Abstract
Introduction
The complications of HIV/AIDS can produce grossly abnormal pathology. In low-resourced settings, women can present late with huge lesions. Massive vulval pathology copresenting in pregnancy produces difficulties in managing the patients and may lead to poor maternal or fetal outcomes.
Case report
A 27-year-old P1 G2 (second pregnancy one live birth) patient presented at 30 weeks gestation with a massive vulval lesion. She was HIV seropositive and taking anti-retroviral therapy. She was anemic with a hemoglobin level of 5.9 and was transfused 4.0 of packed cells. She underwent examination under anesthesia and vulval biopsy. She went into preterm labor and was delivered by cesarean section. Unfortunately, the baby had died while receiving corticosteroid therapy. The histopathological report confirmed a Kaposi’s sarcoma, and she was referred to oncologists for chemotherapy.
Conclusion
Kaposi’s sarcoma can occur in pregnancy in both seropositive and seronegative patients. Kaposi’s sarcoma causes significant fetal and maternal health complications.
Introduction
This is the first time a case of vulval Kaposi’s sarcoma in pregnancy has been described in the literature. Kaposi’s sarcoma is an opportunistic tumor that develops with increased frequency (100,000-fold) after HIV infection.Citation1 It is one of the commonest cancers in HIV-infected patients.Citation2 Herpes virus also known as herpes virus 8 is a tumorigenic casual agent of Kaposi’s sarcoma.Citation2–Citation4
Case report
A 27-year-old P1 G2 (second pregnancy one live birth) patient presented at 30 weeks gestation with a massive vulval lesion. The lesion had been present since the past year in a smaller form. She said that it had rapidly progressed within the last 2 months to a massive form. She was HIV seropositive and taking antiretroviral therapy. Her last CD4 count was 107 cells/mm3. She was able to pass stool and urine but complained of vulval pain and discomfort.
On examination, she was found to have a huge foul-smelling vulval mass. The mass was occupying the whole vulva, perineum, and anal region. The mass was partly necrotic and with vesicular round lesions. The perineal organs were not visible. There were no other suspicious lesions seen in her mouth or skin. She was pale, with a gravid uterus of 30 weeks gestation and a positive fetal heart by Pinard auscultation. There were no other alternative instruments for fetal heart rate monitoring in this low-resourced clinical setting. The use of electronic fetal heart rate monitoring is yet to be introduced in these settings.
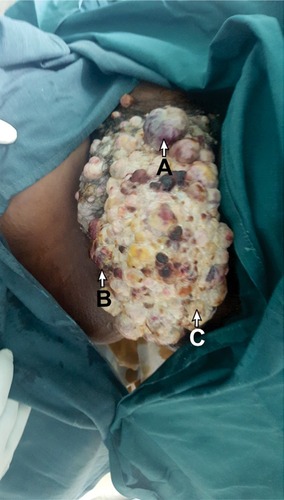
The investigations done showed an Hb of 5.9 g/dL, white blood cell of 7.29×109/L, and platelet count 144×109/L. The repeat CD4 count was 345 cells/mm3. An ultrasound scan showed a live fetus of 29 weeks 6 days gestation. She was transfused 4.0 units of packed cells. The posttransfusion Hb was 9.7. The chest X-ray was normal. She underwent examination under anesthesia and vulval biopsy. The findings observed in the operation theater can be seen in . There was palpable bilateral lymphadenopathy. The urethra was not visible. There were no areas that appeared to be infested around the lesion. The plan was to deliver her by cesarean section after giving her corticosteroid treatment for lung maturation. This mode of delivery was the better one as achieving a normal delivery would be difficult.
Figure 1 A photo taken during examination under anesthesia showing a massive vulval mass.
She was referred to oncologists for chemotherapy. She went into preterm labor and was delivered by cesarean section. Unfortunately, the baby had died while receiving corticosteroid therapy for fetal lung maturation. The baby’s birth weight was 1,300 g. No postmortem examination for the baby was done. She had wound sepsis, which was treated with intravenous broad-spectrum antibiotics. Postoperatively she recovered well. The histopathological report described “proliferating vasoformative spindle cells with red cell extravasation exhibiting a sieve-like pattern, features consistent with Kaposi’s sarcoma”. There are no facilities for testing for herpes virus 8 in this low-resourced setting. The placenta did not undergo virology or histological testing. The patient was referred to oncologists for chemotherapy, where is undergoing their care. Written informed consent was obtained from the patient.
