 and anti-inflammatory activity.Citation14 It has been reported that rebamipide ophthalmic suspension is effective not only for dry eyes but also for other corneal diseases such as Sjögren’s syndrome,Citation15 persistent corneal erosion,Citation16 superficial limbic keratopathy,Citation17 alkaline corneal injury,Citation18 lid wiper epitheliopathy,Citation19 and lagophathalmos.Citation20 However, no reports have been published concerning the efficacy of rebamipide ophthalmic suspension for persistent corneal epithelial defects associated with diabetic keratopathy. Here, we report a case with persistent corneal epithelial defect after infectious corneal ulcer in a patient with diabetes, which resolved following topical application of 2% rebamipide ophthalmic suspension for ∼2 weeks.
Case presentation
A 73-year-old woman presented to the Department of Ophthalmology of Juntendo University Shizuoka Hospital with a sudden onset of discharge and ophthalmalgia in the left eye. She had a history of type 2 diabetes for 35 years. Hemoglobin (Hb) A1c had ranged between 7.2% and 8.0% in recent years, indicating inadequate glycemic control. Cataract surgery had been performed on both eyes ∼20 years ago. She also had a history of nonproliferative diabetic retinopathy for ∼23 years and had not undergone retinal photocoagulation. Her family history was unremarkable.
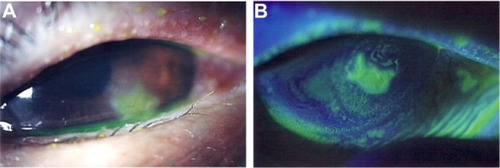
At the first visit to our hospital, a corneal ulcer was noted in the left eye with corneal opacity (). Further, conjunctival injection and chemosis and/or conjunctivochalasis on the lower part of burbar conjunctiva were observed. Infectious corneal ulcer was then diagnosed. Funduscopy revealed mild retinal punctate hemorrhages in both eyes due to nonproliferative diabetic retinopathy. Corrected visual acuity was 14/20 and 16/20 in the right and left eyes, respectively. Topical application of 1.5% levofloxacin (LVFX) antimicrobial eye drops (Cravit® ophthalmic solution 1.5%; Santen Pharmaceutical Co. Ltd, Osaka, Japan) four times daily was commenced together with 0.3% ofloxacin ophthalmic ointment (Tarivid® ophthalmic ointment 0.3%; Santen Pharmaceutical Co. Ltd) twice daily. Cefdinir capsules (Cefzon; Astellas Pharmaceutical Co. Ltd, Tokyo, Japan) were also administered orally (100 mg three times daily for 3 days). Staphylococcus aureus and Streptococcus canis were isolated by culture of corneal scrapings, and both of these bacteria were found to be sensitive to LVFX. At the first hospital visit, HbA1c was 7.3%. Tear secretion was evaluated at 12 mm in the right eye and 11 mm in the left eye by Schirmer’s tear test. Tear breakup time in both eyes was 4 seconds.
Figure 1 Slit lamp microscopic images of the left eye at the time of the initial presentation.
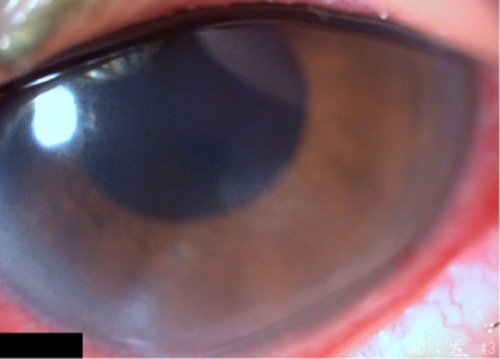
At 2 weeks after the start of treatment, there were no signs of infection, the corneal ulcer reduced, and her symptoms of eye discharge and the ophthalmalgia resolved. In contrast, clinically a lesion of corneal epithelial defect ∼1 mm in size was still noted. Even though additional administration of 0.1% hyaluronic ophthalmic suspension (Hyalein® ophthalmic solution 0.1%; Santen Pharmaceutical Co. Ltd) six times daily, the corneal epithelial defect persisted (). We diagnosed persistent corneal epithelial defect associated with diabetes as well as corneal hypoesthesia and diabetic keratitis. Vitreous hemorrhage occurred in the left eye ∼2 months after the start of treatment, and visual acuity decreased from 16/20 to 8/20. The patient required vitrectomy, but it could not be done until the corneal epithelial defect healed. Accordingly, she was treated with 2% rebamipide ophthalmic suspension (Mucosta ophthalmic suspension unit dose 2%; Otsuka Pharmaceutical Co. Ltd, Tokyo, Japan) four times daily, and the corneal epithelial defect healed after 2 weeks. Vitrectomy was then performed, and administration of this drug was discontinued after vitrectomy, while LVFX eye drops and 0.1% betamethasone ophthalmic suspension were used. After surgery, any corneal epithelial defect did not recur after surgery (), and her corrected visual acuity had recovered to 16/20 at 3 months after surgery.
