Abstract
Purpose
To report a case of a patient with ischemic retinopathy associated with Crohn’s disease.
Case report
This report presents a case of a 28-year-old female patient with Crohn’s disease and sudden decrease of visual acuity in the right eye. Fluorescein angiography, optical coherence tomography, and multifocal electroretinography confirmed the clinical features of ischemic retinopathy. After systemic corticosteroid treatment, the patient developed epiretinal membrane without significant improvement in visual acuity.
Discussion
The patient presented with ischemic retinopathy associated with Crohn’s disease with deficiency of central visual acuity. Periodic examination by a retina specialist is recommended for patients being treated for Crohn’s disease.
Introduction
Crohn’s disease (CD) is a regional enteritis that affects the terminal ileum, but has the potential of involving any segment of the gastrointestinal tract of the patient.
The etiology of CD is unknown, but several proven risk factors exist such as family history, smoking, oral contraceptives, diet, and ethnicity. The combination of risk factors, and aberrant autoimmune response in the intestinal mucosa with endothelial dysfunction lead to digestive tract malfunctioning. The current treatment is not ideal. Therapy generally involves steroids and antitumor necrosis factor alpha blockers but about one-third of patients fail to respond (primary nonresponders) and 10% of patients do not tolerate or are primary nonresponders to all drugs used. One-third of responders to antitumor necrosis factor treatment show transient loss of response (secondary nonresponders). Severe cases may require partial resection of a segment of bowel, possibly total colectomy with the placement of stoma bags for feces when the disease affects the rectum.
Ophthalmic manifestations have been reported to occur in up to 12% of patients with CD and most of them include iritis, uveitis, episcleritis, and conjunctivitis. However, posterior segment manifestations are very rare, occurring in less than 1% of patients.Citation1–Citation4
Case report
A 28-year-old female was admitted because of sudden decrease of visual acuity in the right eye. She had been diagnosed as suffering from CD. She had undergone resection of a 40 cm segment of bowel due to stenosis. She was refractory to treatment using corticosteroids, azathioprine, infliximab, and adalimumab. The patient suffered repeated episodes of abdominal pain, mucous bloody diarrhea, weight loss, and depression.
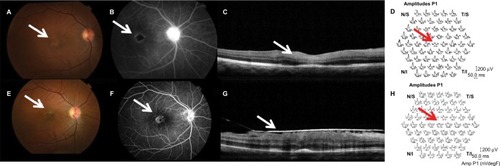
At presentation, she underwent a complete ophthalmological examination. Visual acuity was 20/400 in the right eye. Examination of the anterior segment was normal and the lens was clear. Bilateral intraocular pressure was 13 mmHg. Ophthalmoscopic examination with mydriasis showed severe ischemic retinopathy in the right eye (). Retinal fluorescein angiography showed ischemic retinopathy, especially involving the macular area (). Optical coherence tomography showed thickening and hyperreflectivity of the inner retinal layers, including the nerve fiber and ganglion cell layers owing to ischemia of the superficial capillary plexus () and multifocal electroretinography showed a decrease of electrical responses representing central macula ().
Figure 1 Evaluation of anatomical and functional status before and after treatment using FA, OCT, and ERG.
Notes: (A) Ischemic retinopathy with alteration of foveal reflex (arrow) in the right eye. (B) Retinal FA showing ischemic retinopathy, especially involving the macular area (arrow). (C) OCT showed thickening and hyperreflectivity of the inner retinal layers (arrow). (D) Multifocal ERG showed a decrease in electrical responses from central macula (arrow). (E) Resolution of cotton wool spots (arrow). (F) Reperfusion of some previously ischemic areas during examination with fluorescein (arrow). (G) OCT showed formation of epiretinal membrane (arrow). (H) Multifocal ERG remained at low amplitudes corresponding to central area (arrow), indicating macular dysfunction.
These features suggested the clinical diagnosis of ischemic retinopathy secondary to CD.
We prescribed prednisone 60 mg daily and scheduled new follow-up tests.
Visual acuity showed a slight improvement (20/150), with resolution of cotton wool spots () and reperfusion of some previously ischemic areas during examination with fluorescein (). After 3 months, we observed the formation of an epiretinal membrane (), but without significant macular edema or bleeding. Multifocal electroretinography remained at low amplitudes meaning macular dysfunction ().
Discussion
We present a case of CD complicated by ischemic retinopathy with irreversible damage of central visual acuity.
Several factors are associated with an increased risk of ocular manifestations. Patients with colitis and ileocolitis tend to have a higher risk of ocular involvement compared to those with ileitis alone.Citation5 Presence of other organ involvement also increases the risk.Citation5,Citation6 Particularly, in patients with CD and arthralgia, the risk of ocular involvement increases to 33%.Citation6
Falavarjani et alCitation7 described a 9-year-old male with biopsy-proven CD who developed a cilioretinal artery-sparing central retinal artery occlusion. Trojet et alCitation8 reported a 55-year-old male with CD with associated retinal vasculitis involving the veins, papillitis, cystoid macular edema.
