Abstract
Purpose
To report a case of unilateral central retinal vein occlusion (CRVO) with central retinal artery occlusion (CRAO) in a patient with elevated Factor VIII.
Case presentation
A 48-year-old woman presented with a complaint of decreased visual acuity in her left eye that began 6 weeks prior. The patient had diabetes. The best-corrected visual acuity (BCVA) was hand motion, IOP was 34 mmHg, and there was a neovascularization of the iris in the left eye. A complete fundus evaluation including fluorescein angiography showed non-proliferative diabetic retinopathy in the right eye and CRVO with CRAO in the left eye. Systemic evaluation revealed elevated fibrinogen and Factor VIII suggestive of the diagnosis of thrombophilia due to elevated Factor VIII. This symptom was the first sign of the underlying disorder. IOP was normalized 1 week after IOP lowering agents were applied. Intravitreal anti-vascular endothelial growth factor treatment and pan-retinal photocoagulation were performed in the left eye. Additionally, to treat thrombophilia, warfarin treatment was started and flame-shaped retinal hemorrhage with cotton wool patch near the optic disc and around the retinal vascular arcade at the posterior pole had occurred in the right eye during treatment. Then, warfarin treatment was discontinued and retinal hemorrhage was decreased. In the left eye, the BCVA did not change during treatment.
Conclusion
Elevated levels of Factor VIII as an independent risk in the development of venous thromboembolism. Combined cases usually present with severe visual loss and such patients should be thoroughly evaluated to diagnose underlying factors including Factor VIII, and initiate appropriate management at the earliest.
Introduction
Retinal vascular occlusion, which includes central retinal vein occlusion (CRVO) and central retinal artery occlusion (CRAO), are not uncommon in the elderly age group because of commonly found underlying conditions like hypertension, dyslipidemia, diabetes, and so on.Citation1 In younger age group, inherited and acquired thrombophilia and inflammation of retinal vessels remain the major cause for retinal vascular disorders.Citation2–Citation4 Elevated Factor VIII levels are independent risk factors in the development of idiopathic venous thromboembolism (VTE).Citation5,Citation6 Glueck et alCitation7 reported CRVO patients were more likely than normal controls to have high Factor VIII (odds ratio 2.47, 95% confidence intervals: 1.31–7.9). This case describing combined CRVO and CRAO linked to elevated Factor VIII is a rare instance and may be the first of its kind to be reported to our knowledge. We have obtained written consent from the patient to have the case details and any accompanying images published, and this is a retrospective case report that we concluded the approval of the Institutional Review Board is not necessary.
Materials And Methods
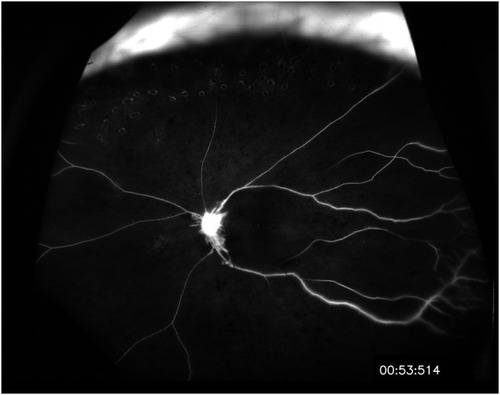
A 48-year-old woman presented with a decreased visual acuity in her left eye that began 6 weeks prior. The patient stated that there was no disease other than diabetes. The best-corrected visual acuity was 20/25 in the right eye and the patient was able to appreciate hand motion in the left eye. In the left eye, the IOP was 34 mmHg and anterior segment examination revealed neovascularization of the iris. Fundus findings were suggestive of left eye CRVO and CRAO. That is, blurred optic disc margin with flame-shaped retinal hemorrhages near optic disc and few blot hemorrhages at mid-periphery of the retina. And, ghost retinal vessels in all four quadrants and retinal whitening at the posterior pole and increased hyperreflectivity of the inner retinal and nerve fiber layers ( and ). Fluorescein angiography revealed delayed filling of retinal arteries with the arm-to-retina time of 18 s in the affected eye. Choroidal circulation was rarely seen, perfusion of retinal veins was faintly appreciable after 1 min suggestive of impaired retinal and choroidal circulation ().
Figure 1 Ultrawide fundus photograph (A) and conventional fundus photograph (B) of the patient at 6 weeks after the symptom occurred. A blurred optic disc margin, with flame-shaped retinal hemorrhages near the optic disc and a few dot-and-blot hemorrhages at the mid-periphery of the retina. Informed consent was submitted by the patient.