Figure 2 Slit lamp images from 2 months after the start of treatments.
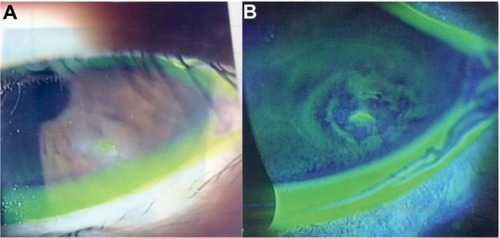
Figure 3 Slit lamp image from 3 weeks after the start of treatments with Mucosta ophthalmic suspension.
Discussion
In patients with a persistent corneal epithelial defect, a corneal epithelial lesion caused by trauma or surgery fails to heal. It is often difficult to treat, and patients may have underlying diseases such as diabetes, corneal neuropathy, or corneal epithelium adhesion factor disorder.Citation21 A persistent corneal epithelial defect is generally treated by topical application of artificial tears, hyaluronic acid, and ophthalmic ointment, wearing a therapeutic soft contact lens, or topical application of serum.Citation22,Citation23 However, the defect is often refractory to these treatments. Use of fibronectin or peptide has also been investigated by some researchers, but these agents are not available yet clinically.Citation21,Citation24 The risk of infection is increased, particularly when the patient has diabetes.Citation4 In the present patient, bacterial infection could have occurred due to a corneal epithelial disorder related to poor glycemic control, and a persistent corneal epithelial defect was noted after treatment of the infection. Diabetic keratopathy may be associated with neuropathic keratitis in patients with a persistent corneal epithelial defect, and dry eyes may occur secondary to a reflex decrease of tear secretion due to corneal hypoesthesia and/or secondary to reduced tear and mucin secretion due to efferent nerve dysfunction.Citation25 Tear secretion was not decreased in this patient, but there was a possibility of other neurological dysfunction. The development of diabetic keratopathy has been also suggested to be related to loss of nerve-derived trophic factors following a decrease in corneal sensation. Furthermore, there was another possibility of dysfunction of the tear meniscus and/or an ectopic tear meniscus by conjunctivochalasis or chemosis as shown in and . It might bring disturbance of stability of the tear film as described in the previous reportCitation26 and lead to persistent corneal epithelial defect.
In this patient, a persistent corneal epithelial defect that was refractory to standard treatment resolved after ∼2 weeks of topical therapy with rebamipide ophthalmic suspension and did not recur when vitrectomy was performed subsequently. During the follow-up period, HbA1c ranged between 6.7% and 7.3%, showing little fluctuation. The main pharmacological effects of rebamipide ophthalmic suspension include promoting the secretion of mucin in tears and membrane-associated mucin, increasing the number of goblet cells, and restoring the barrier function of the corneal epithelium by increasing the expression of tight junction proteins, as well as an anti-inflammatory effect.Citation8–Citation14 Such actions could have been exhibited in this patient with diabetic keratopathy. In brief, as a result of junctions between corneal epithelial cells being strengthened to improve corneal barrier function, mucin was stabilized on the corneal epithelium, and this improved the wettability and stability of the tear film, resulting in promotion of healing of the corneal epithelial defect. It has also been reported that inflammation occurs due to oxidative stress and increased expression of nuclear factor-kappa B in diabetic keratopathy.Citation27 Rebamipide has been reported to have an anti-inflammatory effect and to inhibit the production of interleukin-6, interleukin-8, and tumor necrosis factor-α by human corneal epithelial cells,Citation12–Citation14 so these anti-inflammatory effects would also lead to improvement of persistent corneal epithelial defect.
Conclusion
Rebamipide ophthalmic suspension exhibited a beneficial effect on a presenting persistent corneal epithelial defect in a patient with diabetes relatively soon after the start of treatment.
Acknowledgments
The institutional review board at Juntendo University Shizuoka Hospital did not require the authors to obtain ethics approval and patient consent, following “Ethical Guidelines for Medical and Health Research Involving Human Subjects” established by the Ministry of Education, Culture, Sports, Science and Technology and the Ministry of Health, Labour and Welfare.Citation28 Written informed consent was obtained from the patient before the patient received vitrectomy.
Disclosure
The authors report no conflicts of interest in this work.
