Abstract
Oculogyric crisis (OGC), frequently caused by medications such as antiemetics, antidepressants, and anti-epileptics, is an acute dystonic reaction of the ocular muscles. It consists of wide-staring gaze (lasting variably from seconds to minutes), seizures, and a widely-opened mouth. To date, there have been no reports of anti-tuberculosis medications such as rifampicin, isoniazid, pyrazinamide or ethambutol inducing OGC. It is of utmost importance to recognize this adverse reaction, which could be incorrectly diagnosed as an anaphylactic-like reaction. In this paper, we highlight a case of a 66-year-old Indian man who presented with OGC induced by anti-tuberculosis medications which was initially suspected to be an anaphylactic reaction and was subsequently halted with the administration of diphenhydramine.
Introduction
Dystonia consists of intermittent contractions of muscles resulting in irregular and repetitive movements. It is frequently triggered or aggravated by any voluntary action.Citation1 Oculogyric crisis (OGC), is a form of ocular dystonia frequently caused by medications such as antipsychotics which usually lasts from seconds to minutes.Citation2 It usually presents with contraction of extraocular muscles resulting in a deviation of the eyes.Citation3 The adverse side effects of anti-tuberculosis (anti-TB) medications are well-documented, including arthralgia, neurological disorders, hepatotoxicity, allergic reactions, and gastrointestinal disorders.Citation4,Citation5 To date, there have been no reports of rifampicin, isoniazid, ethambutol, and pyrazinamide (RHEZ) causing OGC. We report a case of a 66-year-old Indian man, admitted to the Department of General Medicine, Tan Tock Seng Hospital, Singapore, who developed acute OGC 30 minutes after ingesting RHEZ.
Case report
Written consent was obtained from the patient for the publication of his case and images. A 66-year-old Indian male patient presented to the Tuberculosis Control Unit after sudden onset of near syncope, nausea, diaphoresis, light-headedness, and a wide-staring gaze with upward and lateral deviation of eyes 30 minutes after consuming newly-prescribed RHEZ. These symptoms resolved on the administration of diphenhydramine 25 mg intravenously at the Emergency Department. The patient was referred, initially, to the Department of Rheumatology, Allergy and Immunology based on the suspicion of a reaction to RHEZ. A diagnosis of anaphylaxis-like and possibly idiosyncratic reaction to rifampicin was made.
On further questioning by the primary team, the patient reported that while he was aware of his surroundings and was able to hear conversations around him, he felt “physical blocked” in that he was unable to respond with purposeful voluntary movements or speech; he additionally described abdominal discomfort and generalized weakness.
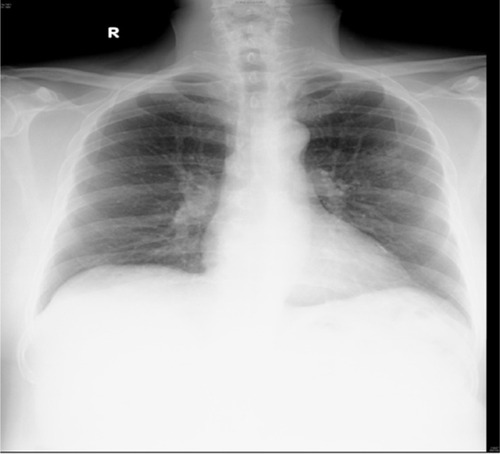
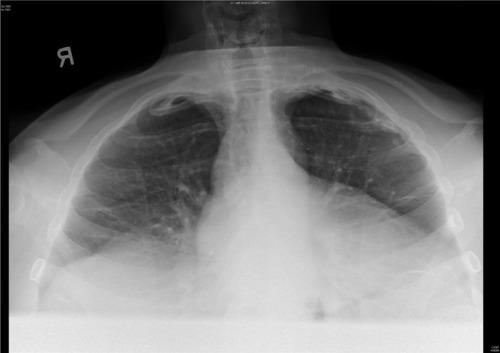
The patient had just been prescribed daily rifampicin 600 mg, isoniazid 300 mg, ethambutol 1.6 g, pyrazinamide 1.75 g (i.e., standard RHEZ combination therapy for TB of uncertain origin and resistance, according to his weight of 98.3 kg) and pyridoxine 10 mg after increased nodular opacities in the left upper zone were observed on sequential chest X-rays ( and ), suggestive of granulomata. A small calcified pleural plaque was also noted. Blood cultures, sputum cultures, and Mycobacterium tuberculosis polymerase chain reaction were negative.
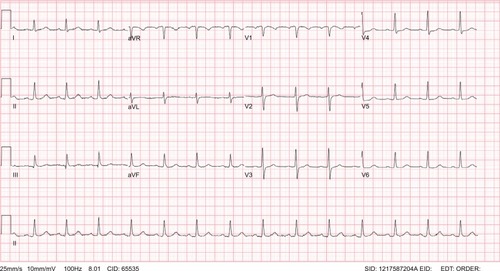
On his initial presentation after the near syncope, the patient’s vitals were stable and physical examination, including neurological examination, did not reveal any conclusive findings. A full blood count, liver function test, thyroid function test, drug screen, troponin I, electrocardiogram (), and a two-dimensional echocardiography were performed.
