Abstract
Background
Nowadays, dislocated intraocular lenses (IOLs) and inadequate capsular support are becoming a challenge for every ophthalmic surgeon. Explantation of dislocated IOL and iris claw IOL (ICIOL) are the techniques that have been used in our ophthalmic department. The aim of this study is to report our technique for retropupillar ICIOL.
Methods
This study is a retrospective case series. A total of 105 eyes with dislocated IOL from the patients at the Department of Ophthalmology in Santa Maria Hospital, a tertiary reference hospital in Lisbon, Portugal, from January 2012 until January 2016, had been analyzed. Of these 105 eyes, 66 eyes had dislocated one-piece IOL and 39 eyes had dislocated three-piece IOL. The latter underwent iris suture of the same IOL and were excluded from this study. The remaining 66 eyes with dislocated one-piece IOL underwent pars plana vitrectomy, that is, explantation of dislocated IOL through corneal incision and an implantation of retropupillary ICIOL. Operative data and postoperative outcomes included best corrected visual acuity, IOL position, intraocular pressure, pigment dispersion, clinical signs of endothelial cell loss, and anterior chamber depth.
Results
The mean follow-up was 23 months (range: 6–48 months). The mean preoperative best corrected visual acuity was 1.260±0.771 logMAR, and postoperative best corrected visual acuity was 0.352±0.400 logMAR units. Mean vision gain was 0.909 logMar units. The patients had the following complications: 1) retinal detachment was found in one patient, 2) corneal edema was found in three patients, 3) high intraocular pressure was observed in twelve patients, 4) subluxation of the IOL was observed in one patient, and 5) macular edema was found in three eyes.
Conclusion
The results demonstrate that retropupillary ICIOL is an easy and effective method for the correction of aphakia in patients not receiving capsule support. The safety of this procedure must be interpreted in the context of a surgery usually indicated in complicated cases.
Introduction
It is well known that worldwide phacoemulsification is one of the most frequent eye surgeries and that intraoperative and postoperative complications have been reduced compared to large-incision extracapsular cataract extraction.Citation1
However, as the surgeries are done in a tertiary reference center, patients with complications post-cataract surgery are referred to the center for treatment. In addition, the incidence of dislocated intraocular lenses (IOLs) is likely to increase continuously as the age of the population increases. One of the reasons for this increase is the natural weakness of the lens zonules that occurs with aging. This weakness can be enhanced by a previous history of vitrectomy, ocular trauma, high myopia, pseudoexfoliation syndrome, or uveitis. Another reason is that more patients have undergone cataract surgery earlier in their life as this surgery has become safer and the threshold for intervention has become lower. Therefore, more IOLs must remain in eyes for longer periods than they did earlier.Citation2,Citation3
Surgical approaches that were used to treat dislocated three-piece IOLs that remain in the capsular bag include pars plana vitrectomy with either iris or scleral fixation of the current lens or exchange of the existing IOL for an anterior chamber (AC) or posterior chamber IOL. ACIOLs and iris-fixated IOLs are found to cause intraocular inflammation that is often chronic and the treatment of this inflammation remains a challenge.
Without adequate capsular support, the surgical management of aphakia is often challenging. To date, no optimal surgical approach is available to overcome this problem.Citation4 However, ACIOLs, iris- or scleral-sutured posterior chamber IOL and iris claw IOL (ICIOL) can be used.Citation5
In 1972, Worst et alCitation6 reported the first ICIOL, a biconvex polymethyl methacrylate IOL, fixated at the anterior surface of the iris, at mid-periphery. The Verisyse® IOL for aphakia (VRS54, Abbott Laboratories Inc, Illinois, USA), one of the latest versions of the iris-fixated ACIOL, with a convex–concave design is associated with fewer complications.Citation7 Surgical time is lessened, and this technique has a short learning curve, which results in a good visual outcome and a low incidence of intraoperative and postoperative complications. Classic recommendation is positioning the ICIOL above the iris in the patients with aphakia.Citation5
Over the last decade, ICIOL implantation had more commonly been used. Although originally designed to be fixed on the anterior surface of the iris, some previous case series reported an advantage of fixing the ICIOL in a retropupillary position, namely by maintaining the AC depth and reducing the corneal endothelial cell loss.Citation8
With the advent of 25 and 23 G pars plana vitrectomy, most posterior segment surgeons, in dealing with complications of cataract surgery, late in the bag luxation or even trauma, prefer to position ICIOL in a retropupillary position.
