Abstract
At present, only one design is available for trifocal intraocular lens (IOL); unfortunately, this particular design is not suitable for implantation in the sulcus with optic capture when posterior capsule rupture (PCR) occurs. Although three-piece bifocal IOLs can be implanted in the sulcus, this form of IOL can be vulnerable to tilt and decentration, thus causing aberration and photopic phenomena, such as halos and glares. However, visual axis centered optic capture using femtosecond laser-assisted cataract surgery (FLACS) is able to manage such complex operations.
In the present study, we implanted a three-piece +4.0 D bifocal IOL into the sulcus of a patient who experienced PCR using optic capture and FLACS following the straightforward implantation of a one-piece trifocal IOL in the other eye. Defocus curves showed that the weakness of the trifocal IOL (nearest distances) was compensated for by the strength of the +4.0 D bifocal IOL, whereas the weakness of the +4.0 D bifocal IOL (middle distance) was compensated for by the strength of the trifocal IOL. Therefore, this combination provided the patient with a wider range of depth of focus. The contrast sensitivity in both eyes was within the normal range. Photopic phenomena were comparable with the bilateral implantation of the trifocal IOL. Anterior segment optical coherence tomography showed that tilt and decentration in the trifocal IOL implanted in the bag was significantly higher than the +4.0 D bifocal IOL implanted in the visual axis centered optic capture.
This case showed that the intraindividual implantation of a single-piece trifocal IOL in the bag and a three-piece +4.0 D bifocal IOL in the sulcus, using a combination of optic capture and FLACS, is promising particularly in cases of PCR and can provide a wider range of vision without losing visual quality.
Introduction
Various types of multifocal intraocular lens (IOL) have recently become available. It is important to be conversant with the pros and cons of IOLs. Single-piece trifocal IOLs have become popular since they provide three good focal points: distance, intermediate (1 m), and near vision (40 cm). In contrast, three-piece +4.0 D bifocal IOLs provide two focal points (distance and very near vision [30 cm]) and can be implanted in the sulcus using optic capture.Citation1–Citation3 However, each type of IOL has specific weaknesses. One of the weak points of trifocal IOLs is that only one design is currently available, which is not suitable for implantation in the sulcus when an undesirable event has occurred during operation. Another weak point is that the quality of very near vision for trifocal IOLs is slightly lower than +4.0 D bifocal IOLs.Citation4 On the other hand, the typical weaknesses of +4.0 D bifocal IOLs include lower visual performance at intermediate distance, and photic phenomena, such as halos and glare.Citation5 Under normal circumstances, implantation of a trifocal IOL in the bag in both eyes would be the most favorable option. Nevertheless, in certain circumstances, such as posterior capsule rupture (PCR), a second option needs to be prepared which meets patient expectation. In such cases, three-piece +4.0 D bifocal IOLs are available to implant into the sulcus; however, the performance of this type of IOL is still vulnerable to tilt and decentration and can induce even worse photic phenomena. Femtosecond lasers can create reproducible circularity and diameter during continuous curvilinear capsulorhexis (CCC). Consequently, implantation of three-piece +4.0 D bifocal IOLs using optic capture could represent an ideal option with which to manage such complex operations. This case report analyzed the visual performance outcome in a patient who agreed to have a three-piece +4.0 D bifocal IOL implanted in the sulcus using optic capture following a straightforward cataract operation with a single-piece trifocal in the bag.
Case report
A 68-year-old man arrived at our clinic with visually significant cataracts bilaterally. He had not received eye surgery previously. The preoperative corrected distance visual acuity was 20/30 in the right eye and 20/20 in the left eye, with a refraction of 6.0 to 1.5×140 and –6.5 to 1.25×150, respectively.
