Abstract
Introduction
Primary intestinal lymphangiectasia (PIL) is a very rare disorder usually diagnosed before the third year of life or later in adulthood, presenting with pitting edema, hypoproteinemia and low immunoglobulin levels. The location and the extent of the affected bowel greatly influence the clinical manifestation. The localized or segmental form of PIL is extremely rare with only five pediatric cases reported worldwide.
Case presentation
A 10 year-old Caucasian boy presented with 3 months history of recurrent abdominal pain and a 1 month history of diarrhea. An ultrasound scan was performed on two separate occasions 10 days apart, revealing a growing cystic mass on the right side of the abdomen, in front of the psoas muscle. Subsequently an MRI scan confirmed that the mass originated from the mesenteries and infiltrates a short segment of the small bowel. Surgical resection of the affected segment was performed. Histopathological examination of the removed segment of ileum was consistent with intestinal lymphangiectasia. We could not identify any associated genetic syndromes or any other conditions that could have caused secondary intestinal lymphangiectasia. The patient’s recovery from surgery was uneventful and no recurrence was observed in the following 4 years.
Conclusion
Despite being a benign condition, mortality of PIL can be as high as 13% due to the difficulties associated with the management of the disease. PIL should be considered as a rare but potential cause for an abdominal mass, even in the older child, when cystic mesenterial involvement might be seen on ultrasound or MRI. In selected cases of PIL affecting only a short segment of the bowel or following unsuccessful conservative treatment, surgical resection of the affected bowel segment can be curative.
Introduction
Primary intestinal lymphangiectasia (PIL), also called as Waldman’s disease is a rare disorder usually diagnosed before 3 years of age or later in adulthoodCitation1 presenting with protein-losing enteropathy, hypoproteinemia and consequent clinical edema.Citation2 PIL is thought to be a congenital disorder with abnormal lymphatic drainage of the small bowel. The pathophysiology of the disorder is poorly understood. According to one of the proposed theories, lymphatic hypoplasia leads to obstruction of lymph flow of the intestines.Citation3 Several genes have been identified, which are responsible for lymphogenesis such as VEGFR3, SOX18, FOXC2, CCBE1.Citation4 PIL might present with a wide range of abnormal laboratory biochemical values and different symptoms based on the extent and exact location of the bowel segment involved. Histopathologic findings are characterized by the presence of lacteal juice, dilated mucosal and submucosal lymphatic vessels shown also in the serosa.Citation1
The condition rarely presents in the older child and usually involves a larger bowel segment if not generalized. Localized form of PIL is extremely rare with only five pediatric cases reported in the literature.
The authors present a case of a 10-year-old boy, with abdominal pain, with a localized mass in front of the right psoas muscle involving the mesenteries, successfully treated with surgical resection.
Case presentation
A 10-year-old boy presented to our outpatient clinic with abdominal pain. He reported recurrent epigastrial pain for the past 3–4 months, which has increased in severity and frequency, thus prompting the parents to seek medical help. The patient also developed diarrhea during the last month prior to presentation. On closer questioning, he described awakening at night with pain, accompanied by sweating and extreme paleness during the painful episodes. The description of the symptoms was alarming, prompting further investigation.
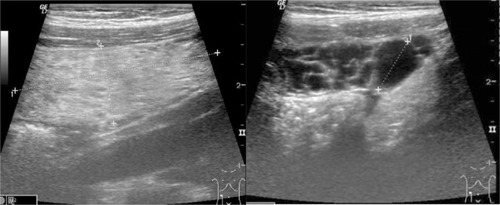
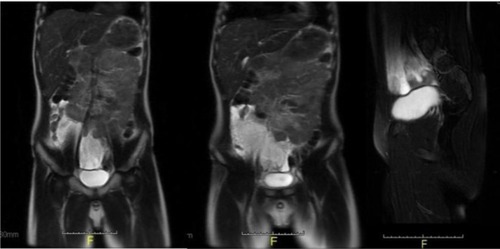
On clinical examination he did not have specific findings: he was pale and his lower abdomen was tender and full. Routine full blood count and biochemistry revealed normal values apart from a slight normocytic anemia, the patient was found to have normal immunoglobulin levels. A subsequent abdominal ultrasound (US) showed an ~20–22 mm-wide band-like cystic mass stretching in front of the right psoas muscle and above the bladder. A follow-up US 10 days later, by the same radiologist identified a gross increase in the size of the abdominal mass, now dislocating the bowels and causing an obstruction (). In order to specify the exact location, origin and nature of the mass, an abdominal MRI scan was performed. Based on the imaging, we had a strong suspicion of dealing with a solid tumor originating from the retroperitoneal space or the mesenteries ().
