Abstract
Coronary artery disease is currently one of the leading causes of mortality in patients with HIV. Severe left main disease (LMD) occurs in ~6% of the HIV-infected patients. We describe a case report of an atypical presentation of silent critical LMD in an HIV-infected patient who underwent a low-risk exercise stress test. The cardiovascular disease team should be vigilant for this latent phenomenon, specifically within this subpopulation despite the high Duke treadmill score.
Key clinical message
Clinicians must be cognizant that patients with atypical chest pain infected with HIV may have silent critical left main coronary artery disease (CAD) despite being stratified as low risk after exercise stress test.
Introduction
CAD is currently one of the leading causes of mortality in patients with HIV. This is primarily attributed to their comparably increased life expectancy, antiretroviral induced metabolic derangements, and the lentivirus itself.Citation1,Citation2 The pathophysiology involves a complex milieu combining direct endothelial injury and dysfunction and hypercoagulability along with a significant contribution from traditional cardiac risk factors.Citation3–Citation5
Severe left main disease (LMD) occurs in ~3%–7% of overall patients undergoing index coronary angiography, and if treated with conservative medical management, a 3-year mortality rate of 50% was found.Citation6,Citation7 In the HIV-infected subpopulation, the prevalence is ~6% as demonstrated in the studies by Escaut et alCitation8 and Mehta and KhanCitation9.
Accruing epidemiologic data on asymptomatic LMD with silent myocardial ischemia is difficult; however, sudden cardiac death and autopsy studies suggest that this entity is relatively common.Citation10
We describe a case report of silent critical LMD in an HIV-infected patient who was stratified as low risk according to the Duke treadmill score (DTS) of 12 after exercise stress test.
Case report
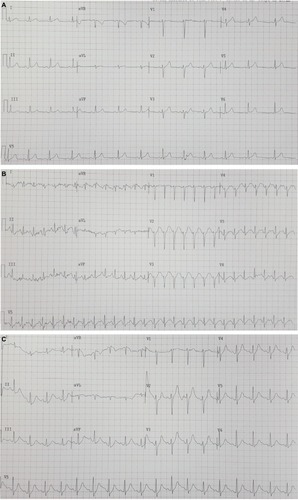
Recently, a 56-year-old Caucasian gentleman with a medical history of HIV infection for 10 years, undergoing antiretroviral therapy (ART) including efavirenz, emtricitabine, and tenofovir, initially presented to the outpatient cardiology clinic for atypical, noncardiac chest pain. His physical examination and vital signs were unremarkable. A 12-lead electrocardiogram (ECG) revealed sinus rhythm with no acute ischemic changes. Recent pertinent laboratory investigations included the following: a normal complete blood count, comprehensive metabolic panel, lipid panel, inflammatory markers such as erythrocyte sedimentation rate and C-reactive protein, glycosylated hemoglobin (HbA1c), cluster of differentiation 4 (CD4) count of 860 cells/mm3 (normal range, 500–1,500 cells/mm3), and undetectable HIV RNA levels (<20 RNA copies/µL). His cardiac troponin T was normal at 0.028 ng×mL−1 (normal range, 0–0.1 ng×mL−1) and did not reflect a myocardial infarction. He was subsequently risk stratified according to Bruce protocol exercise treadmill test, during which he did not report any anginal episodes and achieved 12 minutes and 23 seconds of exercise time with 13.2 metabolic equivalents (METs) and no significant ST-segment deviation. His DTS was calculated at 12, which is considered a low risk for cardiovascular events ().Citation11
Figure 1 Exercise stress ECGs.
Abbreviation: ECG, electrocardiogram.