Methods
This study was conducted in accordance with the tenets of the Declaration of Helsinki and was approved by the Ethics Committee of Santa Maria Hospital, and an informed written consent was obtained from all the patients included in this study.
This retrospective study included 66 eyes from the patients who underwent a Verisyse® IOL for aphakia (VRS54) implantation between January 2012 and January 2016 at the Department of Ophthalmology in Santa Maria Hospital, Lisbon, Portugal.
Eyes with dislocated IOL or having at least vision of light perception were included in this study. All patients had at least 6 months follow-up. Exclusion criteria were eyes with no light perception, corneal decompensation, advanced glaucoma, iris neovascularization, or aniridia.
Snellen visual acuity values were expressed as the logarithm of the minimum angle of resolution (logMAR) for statistical analysis. Visual acuity of light perception was set as 2.9 logMAR, hand movements as 2.6 logMAR, and counting fingers as 2.3 logMAR.
Preoperative data collected are demographics, position of dislocated IOL, previous surgeries, preoperative eye pathology, intraocular pressure, and best corrected visual acuity. Operative data and postoperative outcomes included best corrected visual acuity, lens position, intraocular pressure, pigment dispersion, endothelial cell count (cells/mm2), AC depth, and IOL position. Statistical analysis was performed by using STATA, Version 13.0.
Surgical technique
All surgeries were performed under either general or peribulbar anesthesia, and similar surgical technique was used for all the patients. All eyes included in this study had dislocated or subluxation of one-piece IOL to the vitreous cavity or retina; therefore, core and peripheral pars plana vitrectomy was performed with careful attention to release the IOL from surrounding vitreous before removal. Capsule remnants were removed. In order to protect the macula and to make the manipulation of the IOL easier and safer, perfluorocarbon liquids were used when there was a requirement. After corneal endothelium viscoelastic protection, the prolapsed IOL in the vitreous cavity or retina was carefully grasped with forceps, and the IOL positioned in the AC was extruded through corneal incision.
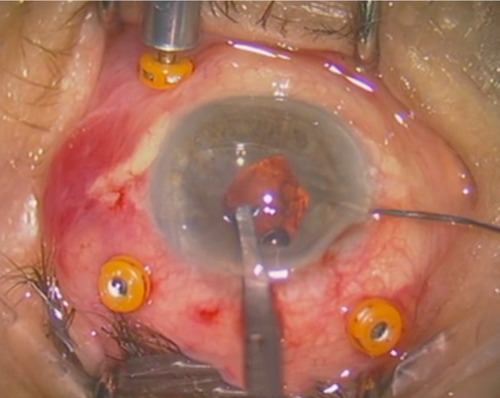
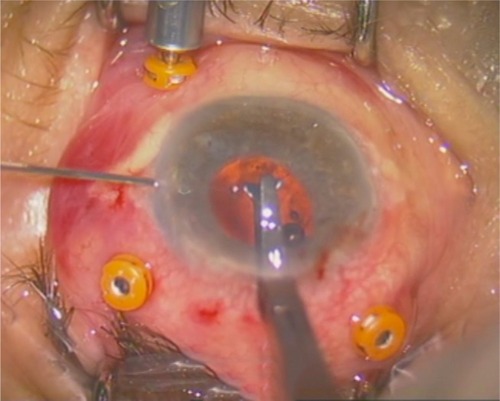
Two small corneal paracenteses were created at 3 and 9 o’clock position, and acetylcholine 1% was used, when there was a requirement, for miosis, followed by injection of viscoelastic. A 5.4 mm corneal incision was made at 12 o’clock, and then, the ICIOL was inserted at concave–convex position, rotating the IOL to a horizontal plane, and centered on the pupil. The optic of the reversed ICIOL was held with forceps. One haptic was gently slided behind the iris, and the optic was lifted slightly forward on the posterior surface of the iris so that the haptic could be found on the anterior surface of the iris. A long microspatula was used through the lateral paracentesis to insert iris tissue into the claw (). The second haptic was fixated in a similar way through the second paracentesis ().