The pathophysiology of the extraintestinal manifestations of CD is not well understood, but it is most likely mediated by the inflammatory nature of the disease. Several proposed mechanisms include circulating antigen–antibody complexes or autoantibody production against cellular antigens shared by the colon and extraintestinal organs.Citation9 Inflammation causing damage to mucosa of the intestinal epithelium may allow proteins or microorganisms to pass through the intestinal barrier and cause a reactive lymphoid tissue response. This, in turn, results in antibody production or antigen–antibody complexes that circulate in the body and cause systemic inflammation. This immune response to a colonic antigen may explain why ocular manifestations may occur more commonly with colitis and ileocolitis than with small bowel involvement alone. Microbial pathogens, through molecular mimicry, may also contribute to the pathogenesis, though this is still being investigated. Genetic factors may also play a role in ocular manifestations. Patients with extraintestinal manifestations of CD have a higher prevalence of HLA-B27 type leukocytes than the regular.Citation10
Ocular complications are categorized as primary, secondary, and coincidental.Citation11 Primary complications are temporally associated with CD exacerbations and tend to resolve with systemic treatment of the intestinal inflammation. These include keratopathy, episcleritis, and scleritis. Secondary complications arise from primary complications. Examples include cataract formation due to treatment with corticosteroids, scleromalacia due to scleritis, and dry eye due to hypovitaminosis A following gut resection. Coincidental complications occur commonly in the general population and cannot be correlated to inflammatory bowel disease alone. These include conjunctivitis, recurrent corneal erosions, and corneal ulcer.Citation11–Citation13
Ocular involvement does not always coincide with active intestinal flare. However, in instances when it does, as is typical of episcleritis, this can be used as an indicator of disease activity, indicating the need for more aggressive management.Citation12
In this case report, the pathogenesis of ischemia in retinal vasculitis is not clear but is suggested to be either thrombotic or obliterative, secondary to the infiltration of inflammatory cells. Based on histological studies, vascular changes in uveitis are characterized by perivascular infiltration of lymphocytes, which results in perivasculitis rather than true vasculitis of the vessel wall.Citation14 Cell-mediated immunity also plays a role in the pathology of retinal vasculitis, with CD4+ T cells documented within and around the retinal vessels. Thrombotic vascular changes can occur due to local endothelial injury or increased prothrombin activity as observed in Behçet’s disease.Citation14,Citation15 The retina has a uniquely high metabolic demand for oxygen that is normally met by a highly efficient vascular supply. Insufficiency of the retinal circulation causes neuroretinal dysfunction and degeneration. Focal retinal ischemia results in selective damage to specific subpopulations of retinal neurons and can result in cellular death by apoptosis or necrosis, with dysfunction and degeneration of the inner retina and eventually visual loss. Retinal vascular obstruction can also promote the production of vascular endothelial growth factor, which increases vascular permeability and results in macular edema and induced neovascularization.Citation15,Citation16
Treatment of ocular manifestations ranges from controlling the underlying intestinal inflammation, topical steroids, systemic nonsteroidal anti-inflammatory drugs, systemic steroids, and immunosuppressant and biological agents. In refractory or severe cases, treatment with monoclonal antibodies has shown promise.
Periodic examination by a retina specialist is recommended for patients being treated for CD.
Acknowledgments
This study was approved by ethics committee of the Beneficencia Portuguesa Hospital in Sao José do Rio Preto, Sao Paulo, Brazil. The patient signed the consent form in the Bone Marrow Transplant Unit of the Beneficencia Portuguesa Hospital of São José do Rio Preto which is accredited by the National Transplant System of the Ministry of Health of Brazil. The consent forms are reviewed and approved by the ethics committee of the Beneficencia Portuguesa Hospital which is accredited by the National Committee of Ethics and Research in Brazil.
Disclosure
The authors report no conflicts of interest in this work.
References
- AbrahamCChoJHInflammatory bowel diseaseN Engl J Med2009361212066207819923578
- KallaRVenthamNSatsangiJArnottICrohn’s disease-clinical reviewBMJ2014349g667025409896
- TaylorSRMcCluskeyPLightmanSThe ocular manifestations of inflammatory bowel diseaseCurr Opin Ophthalmol200617653854417065922
- ZippiMCorradoCPicaRExtraintestinal manifestations in a large series of Italian inflammatory bowel disease patientsWorld J Gastroenterol20142046174631746725516659
- SalmonJFWrightJPMurrayADOcular inflammation in Crohn’s diseaseOphthalmology1991984804842052301
- FelekisTKatsanosKKitsanouMSpectrum and frequency of ophthalmologic manifestations in patients with inflammatory bowel disease: a prospective single-center studyInflamm Bowel Dis2009151293418626979
- FalavarjaniKGParvareshMMShahrakiKNekoozadehSAmirfar-hangiACentral retinal artery occlusion in Crohn diseaseJ AAPOS201216439239322824494
- TrojetSMazloutHHamdouniMRetinal vasculitis in Crohn’s disease: a case reportJ Fr Ophtalmol201033154.e15520022662
- DasKMRelationship of extraintestinal involvements in inflammatory bowel disease: new insights into autoimmune pathogenesisDig Dis Sci19994411139952216
- MallasEGMackintoshPAsquithPCookeWTHistocompatibility antigens in inflammatory bowel disease; their clinical significance and their association with arthropathy with special reference to HLA B27 (W27)Gut197617119069101001980
- AkpekEKThorneJEQaziFADoDVJabsDAEvaluation of patients with scleritis for systemic diseaseOphthalmology2004111350150615019326
- KnoxDLSchachatAPMustonenEPrimary, secondary and coincidental ocular complications of Crohn’s diseaseOphthalmology19849121631736538677
- MadyRGroverWButrusSOcular complications of inflammatory bowel diseaseScientific World J20152015438402
- HughesEHDickADThe pathology and pathogenesis of retinal vasculitisNeuropathol Appl Neurobiol200329432534012887593
- TalatLLightmanSTomkins-NetzerOIschemic retinal vasculitis and its managementJ Ophthalmol2014201419767524839552
- PalmerHEStanfordMRSandersMDGrahamEMVisual outcome of patients with idiopathic ischaemic and non-ischaemic retinal vasculitisEye (Lond)19961033433488796160
