Abstract
We report an unusual presentation of an orbital cavernous hemangioma in a 26-year-old female, who noted sudden redness and swelling of the left eye (LE) on waking up. At presentation, upper eyelid edema with periorbital ecchymosis and subconjunctival hemorrhage were noted in the LE. Although there was transient symptomatic relief with topical medications, blurring of vision developed in the LE. When seen 10 days later, the patient’s LE showed axial proptosis. Magnetic resonance imaging revealed an intraconal soft tissue mass in the superomedial quadrant of the left orbit. Superior orbitotomy with mass excision was done; histopathological examination of the excised mass revealed a cavernous hemangioma. The patient had complete visual recovery following surgery. To our knowledge, an acute presentation of an orbital cavernous hemangioma with subconjunctival hemorrhage and periorbital ecchymosis has not previously been reported.
Introduction
Cavernous hemangiomas are the most common vascular lesions of the orbit in adults, being commonly seen in middle age, with a female predilection.Citation1 Over 80% of orbital cavernous hemangiomas are located within the intraconal compartment, most commonly in the lateral aspect.Citation2 Progressive painless proptosis is the usual mode of presentation, and acute presentations are rare.Citation3 We report an unusual acute presentation of an orbital cavernous hemangioma with subconjunctival hemorrhage (SCH) and periorbital ecchymosis.
Case report
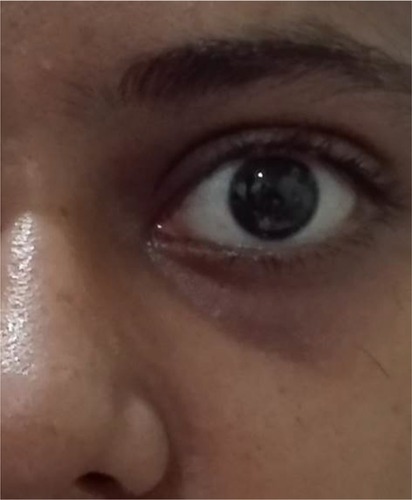
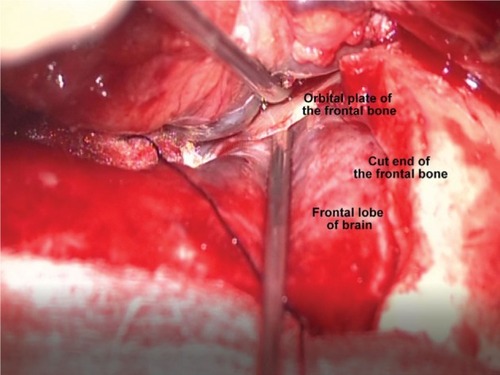
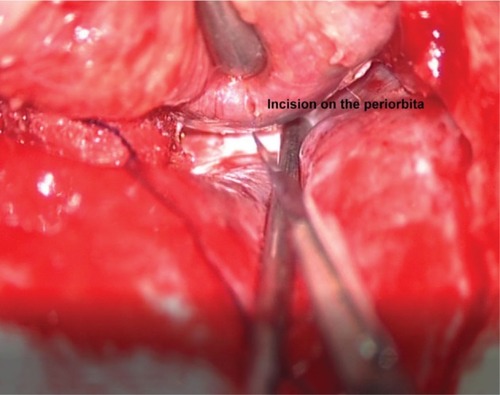
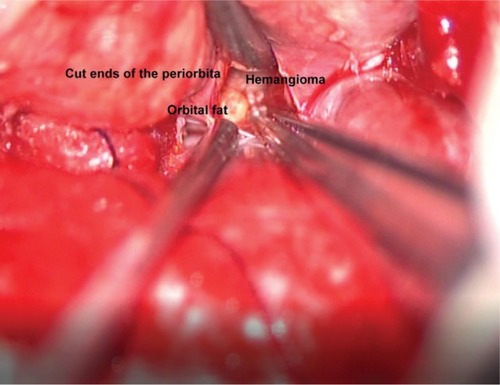
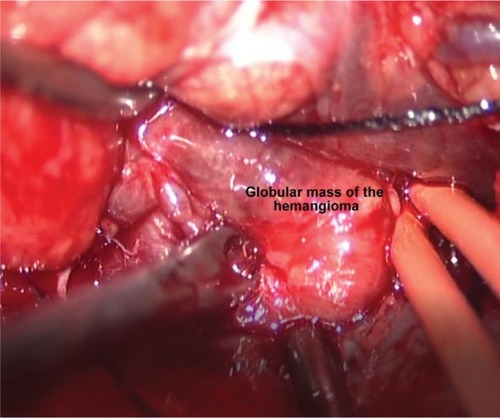
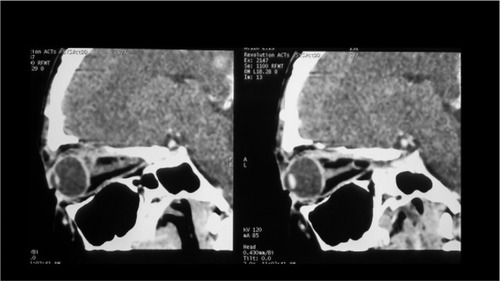
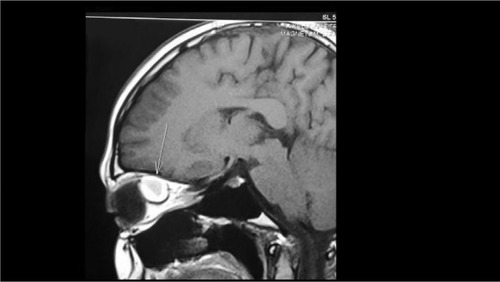
Written informed consent has been provided by the patient to have the case details and any accompanying images published. A 26-year-old female presented with swelling and redness of the left eye (LE) that she noticed on waking up. She had not sustained antecedent trauma or undergone Valsalva maneuver and did not provide any other significant medical history such as bleeding diatheses or drug intake. On examination, the best corrected visual acuity in both eyes was 20/20, N5. The right eye examination was unremarkable. In the LE, there was SCH involving the bulbar temporal conjunctiva, along with upper eyelid edema and periorbital ecchymosis (). The rest of the anterior segment, and the entire posterior segment, were normal. General and systemic examination findings were normal. Hematological investigations did not suggest any bleeding disorder. She was given symptomatic treatment and advised to review after a week. When she returned 10 days later, the swelling and redness were seen to have subsided, but she had developed