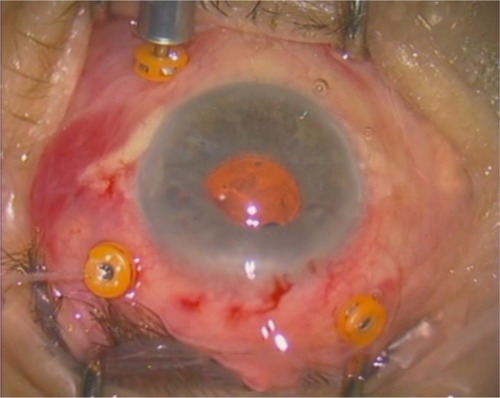
Only a small amount of iris tissue was enclavated at the claw haptics to avoid significant corectopia or pupil ovalization. Corneal incision was closed with three simple interrupted 10-0 nylon sutures ().
The lens used in this study was the Verisyse® IOL for aphakia (VRS54), which is a polymethyl methacrylate IOL with a length of 8.5 mm, maximum height of 1.04 mm, and optical zone width of 5.4 mm. The optic power was calculated using the SRK/T formula with the aim of achieving emmetropia. The manufacturer’s recommendation for constant A is 116.5 for retropupillary implantation.
Results
In this study, 29 women and 37 men were included, with a total of 26 right eyes and 40 left eyes. Nine eyes suffered posttraumatic subluxation or total dislocation of IOL, 27 eyes had postoperative complications of cataract surgery with subluxation or total dislocation of the IOL that required pars plana vitrectomy, 28 eyes had spontaneous subluxation of IOL with capsular bag, and two eyes had glaucoma, hyphema, and uveitis (uveitis-glaucoma-hyphema syndrome); malpositioned IOL was exchanged for retropupillary Verisyse® IOL.
The mean preoperative best corrected logMAR visual acuity was 1.260±0.771 (ranging from perception of light to 10/20 Snellen visual acuity). The mean age of the patients was 66.26±21.8 years (range, 22–84 years). The mean follow-up period was 23 months (range, 6–48 months). The postoperative residual spherical equivalent error was −1.75 dioptres (D) ±1.22 (D). At the end of the follow-up period, the mean postoperative best corrected logMAR visual acuity was 0.351±0.400 (ranging from perception of light to 20/20 Snellen visual acuity).
In all the cases, IOL was in a stable position, except for one case that presented with subluxation because of slippage of one of the iris claw haptics after 1 month. Recapture of the iris was easily accomplished. Pupillary dilation was not an issue in the presence of this lens style.
One case developed retinal detachment after IOL implantation for posttraumatic aphakia. There were two cases with uveitis after IOL implantation and three cases with cystoid macular edema developed 2 months after IOL implantation and vitrectomy for posterior dislocated IOL. Oval pupil was seen in 16 eyes of the patients.
The mean postoperative intraocular pressure was 15.73±3.054 mmHg, and twelve eyes with postoperative high intraocular pressure were medically managed with topical antiglaucoma drugs. Mean AC depth measured by Pentacam® was 4.125±0.8 mm. Mean postoperative endothelial cell count was 1768±741 cells/mm2.
Discussion
Surgical correction of dislocated IOL remains a challenge. The best method is one that offers best visual outcome with lowest complication in an already delicate situation. Each of the available options has its own risks and complications: transscleral fixation of posterior chamber IOLs has the advantage of posterior position of IOL, but it is a time-consuming procedure with known complications.Citation9,Citation10
Pavlidis et al has described an elegant technique of sutureless fixation of a three-piece IOL with the haptics embedded in scleral tunnels;Citation11 Jacob et al has presented a fibrin glue–assisted transscleral fixation of a three-piece IOL.Citation12 George Williams also referred to sutureless scleral fixation through trocar cannulas in the 2014 Yasuo Tano Memorial Lecture.Citation13 Haszcz et al has published a retrospective case series of 42 patients using two different techniques of scleral haptic fixation and sutureless scleral tunnels and found no difference in the outcomes of these techniques for secondary IOL implantation in posttraumatic and postoperative aphakia, which resulted in low incidence of complications.Citation14
Sutureless scleral fixation has exhibited good results especially with three-piece IOL. In this study, only one-piece IOL was considered, and this was not amenable to scleral fixation. This IOL was extruded, and another one was implanted.