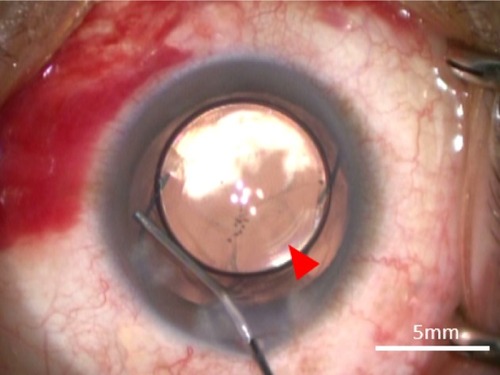
Femtosecond laser-assisted cataract surgery (FLACS) with implantation of a one-piece trifocal diffractive IOL with double C-loop haptics (Pod F FINE VISION, PhysIOL, Liège, Belgium) () was scheduled for both eyes. In the right eye, a trifocal diffractive IOL was implanted following a straightforward FLACS procedure. The same procedure was planned for the left eye 1 week later. As planned, FLACS was performed using the femtosecond laser (LenSx, Alcon Laboratories, Fort Worth, TX, USA); 5.0 mm capsulotomy centered on White-to-White was created with 8.0 mJ of energy (spot and layer separations: 9 µm each) (). Nuclear fragmentation was performed using the chop and cylinder technique with 8.0 mJ of energy (spot and layer separations: 9 µm each) (). An optical coherence tomography (OCT) line scan indicated that there was no abnormality in the posterior capsule (). While the cortex was aspirated, the posterior capsule foramen developed at the 9 o’clock position (). Anterior vitrectomy was performed to clear the vitreous from the anterior chamber and capsular bag. Since the foramen was located relatively peripherally, it was too large to implant a one-piece trifocal lens as planned. Consequently, a three-piece +4.0 D bifocal diffractive IOL with single C-loop haptics (Tecnis multifocal ZMA00, Abbott Medical Optics Inc., Santa Ana, CA, USA) () was placed in the sulcus using optic capture ().
Figure 1 Photographic image of the single-piece trifocal IOL (Pod F FINE VISION).

Figure 2 Intraoperative image taken during femtosecond laser surgery.
Notes: (A) 5.0 mm diameter CCC centered on White-to-White (pink circle). (B) Nuclear fragmentation using the cylinder and chop mode (yellow circle and eight pattern).
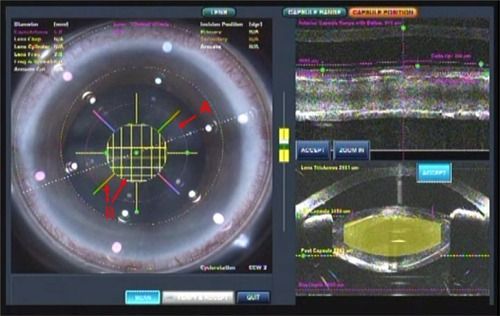
Figure 3 Image of the development of the posterior capsule foramen at the 9 o’clock position (red arrow).
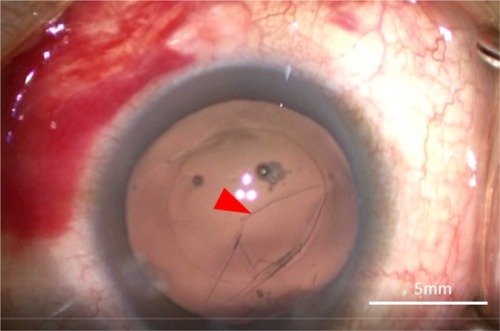
Figure 4 Photographic image of the three-piece +4.0 D bifocal IOL (ZMA00).

Figure 5 Image of optic capture involving the three-piece +4.0 D bifocal IOL.
Abbreviations: CCC, curvilinear capsulorhexis; IOL, intraocular lens.