The patient returned the following fortnight due to persistent atypical chest pain, and as a result, he was hospitalized for further management. Once again, ECGs and cardiac biomarkers of the patient were unremarkable. He was then proceeded to inpatient coronary angiography. Cardiac catheterization revealed an eccentric, critical mid-left main lesion with 90% stenosis (American College of Cardiology/American Heart Association [ACC/AHA] type C) with a diffuse, proximal left anterior descending artery (LAD) stenosis (). The left main lesion was unable to be further characterized with intravascular ultrasound or optical coherence tomography due to the unavailability of these imaging modalities. He remained hospitalized and subsequently underwent successful double coronary artery bypass grafting (CABG) the following day without complications. The patient was then safely discharged following his uneventful postoperative recovery on guideline-directed medical therapy which included aspirin 81 mg, clopidogrel 75 mg, lisinopril 2.5 mg, carvedilol 3.125 mg twice daily, spironolactone 12.5 mg, and pravastatin 20 mg in addition to his maintenance ART.
Figure 2 Left coronary artery angiography.
Abbreviation: LMCA, left main coronary artery.

All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The patient has provided written informed consent to have the details of his case published.
Discussion
Although the patient reported atypical chest pain, his symptoms were not considered to be related to the discovery of his severe left main coronary artery (LMCA) lesion, and thus, were initially considered noncardiac in nature. The mechanisms for the atypical presentation with a high DTS (>12) despite having severe LMD remain unclear. Possible reasons include ART-induced neuropathy which may have masked definitive typical angina or its equivalent along with an HIV-associated neuropathy despite the patient being well controlled as evidenced by his CD4 count and undetectable viral load. There was also no significant coronary collateral circulation present which could attenuate any classical symptoms.Citation12 To the authors’ knowledge, this is the reported first-in-human case of illustrating the phenomenon of an oligosymptomatic left main lesion in an HIV-infected patient who underwent a low-risk exercise treadmill test.
Generally, HIV-infected patients have a significantly higher risk of developing acute coronary syndromes (ACSs).Citation13 This is in part due to a thrombophilic phenomenon which is attributed to various cellular and plasmatic factors, including decreased levels of natural anticoagulants, increased levels of plasminogen activator inhibitor-1, activated protein C resistance, and platelet reactivity.Citation14 The patient proceeded to angiography based on the discordance between the atypical symptoms and a low-risk exercise stress test (DTS>12) despite the growing evidence that achieving ≥10 METs with a negative stress ECG resulted in 94% sensitivity and 97% negative predictive value in identifying high-risk CAD.Citation15
The prevalence of significant LMD appears to be 6%, which is equivalent to a non-HIV-infected cohort.Citation8,Citation9 Coronary anatomy seems to be variable, with some studies showing a higher prevalence of single-vessel disease and others multi-vessel disease.Citation16
CABG has long been considered as the gold standard treatment of unprotected LMCA disease. Currently, there is a dearth of studies with respect to surgical revascularization in HIV-infected patients.Citation17,Citation18 These surmised that both short- and long-term outcomes are similar to their noninfected counterparts with respect to cardiovascular mortality and prognosis.
With the advent of drug-eluting stents (DESs), together with advances in adjunctive pharmacotherapies, percutaneous coronary intervention (PCI) is also a feasible revascularization strategy for patients with unprotected LMCA stenosis.Citation19,Citation20 PCI in HIV-infected patients has been associated with a higher incidence of nonfatal reinfarction, restenosis, and in-stent thrombosis requiring repeat revascularization.Citation16,Citation21,Citation22 It has also been demonstrated that DESs display equivalent safety and efficacy in the HIV-infected population as in the general population.Citation23–Citation25
Conclusion
We describe a case report of an atypical presentation of silent critical LMD in an HIV-infected patient who underwent a low-risk exercise stress test. The cardiovascular disease team should be vigilant for this latent phenomenon, specifically within this subpopulation despite the high DTS and markedly above normal functional capacity. Although CABG remains the gold standard of care for the management of LMD, drug-eluting PCI remains a viable option with streamlined procedural techniques, cutting edge devices, and novel adjunctive pharmacology.
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
There was no funding for this case report.
Disclosure
The authors report no conflicts of interest in this work.
