Abstract
Hepatitis E is caused by infection with the hepatitis E virus (HEV). HEV is transmitted orally via HEV-contaminated food or drink. Hepatitis E usually shows mild symptoms and is self-limiting in the general population; however, it may progress to chronic hepatitis in immunosuppressed patients such as recipients of organ transplantation. However, a few cases of acute hepatitis E have been reported in organ transplantation recipients. We herein report a case of acute hepatitis E in a 31-year-old male renal transplant recipient. The patient underwent renal transplantation 2 years ago, and his postoperative course was uneventful without rejection. After complaining of general fatigue and low-grade fever for 1 week, he was referred to and admitted to our hospital. Careful interview revealed that he ate undercooked pork 10 weeks prior. Blood analysis revealed liver dysfunction but was serologically negative for hepatitis A, B and C virus, cytomegalovirus infection and collagen diseases. Immunoglobulin A antibody against hepatitis E virus (HEV-IgA) was also negative at that point. After 2 weeks of admission, HEV-IgA and HEV-RNA were measured again as hepatitis E could not be ruled out due to history of ingestion of undercooked meat that may have been contaminated with HEV. At that time, HEV-IgA and HEV-RNA (genotype 3) were positive. Thus, an acute hepatitis E was diagnosed. His liver function gradually improved to within the normal range, and HEV-IgA and HEV-RNA were negative at 11 weeks after admission. In conclusion, we describe here a case of acute hepatitis E in a renal transplant recipient. Careful interview regarding the possibility of ingestion of HEV-contaminated food and repeated measurements of HEV-IgA were helpful in finalizing a diagnosis.
Introduction
Hepatitis E is caused by infection with the hepatitis E virus (HEV), which is a single-stranded, non-enveloped, RNA icosahedral virus.Citation1 HEV is most commonly transmitted orally through ingesting food or drink that is contaminated with HEV.Citation2,Citation3 Hepatitis E has been reported to usually cause mild symptoms such as low-grade fever, appetite loss and mild jaundice and is self-limiting in the general population.Citation1 However, it may develop into chronic hepatitis in immunosuppressed patients such as recipients of organ transplantation.Citation4 In the study by Kamar et al,Citation5 66% of hepatitis E patients who were also organ transplantation recipients progressed to chronic hepatitis and 10% these chronic hepatitis E patients progressed to liver cirrhosis.
However, a few cases of acute hepatitis E have been reported in organ transplantation recipients. We herein report a case of acute hepatitis E in a renal transplant recipient.
Case report
The patient was a 31-year-old man who underwent renal transplantation 2 years ago. The donor was his mother. Their ABO blood type was compatible, and antibodies against donor-specific human leukocyte antigen were negative in the recipient as determined by complement-dependent cytotoxicity, flow cytometry-based crossmatch and panel reactive antibody. His postoperative course was uneventful without rejection, and his immunosuppressive regimen consisted of 3.5 mg/day tacrolimus, 1000 mg/day mycophenolate mofetil and 0.5 mg/ day everolimus. The patient’s liver function was normal. He was referred to our hospital after complaining of general fatigue and low-grade fever starting 1 week before presentation. Careful interview revealed that he ate undercooked pork 10 weeks prior. A low-grade fever was observed, but jaundice and abdominal pain were not. Blood examination revealed liver dysfunction. He was admitted to our hospital for further examination and treatment for liver dysfunction. Written informed consent to publication was obtained from the patient.
The laboratory data upon admission are shown in . Blood examination showed liver dysfunction but was negative for antigens and antibodies for hepatitis A, B and C virus, cytomegalovirus (CMV) infection and collagen diseases (). Immunoglobulin A antibody against hepatitis E virus (HEV-IgA) was also negative at that point (). Notably, markers of liver damage were upregulated over time (). Because we knew he ate undercooked pork 10 weeks prior, we thought that the possibility of hepatitis E could not be ruled out as the cause of his liver disease. Therefore, we measured HEV-IgA again and also measured HEV-IgM and HEV-RNA 2 weeks after admission. At that time, both HEV-IgA and HEV-IgM were positive as well as genotype 3 HEV-RNA (4.3 log copy/ mL, cutoff value: <2.0 log copy/mL; ). Therefore, acute hepatitis E was diagnosed. The administration of ursodeoxycholic acid, monoammonium glycyrrhizinate, glycine, aminoacetic acid and l-cysteine hydrochloride hydrate was started for liver protection. No specific antiviral agent against HEV was used. His liver function gradually improved to within the normal range, and HEV-IgA and HEV-RNA were once again negative at 11 weeks after admission (). During this episode, the administration of immunosuppressive agents was continued without deterioration in renal function of the transplanted kidney.
Figure 1 Patient’s clinical course.