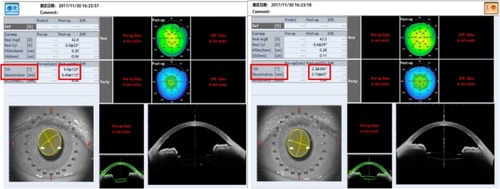
One month postoperatively, refraction was +0.25–0.25×100 in the right eye with the trifocal IOL and 0.00–0.25×180 in the left eye with the +4.0 D bifocal IOL, respectively. Uncorrected distance visual acuity was 30/20 in both eyes. Uncorrected intermediate visual acuity, uncorrected near visual acuity at 40 cm, and the uncorrected near visual acuity at 30 cm were 20/20, 20/30, and 20/40, respectively, in the right eye with the trifocal IOL. These were 20/20, 20/40, and 20/25, respectively, in the left eye with the +4.0 D bifocal IOL. The defocus curve in each eye was similar to the one in the trifocal IOL and the bifocal IOL, which were provided by the manufacturers (). A binocular defocus curve showed that the strength of each IOL compensated for the weaknesses in each type of IOL (). As a matter of fact, the patient’s satisfaction with each distance was high, and he noticed that the intermediate distance was covered by the right eye, whereas, the near distance of 30 cm was covered by the left eye. A contrast sensitivity test (Contrast Glaretester, Takagi, Japan) indicated that the contrast sensitivity in both eyes was within the normal range (). Anterior segment OCT (CASIA2, Tomey, Nagoya, Japan) showed that the degree of both tilt (degree) and decentration (mm) in the single-piece trifocal IOL implanted in the bag (9.9 and 0.49 mm) was higher than the three-piece bifocal IOL implanted in the sulcus using optic capture (2.3 and 0.10 mm) ().
Figure 6 (A) Defocus curve of the Fine Vision trifocal IOL (navy) ZMA00 bifocal IOL (green); right eye with the trifocal IOL (red) and left eye with the bifocal IOL (brown). The defocus curve for the Fine Vision trifocal IOL (navy) and ZMA00 bifocal IOL (green) was provided by the manufacturers. (B) Defocus curve for the right eye with the Fine Vision trifocal IOL (red); left eye with the ZMA00 bifocal IOL (brown) and both eyes (light blue).
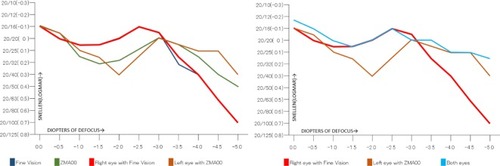
Figure 7 Postoperative contrast sensitivity in both eyes.
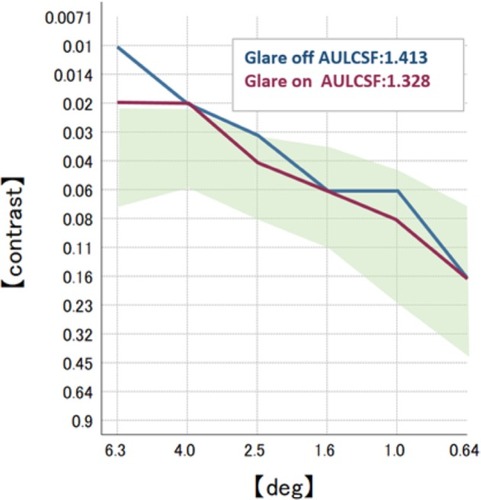
Figure 8 Image of the anterior segment OCT.
Abbreviations: IOL, intraocular lens; OCT, optical coherence tomography.
The patient provided informed written consent for the publication of his case details, and the accompanying images.
Discussion
This intraindividual research study analyzed the implantation of a one-piece trifocal IOL in the bag, and a three-piece bifocal IOL in the sulcus, using optic capture created by a femtosecond laser. Our findings indicated good visual outcomes and high patient satisfaction.