Even though it is less frequent, angle-supported ACIOL implantation has frequent corneal endothelium decompensation and has been associated with several complications related to the iridocorneal angle.Citation15
Verisyse® aphakic lenses have been successfully implanted in the AC and fixated to the anterior surface of the iris in aphakic eyes that had undergone vitrectomy.Citation16,Citation17
Retropupillary implantation of a similar Verisyse® iris claw lens after vitrectomy has also been reported.Citation18–Citation21 Although implanting the iris claw lens above the iris for aphakic eyes may decrease the endothelial cell count, in most studies using the retropupillary fixation technique, a significant effect was not found on the endothelial cell count, as in the present study.Citation22,Citation23
Gicquel et alCitation20 showed a significant difference in the mean endothelial cell loss between 6 months and 1 year after penetrating keratoplasty and ICIOL implantation, comparing a group of eyes that underwent implantation of iris claw lenses in the AC (on the iris) and another group that underwent retropupillary implantation (19% vs 3.7%). Although the sample size was small (27 eyes) and the results of the study were limited, this difference appeared to favor retropupillary implantation compared with fixation on the anterior face of the iris regarding changes in the corneal endothelium.Citation24
Recently, the retropupillary approach for ICIOL implantation has become popular. In 1994, Rijneveld et al reported clinical results in 19 patients with iris claw and penetrating keratoplasty and concluded that retropupillary iris claw lens implantation in combination with penetrating keratoplasty is a safe alternative to achieve pseudophakia in eyes with corneal edema and inadequate posterior capsular support.Citation17 In 2002, Mohr et al reported retropupillary iris claw in 47 eyes and concluded that “the retropupillary fixation of an iris claw lens seems to have the advantages of a true posterior chamber implantation with a low intra- and postoperative risk profile.”Citation18 More recently, in 2015, Forlini et al published a retrospective analysis of long-term follow-up of retropupillary ICIOL implantation in 320 patients and concluded that complications related to retropupillary iris claw were minimal compared with its benefits. Therefore, using retropupillary implantation of the iris claw lens for secondary implantations is a valid alternative strategy for aphakia without capsular support.Citation15
In this study, pigment dispersion in the patients was not detected, and it was believed that the design of the Verisyse® aphakia lens and the concave–convex position provided adequate space between the iris and the ICIOL. One case of spontaneous disenclavation of one haptic occurred in the present series. It was easily grasped in the IOL body and enclavated to the iris again.
In this study, three cases of macular edema were experienced, and this was a result of the primary cause of the aphakia or the vitrectomy operation itself. Ovalization of the pupil was observed in 16 patients. Grabbing only an adequate amount of iris tissue prevented further ovalization.
In this study, elevated IOP was observed in twelve cases, and all were medically managed. Peripheral iridectomies were not performed, and no cases of pupillary block occurred. Corneal edema in three patients was easily controlled, and iris atrophy was permanent. One case of retinal detachment was reported in this series in a posttraumatic IOL dislocation patient and required further surgery.
This study has some limitations. First, its retrospective design. Also, since we wanted to report a large case-series of the same technique, we did not compare it with other options, such as AC implantation of the iris claw lens. Last, since many patients were referrals to our institution, most continued to be followed in their original ophthalmology clinic/hospital after the minimum 6-month period. Therefore, paired comparisons of the evaluated endpoints between the early and late follow-up periods could not be performed in an adequate number of patients to be considered clinically relevant.
Conclusion
The implantation of an iris claw lens behind the iris plane has the advantages of a posterior chamber lens and a short surgery time, and it is an easy surgery technique. The rate of incidences related to the implantation of retropupillar IOLs must be interpreted in the context of the surgeries usually indicated in complicated cases.
Disclosure
The authors report no conflicts of interest in this work.