References
- RecchiaFMConnollyBBensonWEOcular manifestations of diabetesCurr Opin Ophthalmol199896646810387338
- StangaPEBoydSRHamiltonAMOcular manifestations of diabetes mellitusCurr Opin Ophthalmol199910648348910662255
- KajiYPrevention of diabetic keratopathyBr J Ophthalmol200589325425515722297
- DeMillDLHussainMPop-BusuiRShteinRMOcular surface disease in patients with diabetic peripheral neuropathyBr J Ophthalmol Epub20151023
- UchidaMTabusaFKomatsuMMoritaSKanbeTNakagawaKStudies on 2(1H)-quinolinone derivatives as gastric antiulcer active agents. 2-(4-Chlorobenzoylamino)-3-[2(1H)-quinolinon-4-yl] propionic acid and related compoundsChem Pharm Bull (Tokyo)1985339377537864092279
- YamasakiKKanbeTChijiwaTIshiyamaHMoritaSGastric mucosal protection by OPC-12759, a novel antiulcer compound, in the ratEur J Pharmacol1987142123293480223
- KleineAKlugeSPeskarBMStimulation of prostaglandin biosynthesis mediates gastroprotective effect of rebamipide in ratsDig Dis Sci1993388144114498393757
- UrashimaHOkamotoTTakejiYShinoharaHFujisawaSRebamipide increases the amount of mucin-like substances on the conjunctiva and cornea in the N-acetylcysteine-treated in vivo modelCornea200423661361915257002
- RíosJDShatosMUrashimaHTranHDarttDAOPC-12759 increases proliferation of cultured rat conjunctival goblet cellsCornea200625557358116783146
- KinoshitaSAwamuraSOshidenKRebamipide Ophthalmic Suspension Phase II Study GroupRebamipide (OPC-12759) in the treatment of dry eye: a randomized, double-masked, multicenter, placebo-controlled phase II studyOphthalmology2012119122471247823009892
- KinoshitaSOshidenKAwamuraSRebamipide Ophthalmic Suspension Phase 3 Study GroupA randomized, multicenter phase 3 study comparing 2% rebamipide (OPC-12759) with 0.1% sodium hyaluronate in the treatment of dry eyeOphthalmology201312061158116523490326
- TanakaHFukudaKIshidaWHaradaYSumiTFukushimaARebamipide increases barrier function and attenuates TNFα-induced barrier disruption and cytokine expression in human corneal epithelial cellsBr J Ophthalmol201397791291623603753
- KimuraKMoritaYOritaTHarutaJTakejiYSonodaKHProtection of human corneal epithelial cells from TNF-α-induced disruption of barrier function by rebamipideInvest Ophthalmol Vis Sci201354427522760
- ArakakiREguchiHYamadaAAnti-inflammatory effects of rebamipide eyedrop administration on ocular lesions in a murine model of primary Sjögren’s syndromePLoS One201495e9839024866156
- ArimotoAKitagawaKMitaNTakahashiYShibuyaESasakiHEffect of rebamipide ophthalmic suspension on signs and symptoms of keratoconjunctivitis sicca in Sjögren syndrome patients with or without punctal occlusionsCornea201433880681124977983
- KashimaTAkiyamaHMiuraFKishiSResolution of persistent corneal erosion after administration of topical rebamipideClin Ophthalmol201261403140622969286
- TakahashiYIchinoseAKakizakiHTopical rebamipide treatment for superior limbic keratoconjunctivitis in patients with thyroid eye diseaseAm J Ophthalmol2014157480781224412123
- SasakiHKokubunTAlkali burn treated with 2% rebamipide ophthalmic suspension: a case reportCase Rep Ophthalmol20145338038525762927
- ItakuraHKashimaTItakuraMAkiyamaHKishiSTopical rebamipide improves lid wiper epitheliopathyClin Ophthalmol201372137214124204116
- ItakuraMItakuraHKashimaTAkiyamaHKishiSTopical rebamipide improves the ocular surface in mild lagophthalmosClin Ophthalmol201371333133823836962
- WirostkoBRafiiMSullivanDAMorelliJDingJNovel therapy to treat corneal epithelial defects: a hypothesis with growth hormoneOcul Surf201513320421226045234
- KanpolatAUçakhanOOTherapeutic use of Focus Night and Day contact lensesCornea200322872673414576523
- TsubotaKGotoEShimmuraSShimazakiJTreatment of persistent corneal epithelial defect by autologous serum applicationOphthalmology1999106101984198910519596
- MoritaYMorishigeNYamadaNOhtaMSonodaKHNishidaTRecovery of the corneal stroma associated with rapid reepithelialization induced by the fibronectin-derived peptide PHSRN in 2 cases of corneal perforation due to a persistent epithelial defectCornea201534111504150726312620
- ToshidaHNguyenDHBeuermanRWMurakamiAEvaluation of novel dry eye model: preganglionic parasympathetic denervation in rabbitInvest Ophthalmol Vis Sci200748104468447517898267
- YokoiNInatomiTKinoshitaSSurgery of the conjunctivaDev Ophthalmol20084113815818453766
- KimJKimCSSohnEJeongIHKimHKimJSInvolvement of advanced glycation end products, oxidative stress and nuclear factor-kappaB in the development of diabetic keratopathyGraefes Arch Clin Exp Ophthalmol2011249452953621104267
- Ethical Guidelines for Medical and Health Research Involving Human Subjects Provisional Translation (as of March 2015)Ministry of Education, Culture, Sports, Science and Technology; Ministry of Health, Labour and WelfareJapan Available from: http://www.lifescience.mext.go.jp/files/pdf/n1500_01.pdfAccessed April 21, 2016