The trifocal IOL provides better intermediate visual acuity than the bifocal IOL in addition to good far and near vision.Citation6 Initially, we planned to implant the trifocal IOL into each eye. A trifocal IOL was placed into the bag in the right eye as planned. Unexpectedly, however, PCR occurred during the operation in the left eye; therefore, we had to discuss the choice of which IOL to implant based on their individual pros and cons. A one-piece trifocal diffractive IOL with double C-loop haptics limits implantation into an intact bag or a bag with a posterior CCC.Citation7 However, in our case, the PCR occupied a large area superiorly; it was therefore risky to create a posterior CCC to implant the trifocal IOL in the bag. Therefore, one option for implantation was a three-piece monofocal IOL or a bifocal IOL in the sulcus.Citation7 Technically speaking, a monofocal IOL is more suitable to place into the sulcus because the quality of vision of a bifocal IOL is more vulnerable to tilt and decentration.Citation8–Citation10 Optic capture is a valid option with which to deal with such circumstances.Citation10,Citation11 In the case of unforeseen events, such as our case, the implantation of a three-piece bifocal IOL into the sulcus using optic capture should be considered. Fortunately, since this cataract operation was performed by FLACS, the CCC was a suitable size and was round-shaped on the capsular bag. For this specific situation, the best choice for patient satisfaction was the implantation of a three-piece +4.0 D bifocal diffractive IOL with single C-loop haptics into the sulcus using optic capture.
While it is quite challenging for a manual procedure to achieve a completely round-shaped, well-centered and similarly-sized (ideal diameter for optic capture =5 mm) capsulotomy,Citation12 FLACS enables us to overcome this challenge.Citation12 In contrast to the manual procedure, FLACS can create a CCC with reproducible circularity and diameter in a desirable position within the anterior capsule.Citation13 As was the situation with our present case, FLACS can widen the range of IOL choice, even under complicated situations with a capsular bag.
Regarding the quality of vision, in our case, both the right eye with the trifocal IOL, and the left eye with the +4.0 D bifocal IOL, showed an almost identical defocus curve to the ones provided by the manufacturers. In a previous study, Mojzis et alCitation14 demonstrated that there was no significant difference in distant vision when compared between trifocal and +4.0 D bifocal IOLs. Our present case also showed comparable findings in terms of distant vision. Like most previous studies,Citation3,Citation15,Citation16 our present case demonstrated that the right eye with the trifocal IOL showed better intermediate vision (1 m) than the left eye with the +4.0 D bifocal IOL; the very near vision (30 cm) of the left eye was better than the right eye. The near vision (40 cm) of the right eye was comparable to that of the left eye. This result indicated that in the defocus curve, the strengths of each IOL could compensate for the weaknesses of each other, which was evident in the binocular defocus curve. CochenerCitation17 also presented comparable binocular visual outcome following the implantation of a trifocal IOL in one eye and a bifocal IOL in the other eye.
Previous research has indicated that a multifocal IOL can cause a significant reduction in contrast sensitivity compared to a monofocal IOL.Citation18–Citation21 In our case, the right eye with the trifocal IOL showed a slightly higher area under the log contrast sensitivity function than the left eye in the +4.0 D bifocal IOL. This difference, however, was not statistically significant, and both results were above average. This indicates that contrast sensitivity of the implantation of the trifocal and +4.0 D bifocal IOL in each eye can be comparable in a case in which the trifocal IOL was implanted in both eyes.
Photic phenomena, such as halos and glare, are also a major concern after a multifocal IOL implantation.Citation22,Citation23 While Al-Khateeb et alCitation24 found that these symptoms were more severe in a bifocal IOL than a trifocal IOL, CochenerCitation17 showed different results in which symptoms were more troublesome in a trifocal IOL than a bifocal IOL. Our case showed that both halos and glares in the right eye with the trifocal IOL were slightly milder than in the left eye with the +4.0 D bifocal IOL. In both eyes, the halos and glares were comparable with bilateral implantation of the trifocal IOL. In the patient’s questionnaire, there was no indication of issues relating to photic phenomena in everyday life, including night driving.