References
- MinassianDCRosenPDartJKReidyADesaiPSidhuMExtracapsular cataract extraction compared with small incision surgery by phacoemulsification: a randomised trialBr J Ophthalmol200185782282911423457
- DavisDBrubakerJEspandarLStringhamJCrandallAWernerLMamalisNLate in-the-bag spontaneous intraocular lens dislocation: evaluation of 86 consecutive casesOphthalmology2009116466467019344819
- JehanFSMamalisNCrandallASSpontaneous late dislocation of intraocular lens within the capsular bag in pseudoexfoliation patientsOphthalmology2001108101727173111581041
- DickHBAugustinAJLens implant selection with absence of capsular supportCurr Opin Ophthalmol2001121475711150081
- AcarNKapranZAltanTKucuksumerYUnverYBPolatESecondary iris claw intraocular lens implantation for the correction of aphakia after pars plana vitrectomyRetina201030113113919834354
- WorstJGMassaroRGLudwigHHThe introduction of an artifitial lens into the eye using Binkhorst’s techniqueOphthalmologica197216453873914555912
- GüellJLVelascoFMalecazeFVázquezMGrisOManeroFSecondary Artisan-Verysise aphakic lens implantationJ Cataract Refract Surg200531122266227116473216
- Wolter-RoesslerMKüchleMCorrection of aphakia with retroiridally fixated IOLKlin Monatsblätter für Augenheilkd20082251210411044
- LongCWeiYYuanZZhangZLinXLiuBModified technique for transscleral fixation of posterior chamber intraocular lensesBMC Ophthalmol20151512726432550
- CelliniMStrobbeEToschiPGCamposECSecondary IOL Implantation without Capsular Support: A Laser Flare Cell Meter StudyISRN Ophthalmol2011201165324624533188
- PavlidisMde OrtuetaDSchariothGBBioptics in sutureless intrascleral multifocal posterior chamber intraocular lens fixationJ Refract Surg201127538638821243975
- JacobSAgarwalAFibrin glue assisted trans-scleral fixation of an endocapsular device for sutureless trans-scleral capsular bag fixation in traumatic subluxations: the glued endocapsular ring/segmentMed Hypothesis Discov Innov Ophthalmol2013213724600633
- AbbeyAMHussainRMShahARFaiaLJWolfeJDWilliamsGASutureless scleral fixation of intraocular lenses: outcomes of two approaches. The 2014 Yasuo Tano Memorial LectureGraefes Arch Clin Exp Ophthalmol201525311525367831
- HaszczDNowomiejskaKOleszczukAVisual outcomes of posterior chamber intraocular lens intrascleral fixation in the setting of postoperative and posttraumatic aphakiaBMC Ophthalmol20161615027145831
- SawadaTKimuraWKimuraTSugaHOhteAYamanishiSOharaTLong- term follow-up of primary anterior chamber intraocular lens implantationJ Cataract Refract Surg19982411151515209818344
- van der MeulenIJGunningFPVermeulenMGde SmetMDArtisan lens implantation to correct aphakia after vitrectomy for retained nuclear lens fragmentsJ Cataract Refract Surg200430122585258915617928
- RijneveldWJBeekhuisWHHassmanEFDellaertMMGeerardsAJIris claw lens: anterior and posterior iris surface fixation in the absence of capsular support during penetrating keratoplastyJ Refract Corneal Surg199410114197517774
- MohrA1HengererFEckardtCRetropupillary fixation of the iris claw lens in aphakia. One-year outcome of a new implantation techniquesOphthalmologe200299758058312148307
- ForliniMSolimanWBratuARossiniPCavalliniGMForliniCLong-term follow-up of retropupillary iris-claw intraocular lens implantation: a retrospective analysisBMC Ophthalmol20151514326507387
- GicquelJ-JGuigouSBejjaniRABriatBElliesPDighieroPUltrasound biomicroscopy study of the Verisyse aphakic intraocular lens combined with penetrating keratoplasty in pseudophakic bullous keratopathyJ Cataract Refract Surg200733345546417321397
- GonnermannJTorunNKlamannMKJVisual outcomes and complications following posterior iris-claw aphakic intraocular lens implantation combined with penetrating keratoplastyGraefe’s Arch Clin Exp Ophthalmol201325141151115623250481
- SchallenbergMDekowskiDHahnALaubeTSteuhlK-PMellerDAphakia correction with retropupillary fixated iris-claw lens (Artisan) – long-term resultsClin Ophthalmol2014813714124391439
- OdenthalMTPSminiaMLPrickLJJMGortzak-MoorsteinNVölker-DiebenHJLong-term follow-up of the corneal endothelium after artisan lens implantation for unilateral traumatic and unilateral congenital cataract in children: two case seriesCornea200625101173117717172893
- GonnermannJAmiriSKlamannMEndothelial cell loss after retropupillary iris-claw intraocular lens implantationKlin Monatsblätter für Augenheilkd20142318784787