However, the diagnosis was subsequently changed to OGC based on the more complete history recorded. Another possible cause of OGC would include trauma. However, the patient did not suffer from any trauma recently.
Discussion
Acute dystonia is intermittent or sustained involuntary muscle contractions involving the face, neck, and other parts of the body.Citation6 OGC is a subset of acute dystonia which frequently affects the extraocular muscles resulting in spasmodic-like action. The most common cause includes medications such as metoclopramide, olanzapine, haloperidol, and carbam-azepine.Citation7,Citation8 Certain recreational drugs such as cocaine have also been reported to cause OGC.Citation9 Interestingly, until now there have been no reports of anti-TB medications causing OGC. In addition, OGC can occur in Wilson’s disease, cystic glioma, and post-encephalitic parkinsonism.Citation10–Citation13
The pathophysiology of OGC is still uncertain, but it is believed to be caused by blockage of dopaminergic pathways centrally, which results in an upregulation of striatal acetylcholine.Citation14 This in turn causes involuntary, irregular muscular contractions. A study done by Mendhekar et al. showed that, at low doses, amisulpride (100–300 mg/day) preferentially binds to D2/D3 presynaptic receptors which subsequently increases dopaminergic transmission in the prefrontal cortex. However, OGC occurred at a dose of 400-800 mg/day where there is antagonism of the postsynaptic dopaminergic receptors.Citation15 Shumy et al. reported a case of pyrazinamide-induced parkinsonism which could be linked to the dopaminergic antagonist effects of it.Citation16 Similarly, the dopaminergic antagonist effects of pyrazinamide could have resulted in the OGC.
Reversal of OGC may be effected with the use of anti- cholinergic medications like promethazine or diphenhydramine. Diphenhydramine served both as a diagnostic test and therapeutic intervention in this 66-year-old gentleman.
In this case, the diagnosis was based on history and the resolution of symptoms with diphenhydramine.
Conclusion
OGC is often a diagnosis that is overlooked because of an incomplete history, poor appreciation of the presentation of OGC, and a low index of suspicion in cases where the medication implicated is not often associated with such a reaction. In such cases, rather than assigning a label such as an “allergic” reaction, the history should be confirmed and if possible, a monitored drug challenge undertaken to ascertain the reaction provoked. Physicians should also be alert toward medications which are not known to cause OGC, but may also cause it.
Disclosure
The authors report no conflicts of interest in this work.
References
- AlbaneseABhatiaKBressmanSBPhenomenology and classification of dystonia: a consensus updateMov Disord201328786387323649720
- GardnerDMAbidiSUrsuliakZMorrisonJTeehanMDTibboPGIncidence of oculogyric crisis and long-term outcomes with second-generation antipsychotics in a first-episode psychosis programJ Clin Psychopharmacol201535671571826485339
- RobottomBJFactorSAWeinerWJMovement disorders emergencies part 2: hyperkinetic disordersArch Neurol201168671972421670395
- SinglaRSharmaSKMohanAEvaluation of risk factors for antituberculosis treatment induced hepatotoxicityIndian J Med Res20101327818620693595
- VolminkJGarnerPDirectly observed therapy for treating tuberculosisCochrane Database Syst Rev20074CD00334317943789
- MunhozRPMoscovichMAraujoPDTeiveHAMovement disorders emergencies: a reviewArq Neuropsiquiatr201270645346122699544
- BatemanDNRawlinsMDSimpsonJMExtrapyramidal reactions with metoclopramideBr Med J (Clin Res Ed)19852916500930932
- BhachechJTAripiprazole-induced oculogyric crisis (acute dystonia)J Pharmacol Pharmacother20123327928123129969
- van HartenPNHoekHWKahnRSFortnightly review: acute dystonia induced by drug treatmentBMJ1999319721062362610473482
- OnuaguluchiGCrises in post-encephalitic parkinsonismBrain19618439541414482072
- MatsumuraKSakutaMOculogyric crisis in acute herpetic brainstem encephalitisJ Neurol Neurosurg Psychiatry19875033653663559623
- LeeMSKimYDLyooCHOculogyric crisis as an initial manifestation of Wilson’s diseaseNeurology19995281714171510331711
- StechisonMTCystic glioma with positional oculogyric crisisJ Neurosurg1989716955957
- BlanchetPJAntipsychotic drug-induced movement disordersCan J Neurol Sci200330Suppl 1S101S10712691483
- MendhekarDNLohiaDKateriaPTardive oculogyric crisis associated with amisulpride monotherapyJ Postgrad Med201056430530620935407
- ShumyFAnamAChowdhuryMShazzadMPyrazinamide Induced ParkinsonismJournal Of Medicine20171814446