Abstract
In this report, we present a case of diabetic papillopathy that resolved after a single dose of intravitreal ranibizumab injection. A 50-year-old male presented with painless visual loss in his right eye. His visual acuity was 1/10 in the right eye and 10/10 in the left eye. Anterior segment examination of both eyes was unremarkable. Posterior segment of the right eye showed nonproliferative diabetic retinopathy with a swollen optic disc. Fluorescein angiography and optical coherence tomography were performed. There was dye leakage from the right optic disc. Optical coherence tomography revealed a significant increase in retinal nerve fiber layer thickness. Magnetic resonance imaging of the brain and orbit were normal. The patient received a single intravitreal ranibizumab (0.5 mg) injection. Two weeks after the injection, there was a marked regression of the disc swelling. Three months after the injection the optic disc was pallor and visual acuity was 6/10.
Introduction
The term diabetic papillopathy (DP) is used for unilateral or bilateral optic disc swelling in which the patient has either type 1 or type 2 diabetes mellitus.Citation1 This entity is diagnosed by excluding the other causes of disc swelling.Citation2 The exact pathogenesis is not clearly understood but some authors consider DP as a form of anterior ischemic optic neuropathy (AION).Citation3 Unlike AION; DP has a benign course without significant sequela.Citation1 Although there is no accepted treatment paradigm; in some recent case reports, treatment with intravitreal injection of different agents was effective in reducing disc swelling.Citation4–Citation6 In this study we report a case of DP treated with intravitreal ranibizumab injection and demonstrate resolution of optic disc swelling.
Case report
Written informed consent has been provided by the patient to have the case details and accompanying images published.
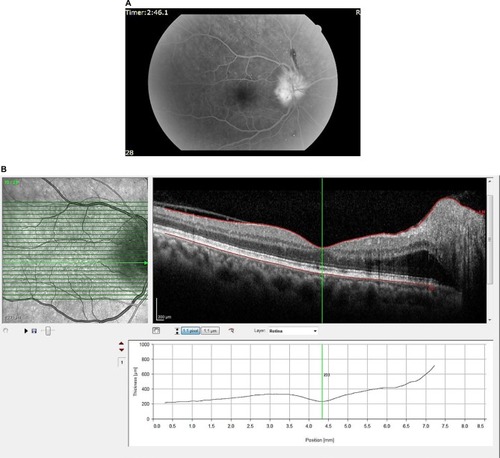
A 53-year-old male presented with acute painless decreased vision in his right eye. The patient was on a regimen of oral hypoglycemic agents and had no other known medical disease. Best-corrected visual acuity (BCVA) was 1/10 in the right eye and 10/10 in the left eye. The intraocular pressure (IOP) was 14 mm Hg in each eye. The anterior segment examination of both eyes was unremarkable. There was no afferent pupillary defect. Dilated fundus examination showed significant bilateral non-proliferative diabetic retinopathy and a swollen optic disc with telangiectatic vessels in the right eye (). Fundus fluorescein angiography (FFA) and optical coherence tomography were performed. In the right eye there was dye leakage from the optic disc and a significant increase in the retinal nerve fiberlayer thickness without macular edema (). Visual field examination of the right eye showed diffuse depression whereas the left eye was normal. Visual evoked potential was in the normal range for both eyes. Clinical neurologic examination and magnetic resonance imaging of the brain were normal. Blood pressure measurements, complete blood count, sedimentation rate and electrolytes were within normal limits. Glycosylated hemoglobin was 9.5%. After complete examination of the patient, he was diagnosed with DP and informed about expected effects and possible complications of intravitreal ranibizumab injection. After the patient was informed about the expected effects, the right eye was prepared and draped in a sterile manner and topical anesthetic was instilled in the eye. Subsequently, 0.5 mg/0.05 ml ranibizumab was injected into the vitreous cavity.
Figure 1 Fundus photographs of the patient.
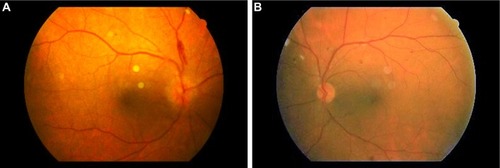
Figure 2 Fundus fluorescein angiography and optical coherence tomography image of the right eye.
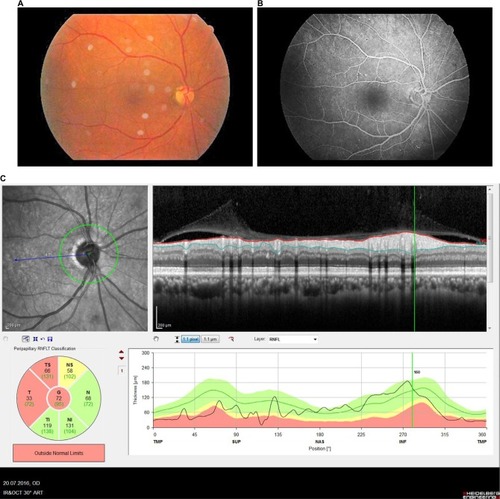
Within 2 weeks, BCVA in the right eye improved to 3/10 and IOP was normal. There was marked regression of disc swelling (). Three months following the injection, BCVA was 6/10, IOP was normal, and the optic disc was mildly pale with complete resolution of swelling in the right eye (). The patient is being followed up for his diabetic retinopathy.