blurred vision in the LE. The vision in the LE was 20/40, pupils were brisk and reacting normally to light and extraocular movements were full. However, the left eyeball was proptosed with inferior scleral show (). Hertels exophthalmometry showed a 3 mm axial proptosis of the LE, with fundus examination revealing choroidal folds at the posterior pole. Color vision and visual fields were normal. Magnetic resonance imaging revealed a well-defined intraconal mass lesion of size 20×16×15 mm in the superomedial aspect of left orbit that was T1/T2 hyperintense with a mass effect on optic nerve, medial rectus and posterior surface of globe. The presence of T1 hyperintensity (plain and fat suppression) indicated the presence of blood degradation products suggestive of intralesional thrombosis (–). Since the lesion was located behind the globe (retro-ocular), and in order to minimize handling of tissues in the anterior part of the orbit, a transcranial approach was preferred. An intrahairline left frontal scalp incision was made. The frontal bone was cut using craniotome. Working from the orbital side with osteotomes, the roof of the orbit was cut behind the supraorbital margin to raise the orbitofrontal bone flap as a single piece. The posterior portion (medial part) of the roof of the orbit was removed (). The periorbita was incised (). Dissecting through the fat of the orbit, the medial part of the muscle cone was entered between the medial border of the superior rectus and the medial rectus muscles. The hemangioma was seen as a dark globular mass (). It had a good plane of cleavage and initial dissection was done on the lateral surface, then the medial surface and then the anterior surface. The tumor was dissected away from the medial rectus muscle on the medial aspect. The posterior most portion of the tumor was the last to be exposed. There was a single vascular pedicle on the superolateral aspect, which was coagulated and divided to excise the entire mass of the hemangioma (). Intraorbital and extradural hemostasis was ensured. The orbitofrontal bone flap was replaced. The patient had no neurological deficits after surgery. The postoperative computerized tomogram confirmed that the mass had been completely excised (). Histopathological examination of the excised mass revealed a cavernous hemangioma with an organized hematoma. When seen 1 month after surgery, she was found to have had a complete (20/20) visual recovery ().
Figure 3 Magnetic resonance imaging (axial section) showing intraconal mass lesion in the left orbit (arrow).
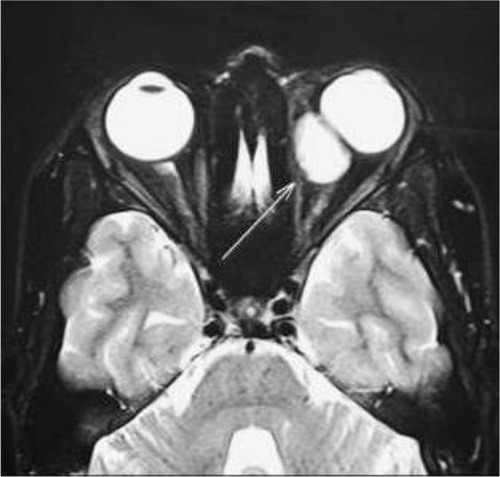
Figure 4 Magnetic resonance imaging of axial (A) and coronal (B) section.
Abbreviation: RHP, right headend posterior.
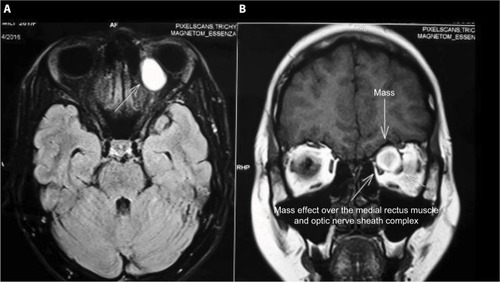
Figure 5 Magnetic resonance imaging showing sagittal section.