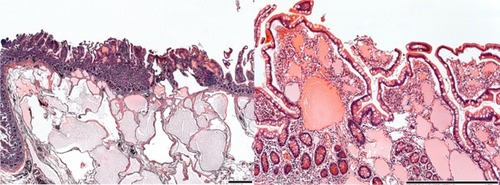
Pediatric surgeons performed a laparotomy. They located the mass to be in the middle part of the ileum and the attaching mesentery containing numerous cysts with localized infiltration of the bowel wall. A 30 cm long, macroscopically abnormal part of the ileum was resected. Pathologic examination was consistent with intestinal lymphangiectasia based on the dilated lymphatic system/vessels in the submucosa, subserosa and even in lamina propria (). The edges of the resection line revealed normal histologic features.
Figure 3 Microscopic picture showing typical changes for PIL: dilated lymphatics in subserosa, submucosa and lamina propria.
Abbreviation: PIL, primary intestinal lymphangiectasia.
Secondary causes of intestinal lymphangiectasia (IL) (eg, cardiac conditions, lymphoma, mesenteric tuberculosis, etc)Citation5 or associated conditions described in the literature (Noonan, Turner, Klippel-Trenaunay, Hennekam, von Recklinghausen syndrome)Citation6 were not identified. Family history was negative for PIL and also free of inherited disorders.
The early postoperative period was uneventful, and there were no complications. The patient’s symptoms subsided, with no further signs of PIL during follow-ups for the next 4 years; he had only occasional abdominal symptoms for which he was started on proton pump inhibitor (PPI). Albumin and immunoglobulin levels stayed within normal range for his age. Serial abdominal USs have not revealed any signs of recurrence up to date.
Discussion and conclusion
Although intestinal lymphangiectasia is a condition usually involving various lengths of the small bowel and presents with a protein-losing enteropathy,Citation7 there has been very few pediatric case reports about intestinal lymphangiectasia treated with bowel resection. Despite a thorough literature search, we could only identify five cases of PIL treated surgically (). All patients were male, with the age at presentation ranging from 0 to 10 years. Two PIL cases presented in infancy, one of these diagnosed in utero. Only one patient had undergone surgery as a rescue treatment after unsuccessful conservative management. The remaining two patients presented as acute abdomen and recurrent abdominal pain similar to our case. Various investigation tools were used, radiation-free US and MRI preferable in children.Citation13 All patients are symptom free after surgery with various follow-up times (1 month to 6 years).
Table 1 Pediatric localised PIL cases treated successfully with surgical resection.
Interestingly, in our case, no signs or symptoms were present typical for PIL, like protein losing enteropathy and consequent edema, low levels of albumin and immunoglobulins. According to our hypothesis typical signs were not present due to a very early diagnosis and because of the involvement of a short bowel segment (only 30 cm section of the ileum was affected)
Typical signs and symptoms are universally present in generalized/diffuse type of PILCitation1 and in most of localized PIL cases.Citation14 Only two adultCitation14 and only one pediatric reportCitation10 were similar to our case in view of normal biochemical values and absence of edema, all these patients presented acutely.
The principal treatment for PIL is mainly conservative: high-protein and low-fat diet with medium-chain-triglyceride supplementation, the dietary intervention being more effective in children than in adults.Citation15 In addition to diet, supportive measures (albumin infusion, total parenteral nutrition) are usually needed, especially in nonresponders. Further pharmacological treatment includes octreotide and tranexamic acid, their beneficial effect proven by several case reports.Citation2
In the treatment algorithm of PIL surgical intervention is only reserved for localized or therapy-refractory cases. Most of the reported “successfully treated by surgical resection” PIL cases, like ours, are diagnosed intraoperatively/postoperatively.