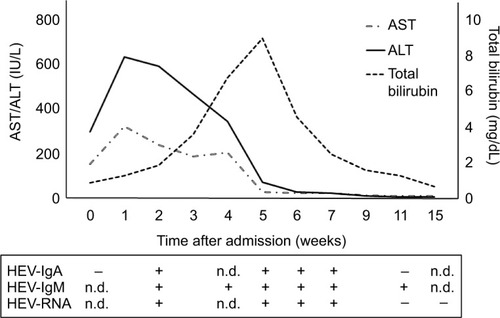
Table 1 Laboratory findings at initial presentation
Discussion
We have described a case of acute hepatitis E in a renal transplant recipient. Four genotypes of HEV have been reported.Citation6 Genotypes 1 and 2 of HEV can only be transmitted to humans via waterborne and fecal–oral transmission.Citation6 Genotypes 3 and 4 of HEV are transmitted via zoonotic infections from pigs, wild boar, deer and other animals and humans.Citation6 Humans are therefore commonly infected with HEV by ingesting meat or water contaminated with HEV.Citation7 In addition, blood transfusion and allograft transplantation reportedly increase the risk of transmission of HEV because screening for HEV is not well established in blood and organ donation.Citation8,Citation9 In the present case, the patient had a recent history of ingestion of undercooked meat but not of blood transfusion. Additionally, his postoperative course was uneventful without liver dysfunction during the 2 years after renal transplantation. Therefore, HEV in this patient may be caused by ingestion of HEV-contaminated meat.
Previously, hepatitis E has been diagnosed based on the presence of HEV-IgM and HEV-RNA.Citation10 However, recently HEV-IgA has been used as a first screening examination to detect the acute phase of HEV infection because HEV-IgA is superior to HEV-IgM in terms of sensitivity and specificity.Citation11 HEV-IgA has been reported to be positive when symptoms appear, and liver enzymes increase in the general population.Citation11 However, in this patient, HEV-IgA was negative when symptoms first appeared and liver enzymes increased. Notably, HEV-IgA showed a delayed positive response at 5 weeks later. Immunosuppression in this patient may contribute to the delayed production of HEV-IgA. It may therefore be better to measure HEV-IgA repeatedly with HEV-RNA to diagnose hepatitis E in immunosuppressed patients. A previous study reported that hepatitis E progressed to chronic hepatitis in 66% of organ transplantation recipients and all chronic hepatitis E infections were caused by HEV genotype 3.Citation10 In this case, HEV (genotype 3) infection did not progress to chronic hepatitis despite the patient taking immunosuppressive agents. The low titer of HEV-RNA of 4.3 log copy/mL (cutoff value: <2.0 log copy/mL) may have contributed to the HEV infection not progressing to a chronic infection. Further studies are required to investigate both the mechanism of progression of HEV infection to chronic hepatitis and the optimal testing and treatment of HEV in immunosuppressed patients.
Conclusion
We have described a case of acute hepatitis E in a renal transplant recipient. Careful interview regarding the possibility of consumption of HEV-contaminated food and repeated measurements of HEV-IgA were helpful in finalizing a diagnosis. Undercooked meat may be recommended to be excluded from menu in immunosuppressed patients such as recipients of organ transplantation.
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
We thank Simon Teteris, PhD, from the Edanz Group for editing the English in this manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
- DaltonHRBendallRIjazSBanksMHepatitis E: an emerging infection in developed countriesLancet Infect Dis200881169870918992406
- TeiSKitajimaNTakahashiKMishiroSZoonotic transmission of hepatitis E virus from deer to human beingsLancet2003362371373
- MatsudaHOkadaKTakahashiKMishiroSSevere hepatitis E virus infection after ingestion of uncooked liver from a wild boarJ Infect Dis200318894412964128
- KamarNKamarNSelvesJHepatitis E virus and chronic hepatitis in organ-transplant recipientsN Engl J Med200835881181718287603
- KamarNGarrousteCHaagsmaEBFactors associated with chronic hepatitis in patients with hepatitis E virus infection who have received solid organ transplantsGastroenterology20111401481148921354150
- OkamotoHGenetic variability and evolution of hepatitis E virusVirus Res200712721622817363102
- KamarNBendallRLegrand-AbravanelFHepatitis ELancet201237998352477248822549046
- HewittPEIjazSBrailsfordSRHepatitis E virus in blood components: a prevalence and transmission study in southeast EnglandLancet201438499561766177325078306
- GallianPLhommeSPiquetYHepatitis E virus infections in blood donors, FranceEmerg Infect Dis2014201914191725340881
- KamarNDaltonHRAbravanelFIzopetJHepatitis E virus infectionClin Microbiol Rev20142711613824396139
- TakahashiMKusakaiSMizuoHSimultaneous detection of immunoglobulin A (IgA) and IgM antibodies against hepatitis E virus (HEV) is highly specific for diagnosis of acute HEV infectionJ Clin Microbiol200543495615634950