Discussion
Vascular events in the orbit can present acutely. The symptoms or signs can occur due to orbital hemorrhage, acute arteriovenous shunting or subacute thrombosis (typically within orbital veins). Such acute symptoms can either lead to a new diagnosis of underlying vascular disease in some, or there can be an acute deterioration of a vascular disease that was already known, in others.Citation4
The most common cause of a spontaneous orbital hemorrhage is an underlying orbital vascular anomaly.Citation5 An acute orbital hemorrhage can occur from normal vessels following trauma, Valsalva maneuvers, in hypertensives and in those on antiplatelets or those with bleeding disorders. It can also occur in the presence of congenital or acquired vascular malformations, such as venous–lymphatic malformations (common) and in arteriovenous malformations (rare), as well as from neoplastic vessels (tumors).Citation4
Sudden onset of symptoms in an acute vascular event is proposed to be due to hemorrhage from fragile abnormal vessels, acute arteriovenous shunting and subacute thrombosis due to changes in perfusion. The presenting symptoms and signs include proptosis, periocular bruising, episcleral venous congestion, increased intraocular pressure, chemosis and a frank bleeding from the orbit.Citation4
A cavernous hemangioma of the orbit, which typically presents as a slow-growing tumor with gradual onset of symptoms, usually causes a mass effect, due to an increase in volume of the orbital contents. The patient may present with a painless, slowly progressive bulging of the globe. A reduction in visual acuity and presence of visual field defects are manifestations of a mass effect or pressure on the optic nerve and surrounding vasculature. Diplopia may occur due to extraocular muscle dysfunction. Lagophthalmos due to extraocular muscle dysfunction or nerve involvement results in exposure keratopathy, keratitis, and corneal perforation. Pupillary dysfunction is sometimes noted due to involvement of neural structures within the orbit.Citation6
Spontaneous bleeding in an orbital cavernous hemangioma, with resultant acute onset of symptoms, although extremely rare, has been reported.Citation7 Yamamoto et alCitation7 report a spontaneous hemorrhage from orbital cavernous hemangioma resulting in sudden onset of ophthalmopathy in an elderly lady. Arora et alCitation3 describe an acute presentation of an orbital cavernous hemangioma with a visual field defect. Three cases of spontaneous intraorbital hemorrhage caused by cavernous angioma of the orbit have been reported by Zenobii et al.Citation8
The mechanism of bleed remains unclear. Some postulates include local hemodynamic changes, hypoxiaCitation9 and bleeding from capillaries in the sinusoidal space.Citation10 SCH and periorbital ecchymosis noted in our patient may have happened due to the blood tracking within the fascial planes of orbit, following a spontaneous orbital bleed.Citation8
A search of the PubMed database, using the keywords “cavernous hemangioma, subconjunctival haemorrhage”, “cavernous hemangioma, periorbital ecchymosis” did not generate any relevant published papers. To our knowledge, this is the first case report of an intraconal cavernous hemangioma of the orbit, presenting acutely, with SCH and periorbital ecchymosis.
Disclosure
The authors report no conflicts of interest in this work.
References
- AnsariSAMafeeMFOrbital cavernous hemangioma: role of imagingNeuroimaging Clin N Am200515113715815927865
- AnandRDeriaKSharmaPNarulaMGargRExtraconal cavernous hemangioma of orbit: a case reportIndian J Radiol Imaging200818431031219774188
- AroraVPratMCKazimMAcute presentation of cavernous hemangioma of the orbitOrbit201130419519721780934
- RoseGEVerityDHAcute presentation of vascular disease within the orbit-a descriptive synopsis of mechanismsEye (Lond)201327329930723370421
- Wills Eye Resident Case Series – Diagnosis and Discussion Available from: https://www.reviewofophthalmology.com/.../wills-eye-resident-case-series-diagnosis-accessedAccessed January 10, 2017
- CohenAJMercandettiMWeinbergDA webpage on the InternetHemangioma, Cavernous (Aug 2008) Available from: http://emedicine.medscape.com/article/12,18,120-overviewAccessed May 25, 2016
- YamamotoJTakahashiMNakanoYSpontaneous hemorrhage from orbital cavernous hemangioma resulting in sudden onset of ophthalmopathy in an adult – case reportNeurol Med Chir (Tokyo)2012521074174423095267
- ZenobiiMGalzioRJLucantoniDCaffagniEMaglianiVSpontaneous intraorbital hemorrhage caused by cavernous angioma of the orbitJ Neurosurg Sci198428137406470801
- McNabAAWrightJECavernous haemangiomas of the orbitAust N Z J Ophthalmol19891743373452624723
- HarrisGJJakobiecFACavernous hemangioma of the orbitJ Neurosurg1979512219228448430