When it comes to the stabilization of refraction, optic capture can perform earlier anterior–posterior stabilization than in-the-bag IOL placement. Indeed, in-the-bag IOL placement can cause delayed myopic shift more frequently than optic capture.Citation25 Stitfter et alCitation26 reported that in most cases, in-the-bag IOL placement can show forward movement in the first few weeks after operation, and forward or backward movement between 3 months and 1 year postoperation. This phenomena can cause continuous refractive change; such a tendency was also seen in our case. While refraction in the right eye with the single-piece trifocal IOL in the bag showed myopic shift for 6 months postoperation, the left eye, implanted with the three-piece bifocal IOL in the sulcus using optic capture, demonstrated no refractive shift after the operation. Consequently, the refraction with optic capture is most probably stabilized sooner than that with in-the-bag IOL placement, which can offer more accurate postoperative refraction.Citation27 FLACS can consistently offer an accurate diameter of CCC which enables us to place IOLs in the sulcus using optic capture without overstretching the capsule and risking a tear in the capsule. Furthermore, some studies have reported that IOL implantation by optic capture in the center of the visual axis shows better visual outcome than others.Citation28 While it is not a problem for experienced surgeons to create a CCC of the same size consistently, the FLACS method is superior to the manual procedure in that it can consistently produce a CCC on the visual axis. Given the fact that FLACS enables us to create optic capture at a desirable position, even in our case, optic capture should have been positioned in the center of the visual axis, rather than the center of the White-to-White. As a matter of fact, the recently released IOL, known as FEMI-NIS (Oculentis, Berlin, Germany), is specially designed to implant into the bag with optic capture in the center of the visual axis created by FLACS, and is expected to show better performance in terms of the quality of vision.Citation29
In conclusion, our present case showed that intraindividual implantation of a trifocal IOL in the bag, and a +4.0 D bifocal IOL in the sulcus, using optic capture created by FLACS is a promising technique, since the strength of each IOL supplemented their own weaknesses, thus leading to a wider depth of focus. This is particularly useful for when unanticipated PCR occurs because it ensures that the outcome of the operation can still live up to patient expectation. Furthermore, FLACS can play an important role in performing this technique in a consistent and predictable manner.
Acknowledgments
All researchers involved in this case study have no affiliations with or involvement in any organization or entity with any financial interest or nonfinancial interest.
Disclosure
The authors report no conflicts of interest in this work.
References
- MojzisPKukuckovaLMajerovaKLiehneovaKPiñeroDPComparative analysis of the visual performance after cataract surgery with implantation of a bifocal or trifocal diffractive IOLJ Refract Surg2014301066667225291749
- KaymakHBreyerDAlióJLCochenerBVisual performance with bifocal and trifocal diffractive intraocular lenses: a prospective three-armed randomized multicenter clinical trialJ Refract Surg2017331065566228991332
- GatinelDHoubrechtsYComparison of bifocal and trifocal diffractive and refractive intraocular lenses using an optical benchJ Cataract Refract Surg20133971093109923692884
- MaxwellAHollandECibikLClinical and patient-reported outcomes of bilateral implantation of a +2.5 diopter multifocal intraocular lensJ Cataract Refract Surg2017431294128317674
- CarsonDLeeSAlexanderEWeiXLeeSComparison of two laboratory-based systems for evaluation of halos in intraocular lensesClin Ophthalmol20181238539329503526
- KohnenTTitkeCBöhmMBeuro;ohm M. Trifocal intraocular lens implantation to treat visual demands in various distances following lens removalAm J Ophthalmol2016161717726432565