Discussion
Kaposi’s sarcoma causes significant morbidity from mucocutaneous involvement and mortality from complications of visceral sites of disease such as the gastrointestinal tract and liver.Citation1 In pregnancy, it compromises both maternal and fetal health, leading to poor or adverse outcomes.
Kaposi’s sarcoma has been described in pregnancy to be occurring in the lungCitation5,Citation6 and trachea.Citation7 It can present as skin lesions, lymphadenopathy, or respiratory compromise.Citation5–Citation7 There have been rare cases of HIV-seronegative patients with Kaposi’s sarcoma.Citation8
The treatment for Kaposi’s sarcoma is chemotherapy, and the tumor is potentially responsive.Citation6 Patients with advanced disease such as widespread mucocutaneous disease, lymphedema, and visceral involvement are treated most effectively with cytotoxic agents.Citation1 Cytotoxic agents used include a combination of doxorubicin, bleomycin, and vinblastine, which have been given during pregnancy, resulting in a live growth-restricted baby.Citation9 Conservative management has also been described with good outcomes.Citation10 A rare case of Kaposi’s sarcoma in a 2-week-old infant born to a mother with Kaposi’s sarcoma/AIDS has been reported in the literature.Citation11 Kaposi’s sarcoma in an HIV-seropositive patient presenting as a massive vulval mass in pregnancy complicates the pregnancy, even further affecting the vaginal mode of delivery. A cesarean section being done with a dirty vulva risks complicating with sepsis as happened in this case.
Conclusion
Kaposi’s sarcoma can occur in pregnancy in both seropositive and seronegative patients. Therefore, any suspicious lesions must have early recourse to a biopsy to obtain histopatho-logical diagnosis and early treatment. Kaposi’s sarcoma causes significant fetal and maternal health complications. In low-resourced settings, when the clinician is faced with a heavy disease burden, with little recourse to advanced medical equipment, the only target remains to prevent maternal morbidity and mortality.
Disclosure
The author reports no conflicts of interest in this work.
References
- McGarveyMETulpuleACaiJEmerging treatments for epidemic (AIDS related) Kaposi’s sarcomaCurr Opin Oncol19881054134219800111
- BagniRWhitbyDKaposi’s sarcoma-associated herpes virus transmission and primary infectionCurr Opin HIV AIDS200941222619339936
- GoedertJJCharuratMBlattnerWARisk factors for Kaposi’s sarcoma-associated herpes virus infection amongst HIV-1 infected pregnant women in the USAAIDS200317342543312556697
- SitasFNewtonRKaposi’s sarcoma in South AfricaJ Natl Cancer Inst Monogr2001281411158199
- PantanowitzLDezubeBJKaposi’s sarcoma and pregnancyAm J Perinatol200522845716283606
- BryantAEGencMHurtadoRMChenKTPulmonary Kaposi’s sarcoma in pregnancyAm J Perinatol200421635536315311373
- RajaratnamKDesaiSKaposi’s sarcoma of the tracheaJ Laryngol Otol1988102109519533199020
- Brunet-PossentiFPagesCRouzierRDupinNBagotMLebbeCKaposi’s sarcoma and pregnancy: case report and literature reviewDermatology2013226431131423838298
- RawlisonKFZubrowABHarrisMAJacksonUCChaoSDisseminated Kaposi’s sarcoma in pregnancy: a manifestation of acquired immune deficiency syndromeObstet Gynecol1984633 suppl2S6S6700876
- AdeyemoAWoodCGovindAKaposi’s sarcoma in pregnancy after initiation of highly active antiretroviral therapy: a manifestation of immune reconstitution syndromeInt J STD AIDS2012231290590623258835
- McCartyKABunguZKaposi’s sarcoma in a two week old infant born to a mother with Kaposi’s sarcoma/AIDSCent Afr J Med199541103303318556781
