Abstract
Two illustrative cases of chronic branch retinal vein occlusion are presented with multimodal imaging, including commercially available optical coherence tomography angiography. In these two patients, retinal ischemia and collateral vessels were well imaged without the need to use traditional fluorescein angiography. Optical coherence tomography angiography provides useful information for the diagnosis and management of patients with branch retinal vein occlusion and other retinal vascular diseases.
Introduction
Branch retinal vein occlusion (BRVO) is a common retinal vascular disease that may lead to cystoid macular edema (CME), retinal ischemia, retinal neovascularization, and other complications.Citation1 Spectral domain optical coherence tomography (SD-OCT) is important in the management of this entity. More recently, OCT angiography (OCT-A) has become available and has provided new insights for clinicians managing this disease.Citation2
Using multimodal imaging, including OCT-A imaging with the commercially available Cirrus 5000 with AngioPlex (Zeiss, Jena, Germany), the pathologic features of chronic BRVO in two patients are demonstrated.
Report of two cases
Case 1
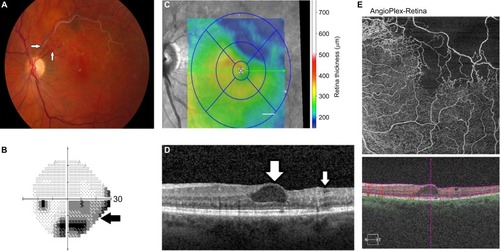
A 56 year-old female with a history of chronic BRVO left eye returned for scheduled follow-up, noting long-standing but stable blurred vision. She had been treated with intravitreal Avastin® (bevacizumab) (Avastin®; Genentech, South San Francisco, CA, USA) and triamcinolone acetonide in the past, but no treatments for several years. On examination, best-corrected visual acuity was 20/40 in the left eye. Fundus examination revealed sclerotic vessels in the superotemporal quadrant with collaterals near the optic disc, as well as CME (). Humphrey visual field 24-2 testing revealed an inferior arcuate defect encroaching fixation (). SD-OCT revealed mild thickening centrally and atrophy superotemporally (). SD-OCT through the center of the macula revealed a prominent central cyst as well as temporal thinning (). The OCT-A retina slab (6×6 mm) demonstrated marked capillary nonperfusion in the superotemporal macula, involving the foveal avascular zone (FAZ) ().
Figure 1 BRVO, left eye.
Abbreviations: BRVO, branch retinal vein occlusion; OCT-A, optical coherence tomography-angiography; SD-OCT, spectral domain optical coherence tomography.
Case 2
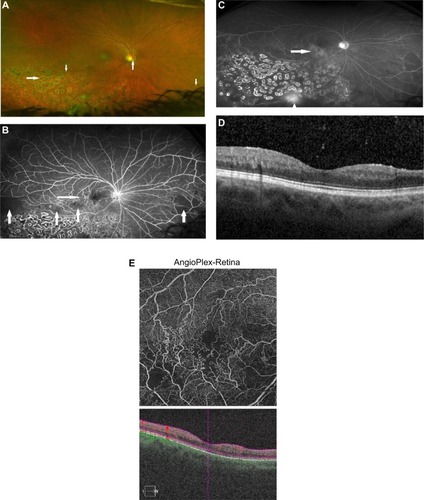
A 52-year-old female with a history of chronic hemiretinal vein occlusion right eye presented with recurrent episodes of floaters and visual loss. She had been treated with scatter photocoagulation elsewhere about six months previously. On examination, best-corrected visual acuity was 20/25. Fundus examination revealed sclerotic veins inferotemporally and inferonasally. Scatter photocoagulation was evident inferotemporally. Collateral vessels temporal to the center of the macula and crossing the horizontal raphe were present (). Fluorescein angiography revealed areas of ischemia temporally and inferonasally, with collateral vessels temporal to the center of the macula (). Late frames revealed mild macular leakage and more prominent leakage inferiorly, consistent with retinal neovascularization (). SD-OCT through the center of the macula showed no frank CME (). The OCT angiography retina slab (6×6 mm) demonstrated prominent collateral vessels temporal (and some nasal) to the foveal avascular zone, as well as capillary nonperfusion involving the inferior FAZ as well as inferotemporal to the center of the macula ().
Figure 2 Hemiretinal vein occlusion, right eye.
Abbreviations: OCT-A, optical coherence tomography-angiography; SD-OCT, spectral domain optical coherence tomography.
Discussion
These two cases illustrate the utility of OCT-A in providing additional information in the management of patients with chronic BRVO. In case 1, OCT-A demonstrates capillary non-perfusion involving the FAZ, which correlates with the visual field defect encroaching fixation. This suggests that visual loss is due to both CME and macular ischemia and that further pharmacologic treatment of the CME might not benefit the patient. In case 2, OCT-A demonstrates capillary nonperfusion and highlights the collateral vessels, which were poorly visualized on fundus photography but were visualized using fluorescein angiography. Case 2 also provides a comparison between OCT-A and fluorescein angiography, demonstrating concordance between the collateral vessels and the macular ischemia on each test.
The role of OCT-A in the management of BRVO is evolving. OCT-A may offer similar information to fluorescein angiographyCitation3 and can be obtained rapidly and without the need for dye injection. OCT-A is reported to image the FAZ well in patients with BRVO.Citation4 However, the technology is currently expensive, and image quality depends on the patient’s ability to fixate.Citation5
As additional patients with acute and chronic BRVO, and other retinal vascular diseases, are imaged with OCT-A, the utility of this noninvasive imaging technology will become better understood and may help in screening or predicting visual outcomes.
Acknowledgments
Partially supported by NIH Center Core Grant P30EY014801 and an unrestricted grant from Research to Prevent Blindness. This manuscript has not been presented at any meeting. Written informed consent has been provided by the patients to have the case details and any accompanying images published.
Disclosure
The authors report no conflicts of interest in this work. SGS has received consulting fees from Alimera Sciences unrelated to this work.
References
- GregoriNZRattanGHRosenfeldPJSafety and efficacy of intravitreal bevacizumab (Avastin) for the management of branch and hemiretinal vein occlusionRetina200929791392519584649
- ShahlaeeAHongBKHoACOptical coherence tomography angiography features of branch retinal vein occlusionRetin Cases Brief Rep2017111909326938835
- SuzukiNHiranoYYoshidaMMicrovascular abnormalities on optical coherence tomography angiography in macular edema associated with branch retinal vein occlusionAm J Ophthalmol201616112613226454243
- WonsJPfauMWirthMAOptical coherence tomography angiography of the foveal avascular zone in retinal vein occlusionOphthalmologica2016235419520227160007
- Nobre CardosoJKeanePASimDASystematic evaluation of optical coherence tomography angiography in retinal vein occlusionAm J Ophthalmol20161639310726621685