- Al-KhateebGShajariMKohnenTIntraindividual comparative analysis of the visual performance after cataract surgery with implantation of a trifocal and a bifocal intraocular lensJ Cataract Refract Surg201743569569828602334
- EppigTScholzKLöfflerAMeßnerALangenbucherAEffect of decentration and tilt on the image quality of aspheric intraocular lens designs in a model eyeJ Cataract Refract Surg20093561091110019465297
- SauerTMesterUTilt and decentration of an intraocular lens implanted in the ciliary sulcus after capsular bag defect during cataract surgeryGraefes Arch Clin Exp Ophthalmol20132511899322940795
- YangHCChungSKBaekNHDecentrationBNHDecentration, tilt, and near vision of the Array multifocal intraocular lensJ Cataract Refract Refractive Surgery2000264586589
- GimbelHVAmritanandAReverse optic capture to stabilize a toric intraocular lensCase Rep Ophthalmol20134313814324163682
- FriedmanNJPalankerDVSchueleGFemtosecond laser capsulotomyJ Cataract Refract Surg20113771189119821700099
- NagyZTakacsAFilkornTSaraybaMInitial clinical evaluation of an intraocular femtosecond laser in cataract surgeryJ Refract Surg200925121053106020000286
- MojzisPKukuckovaLMajerovaKLiehneovaKPiñeroDPComparative analysis of the visual performance after cataract surgery with implantation of a bifocal or trifocal diffractive IOLJ Refract Surg2014301066667225291749
- ZhaoGZhangJZhouYHuLCheCJiangNVisual function after monocular implantation of apodized diffractive multifocal or single-piece monofocal intraocular lensJ Cataract Refract Surg201036228228520152611
- NuijtsRMMAJonkerSMRKauferRABilateral implantation of +2.5 D multifocal intraocular lens and contralateral implantation of +2.5 D and +3.0 D multifocal intraocular lenses: Clinical outcomesJ Cataract Refract Surg201642219420227026442
- CochenerBProspective clinical comparison of patient outcomes following implantation of trifocal or bifocal intraocular lensesJ Refract Surg201632314615127027620
- PiehSWeghauptHSkorpikCContrast sensitivity and glare disability with diffractive and refractive multifocal intraocular lensesJ Cataract Refract Surg19982456596629610449
- CillinoSCasuccioAdi PaceFOne-year outcomes with new-generation multifocal intraocular lensesOphthalmology200811591508151618538402
- KohnenTAllenDBoureauCEuropean multicenter study of the AcrySof ReSTOR apodized diffractive intraocular lensOphthalmology20061134578584
- SheppardALShahSBhattUBhogalGWolffsohnJSVisual outcomes and subjective experience after bilateral implantation of a new diffractive trifocal intraocular lensJ Cataract Refract Surg201339334334923332118
- de VriesNEWebersCABTouwslagerWRHDissatisfaction after implantation of multifocal intraocular lensesJ Cataract Refract Surg201137585986521397457
- SoodPWoodwardMAPatient acceptability of the Tecnis multifocal intraocular lensClin Ophthalmol2011540341021499564
- Al-KhateebGShajariMKohnenTIntraindividual comparative analysis of the visual performance after cataract surgery with implantation of a trifocal and a bifocal intraocular lensJ Cataract Refract Refractive Surgery2017435695698
- MenapaceRPosterior capsulorhexis combined with optic buttonholing: an alternative to standard in-the-bag implantation of sharp-edged intraocular lenses? A critical analysis of 1000 consecutive casesGraefes Arch Clin Exp Ophthalmol2008246678780118425525
- StifterEMenapaceRLukschANeumayerTSacuSAnterior chamber depth and change in axial intraocular lens position after cataract surgery with primary posterior capsulorhexis and posterior optic buttonholingJ Cataract Refract Surg200834574975418471628
- ScottWJOwsiakRRFemtosecond laser–assisted primary posterior capsulotomy for toric intraocular lens fixation and stabilizationJ Cataract Refract Surg20154181767177126432136
- VersacePAngle kappa as a determinant of success with multifocal IOLsPaper presented at: The XXXIV Congress of the ESCRSSeptember 10–14; 2017Copenhagen, Denmark
- CummingsACapsulorhexis reconsidered. Eurotimes Stories Available from: http://www.eurotimes.org/capsulorhexis-reconsidered/Accessed September 10, 2018