Whether surgical treatment should be considered in an earlier phase of the treatment process, would need bigger numbers and further investigation.
Four years following surgery, the patient is symptom-free with normal biochemical values. Close ultrasound and laboratory monitoring showed no further abnormalities; at present we believe that surgery was curative in our case.
Localized IL diagnosed at early stage can present with normal albumin and immunoglobulin levels.
Surgical removal of the affected bowel segment could be curative, with close monitoring of the biochemical values and surveillance with abdominal US.
Pediatric ultrasound may be a useful, noninvasive tool to lead to the diagnosis of IL and also play a role as a radiological surveillance tool for recurrence.
Based on the index cases resection of the affected bowel segment might be considered at an early stage in the treatment algorithm of pediatric PIL.
Although more than 90% of chronic abdominal pain in pediatric population is diagnosed as functional after evaluation, on rare occasions extraordinary diagnoses can be made based on radiologic and histologic findings; therefore, we think that the rare diagnosis of IL should be considered when dealing with chronic, recurrent abdominal pain with warning symptoms.
Consent for Publication
Written informed consent was obtained from the patient’s parents to publish this case report and any accompanying images. According to the standard of operating procedure of the Institutional Review Board of our University (SZTE University, Szeged, Hungary), publishing a case report is exempted from the board review.
Acknowledgments
The authors thank Krisztian Sisak gratefully for revising the manuscript. The authors also thank the patient’s family for their understanding and cooperation.
Disclosure
The authors report no conflicts of interest in this work.
References
- VignesSBellangerJPrimary intestinal lymphangiectasia (Waldmann’s disease)Orphanet J Rare Dis200831518294365
- AlshikhoMJTalasJMNoureldineSIIntestinal lymphangiectasia: insights on management and literature reviewAm J Case Rep20161751252227440277
- LevineCPrimary disorders of the lymphatic vessels—a unified conceptJ Pediatr Surg19892432332402709285
- HokariRKitagawaNWatanabeCChanges in regulatory molecules for lymphangiogenesis in intestinal lymphangiectasia with enteric protein lossJ Gastroenterol Hepatol2008237 Pt 2e88e9518005011
- LevittDGLevittMDProtein losing enteropathy: comprehensive review of the mechanistic association with clinical and subclinical disease statesClin Exp Gastroenterol20171014716828761367
- HennekamRCGeerdinkRAHamelBCAutosomal recessive intestinal lymphangiectasia and lymphedema, with facial anomalies and mental retardationAm J Med Genet19893445936002624276
- FreemanHJNimmoMIntestinal lymphangiectasia in adultsWorld J Gastrointest Oncol201132192321364842
- PersićMBrowseNLPrpićIIntestinal lymphangiectasia and protein losing enteropathy responding to small bowel restrictionArch Dis Child1998782194
- UğuralpSMutusMKutluOCetinSBaysalTMizrakBPrimary intestinal lymphangiectasia: a rare disease in the differential diagnosis of acute abdomenJ Pediatr Gastroenterol Nutr200133450851011698774
- KatochPBhardwajSLymphangiectasia of small intestine presenting as intussusceptionIndian J Pathol Microbiol200851341141218723975
- KimNRLeeSKSuhY-LPrimary intestinal lymphangiectasia successfully treated by segmental resections of small bowelJ Pediatr Surg20094410131719159713
- MitsiakosGDrogoutiEDrogoutiMDoitsidisCPazarliESpyridakisICongenital intestinal lymphangiectasia. A case reportJ Pediatr Neonatal Individ Med201871070106
- MaloneLJFentonLZWeinmanJPAnagnostMRBrowneLPPediatric lymphangiectasia: an imaging spectrumPediatr Radiol201545456256925301383
- HuberTPascholdMEckardtAJLangHKneistWSurgical therapy of primary intestinal lymphangiectasia in adultsJ Surg Case Rep201520157rjv08126169531
- WenJTangQWuJWangYCaiWPrimary intestinal lymphangiectasia: four case reports and a review of the literatureDig Dis Sci201055123466347220198428