References
- WormSWDe WitSWeberRDiabetes mellitus, preexisting coronary heart disease, and the risk of subsequent coronary heart disease events in patients infected with human immunodeficiency virus: the data collection on adverse events of anti-HIV drugs (D:A:D study)Circulation2009119680581119188509
- WormSWSabinCWeberRRisk of myocardial infarction in patients with HIV infection exposed to specific individual antiretroviral drugs from the 3 major drug classes: the data collection on adverse events of anti-HIV drugs (D:A:D) studyJ Infect Dis2010201331833020039804
- MatetzkySDomingoMKarSAcute myocardial infarction in human immunodeficiency virus-infected patientsArch Intern Med2003163445746012588205
- BoccaraFMary-KrauseMTeigerEAcute coronary syndrome in human immunodeficiency virus-infected patients: characteristics and 1 year prognosisEur Heart J2011321415020965887
- SeecheranVKGiddingsSLSeecheranNAAcute coronary syndromes in patients with HIVCoron Artery Dis201728216617227845996
- CohenMVGorlinRMain left coronary artery disease. Clinical experience from 1964–1974Circulation19755222752851080085
- SoleimaniAAbbasiAKazzaziEHPrevalence of left main coronary artery disease among patients with ischemic heart disease: insights from the Tehran Angiography RegistryMinerva Cardioangiol200957217518319274028
- EscautLMonsuezJJChironiGCoronary artery disease in HIV infected patientsIntensive Care Med200329696997312739013
- MehtaNJKhanIAHIV-associated coronary artery diseaseAngiology200354326927512785019
- ShawlFAChunPKMutterMLAsymptomatic left main coronary artery disease and silent myocardial ischemiaAm Heart J198911735375422919533
- ShawLJPetersonEDShawLKUse of a prognostic treadmill score in identifying diagnostic coronary disease subgroupsCirculation19989816162216309778327
- MeierPSchirmerSHLanskyAJTimmisAPittBSeilerCThe collateral circulation of the heartBMC Med20131114323735225
- FreibergMSChangC-CHKullerLHHIV infection and the risk of acute myocardial infarctionJAMA Intern Med2013173861462223459863
- EnerRAPalermoJO’MurchuBBurkeJAWolfNMVan DeckerWAHIV disease in thrombocardiologyJ Invasive Cardiol200719523523917476040
- LöfflerAIPerezMVNketiahEOBourqueJMKeeleyECUsefulness of achieving ≥10 METs with a negative stress electrocardiogram to screen for high-risk obstructive coronary artery disease in patients referred for coronary angiography after exercise stress testingAm J Cardiol2017121328929329191566
- BoccaraFMary-KrauseMTeigerE012 Acute coronary syndrome in HIV-infected patients: characteristics and prognosisArch Cardiovasc Dis Suppl2011314
- FilsoufiFSalzbergSPvon HarbouKTJNeibartEAdamsDHExcellent outcomes of cardiac surgery in patients infected with HIV in the current eraClin Infect Dis200643453253616838245
- BoccaraFCohenAAngelantonioECoronary artery bypass graft in HIV-infected patients: a multicenter case control studyCurr HIV Res200861596418288976
- FajadetJChieffoACurrent management of left main coronary artery diseaseEur Heart J201233136b50b22210689
- DashDStenting of left main coronary artery stenosis: A to ZHeart Asia201351182727326065
- MestresCAChuquiureJEClaramonteXLong-term results after cardiac surgery in patients infected with the human immunodeficiency virus type-1 (HIV-1)Eur J Cardiothorac Surg200323610071016 discussion 101612829080
- BoccaraFEderhySJanowerSBenyounesNOdiGCohenAClinical characteristics and mid-term prognosis of acute coronary syndrome in HIV-infected patients on antiretroviral therapyHIV Med20056424024416011528
- RenXTrilesskayaMKwanDMNguyenKShawREHuiPYComparison of outcomes using bare metal versus drug-eluting stents in coronary artery disease patients with and without human immunodeficiency virus infectionAm J Cardiol2009104221622219576350
- SerruysPWMoriceM-CKappeteinAPPercutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery diseaseN Engl J Med20093601096197219228612
- ChristiansenEHMäkikallioTHolmNREverolimus-eluting stents or bypass surgery for left main coronary diseaseN Engl J Med2017376111087108928301104