Figure 3 Retinal images 2 weeks after the injection.
Abbreviations: RNFL, retinal nerve fiber layer; RNFLT, retinal nerve fiber layer thickness; T, temporal; TS, superior temporal; NS, superior nasal; N, nasal; NI, inferior nasal; TI, inferior temporal; G, global; TMP, temporal; SUP, superior; NAS, nasal; INF, inferior.
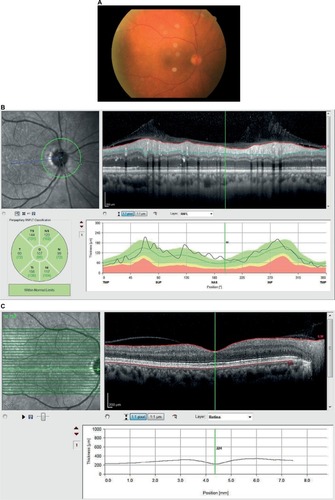
Figure 4 Retinal images 3 months after the injection.
Discussion
Acute, painless visual loss is a clinical sign of optic disc swelling that is caused by a variety of reasons. DP is one of these reasons and it has been published by many investigators since 1971.Citation7,Citation8 Although it is thought to be a mild form of non-arteritic AION by some researchers,Citation3 DP can be distinguished from AION by certain clinical findings. In contrast to patients with DP, AION patients suffer from profound loss of visual acuity. After the resolution of optic neuropathy visual field defect and visual acuity loss persists in patients with AION. On the other hand; in DP patients visual field defects are transient and visual acuity improves to 4/10 or more.Citation1,Citation2 These two conditions can also be distinguished by FFA. Early disc hypofluorescence due to hypoperfusion with late leakage around the affected segment occurs in AION. But in patients with DP, FFA shows a very early hyperfluorescence, most likely due to telangiectasia of the optic disc that increases throughout the study.Citation9
The patient was diagnosed as having DP because of the following: painless visual loss, no other clinical disorder except uncontrolled diabetes mellitus, early disc hyperfluo-rescence on FFA and good visual outcome post-treatment.
Anti-VEGF agents have recently been used for some reported DP cases with visual improvement and reduced optic disc swelling.Citation4,Citation5 Periocular and intravitreal corticosteroid injection was also found to be effective in patients with DP.Citation6 These effective treatment options indicate that inflammatory elements could be involved in the pathogenesis of this disorder. It is known that VEGF induces a rapid and reversible increase in vascular permeability. So, if an optic nerve head is ischemic there will be an increased amount of VEGF leading to vasogenic disc edema.Citation10 But still the exact pathogenesis of DP and the mechanism of action of anti-VEGF in patients with DP is not well understood. The treatment we administered in our case was intravitreal ranibizumab injection. After 2 weeks, disc swelling had largely resolved and visual acuity had improved from 1/10 to 6/10. There were no complications at all and DP had not reappeared at the 3-month follow-up.
Conclusion
Two weeks after intravitreal ranibizumab injection, there was an increase in visual acuity in our patient. VEGF may play a role in the pathogenesis of DP and so the administered intravitreal ranibizumab could have helped the patient to recover. However, the efficacy and safety of this management of DP needs to be proven through further larger clinical studies.
Disclosure
The authors report no conflicts of interest in this work.
References
- BayraktarZAlacaliNBayraktarSDiabetic papillopathy in type II diabetic patientsRetina200222675275812476102
- RegilloCDBrownGCSavinoPJByrnesGABensonWETasmanWSSergottRCDiabetic papillopathy. Patient characteristics and fundus findingsArch Ophthalmol199511378898957605280
- HayrehSSZimmermanBNonarteritic anterior ischemic optic neuropathy: clinical characteristics in diabetic patients versus nondiabetic patientsOphthalmology2008115101818182518502511
- KimMLeeJHLeeSJDiabetic papillopathy with macular edema treated with intravitreal ranibizumabClin Ophthalmol201372257226024348012
- Al-HinaiASAl-AbriMSAl-HajriRHDiabetic papillopathy with macular edema treated with intravitreal bevacizumabOman J Ophthalmol20114313513822279402
- Al-HaddadCEJurdiFABashshurZFIntravitreal triamcinolone acetonide for the management of diabetic papillopathyAm J Ophthalmol200413761151115315183815
- LubowMMakleyTAJrPseudopapilledema of juvenile diabetes mellitusArch Ophthalmol19718544174225554869
- AppenREChandraSRKleinRMyersFLDiabetic papillopathyAm J Ophthalmol19809022032097425031
- OtoSYilmazGCakmakciAAydinPIndocyanine green and fluorescein angiography in nonarteritic anterior ischemic optic neuropathyRetina200222218719111927852
- WeisSMChereshDAPathophysiological consequences of VEGF-induced vascular permeabilityNature2005437705849750416177780