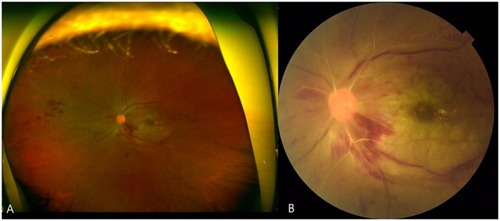
Figure 2 Optical coherence tomography of the patient at 6 weeks after the symptom occurred. Increased hyperreflectivity of the inner retinal and nerve fiber layer and diffuse retinal atrophy at temporal side. Informed consent was submitted by the patient.
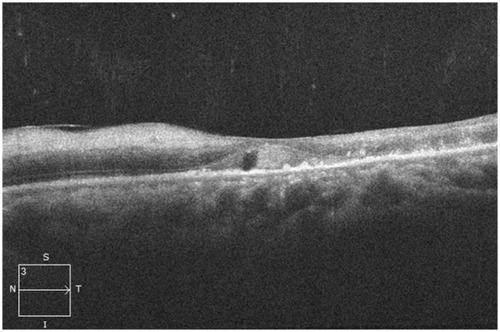
Figure 3 Fluorescein angiography of the patient at 6 weeks after the symptom occurred. Choroidal circulation was rarely seen; perfusion of retinal veins was faintly appreciable after 1 min, indicating impaired retinal and choroidal circulation. Informed consent was submitted by the patient.
Complete blood count, renal function tests, and extended lipid profile were within normal limits. HIV, Venereal Disease Research Laboratory test, rheumatoid factors, and antinuclear antibodies were investigated to rule out the underlying causes of vasculitis. Hematological tests, such as activated prothrombin time, international normalized ratio were within normal limits. But, erythrocyte sedimentation rate was elevated (73mm), prothrombin time was near the lower limit and hemoglobin A1c was elevated (11.7%). Fibrinogen was increased to 554mg/dL and Factor VIII was increased to 560%. Immunologic assay for protein C antigen and protein S antigen showed normal levels.
Systemic evaluation revealed elevated fibrinogen and Factor VIII suggestive of the diagnosis of thrombophilia. The ocular symptom was the first sign of the underlying disorder. IOP was normalized 1 week after IOP lowering agents were applied. Intravitreal anti-vascular endothelial growth factor treatment and pan-retinal photocoagulation were performed in the left eye.
Results
Additionally, to treat thrombophilia, the patient was referred to a hematologist, and anticoagulants oral warfarin was started.
Discussion
Our patient experienced a sudden visual loss due to a combined retinal vein occlusion (RVO) and retinal artery occlusion (RAO). The etiologies may be mechanical compression of the optic nerve, such as inadvertent retrobulbar injection in the optic nerve sheath, optic nerve inflammation from systemic disease or orbital inflammatory pseudotumor.Citation8–Citation10 Additionally, systemic disorders may also cause combined RVO and RAO, such as protein C deficiency, systemic lupus erythematous, antiphospholipid syndrome, and PAX3 mutation with Waardenburg syndrome type 1.Citation11–Citation13
The Leiden Thrombophilia study was the first to report that the level of clotting Factor VIII influences the risk of VTE. They reported that Factor VIII coagulant activity levels remained a significant independent risk factor.Citation14 In 2011, Ota et al have reported that elevated plasma level of Factor VIII is a risk factor for VTE and Factor VIII levels above the 75th percentile are associated with a significant odds ratio for the occurrence of VTE in Asian.Citation15 Searching at the ophthalmic division, Glueck et al have described that CRVO cases were more likely than controls to have high Factor VIII (odds ratio 2.47, 95% confidence intervals: 1.96–38) and treatable thrombophilia is more common in RVO cases than in normal controls.Citation7
Factor VIII is a plasma sialoglycoprotein that plays an essential role in normal hemostasis by acting as a critical cofactor for the serine protease, activated Factor IX. Following the initiation of coagulation, plasma Factor VIII is cleaved and activated by thrombin. The resulting Factor VIIIa (activated Factor VIII) heterotrimer is released from its complex with VWF, and is then able to interact with exposed anionic phospholipids, where it functions as a non-enzymatic cofactor for Factor IXa (activated Factor IX) in the activation of Factor X. In view of the critical cofactor function of Factor VIIIa, it is not surprising that FVIII levels have been predicted to influence the rate of thrombin generation.Citation16
We cannot be sure that CRVO and CRAO can develop simultaneously or consequentially. In our patients, we presumed that consequential occlusion of vein and artery is more likely. Considering the high plasma Factor VIII, we thought that CRVO would have occurred first. According to Hayreh’s theory, after the occurrence of CRVO, the lack of central retinal vein tributaries anterior to the site of occlusion leads to complete hemodynamic block of retinal circulation causing secondary CRAO and presenting as combined CRVO with CRAO.Citation17
To the best of our knowledge, this is the first report of CRAO following CRVO in a middle-age patient and the cause was presumed as hematologic disorder.
Young patients presenting with the combined occlusion of central retinal artery and vein should be evaluated in detail because distinction between thrombotic and inflammatory etiology is important for proper management. Ocular and systemic management for patients with high plasma Factor VIII during acute phase mainly relies on systemic anticoagulation therapy and proper ocular management.
Conclusion
Although unilateral involvement of combined CRVO and CRAO in the young age group, the patient may have a systemic underlying etiology. And the patient having such presentation should be thoroughly evaluated to diagnose underlying conditions and initiate appropriate management as soon as possible.
Disclosure
The authors report no conflicts of interest in this work.
References
- Özdek Ş, Yülek F, Gürelik G, Aydin B, Hasanreisoǧlu B. Simultaneous central retinal vein and retinal artery branch occlusions in two patients with homocystinaemia. Eye. 2004;18(9):942. doi:10.1038/sj.eye.670132015002016
- Sottilotta G, Oriana V, Latella C, et al. Role of hyperhomocystinemia in retinal vascular occlusive disease. Clin Appl Thromb Hemost. 2007;13(1):104–107. doi:10.1177/107602960629642317164500
- Kuo JZ-C, Lai -C-C, Ong FS-C, et al. Central retinal vein occlusion in a young Chinese population: risk factors and associated morbidity and mortality. Retina. 2010;30(3):479. doi:10.1097/IAE.0b013e3181b9b3a020010454
- Marcucci R, Sofi F, Grifoni E, Sodi A, Prisco D. Retinal vein occlusions: a review for the internist. Intern Emerg Med. 2011;6(4):307–314. doi:10.1007/s11739-010-0478-221547483
- Reitsma PH, Prins MH, van Den Ende A, Biiller HR. High plasma concentration of factor VIIIc is a major risk factor for venous thromboembolism. Thromb Haemost. 2000;83:5–9.10669145
- Kyrle PA, Minar E, Hirschl M, et al. High plasma levels of factor VIII and the risk of recurrent venous thromboembolism. N Engl J Med. 2000;343(7):457–462. doi:10.1056/NEJM20000817343070210950667
- Glueck CJ, Hutchins RK, Jurantee J, Khan Z, Wang P. Thrombophilia and retinal vascular occlusion. Clin Ophthalmol. 2012;6:1377. doi:10.2147/OPTH.S3462722969282
- Torres RJDA, Luchini A, Weis W, Frecceiro PR, Casella M. Combined central retinal vein and artery occlusion after retrobulbar anesthesia: report of two cases. Arq Bras Oftalmol. 2005;68(2):257–261. doi:10.1590/S0004-2749200500020002015905952
- Shukla D, Arora A, Hadi KM, Kumar M, Baddela S, Kim R. Combined central retinal artery and vein occlusion secondary to systemic non-Hodgkin’s lymphoma. Indian J Ophthalmol. 2006;54(3):204. doi:10.4103/0301-4738.2707716921223
- Foroozan R. Clinical case notes: combined central retinal artery and vein occlusion from orbital inflammatory pseudotumour. Clin Exp Ophthalmol. 2004;32(4):435–437. doi:10.1111/j.1442-9071.2004.00850.x15281983
- Desai S, Rai N, Kulkarni P, Natarajan S. Combined CRVO with CRAO in a patient with protein C deficiency. Retin Cases Brief Rep. 2014;8(2):145–149. doi:10.1097/ICB.000000000000002725372333
- Durukan AH, Akar Y, Bayraktar MZ, Dinc A, Sahin OF. Combined retinal artery and vein occlusion in a patient with systemic lupus erythematosus and antiphospholipid syndrome. Can J Ophthalmol. 2005;40(1):87–89.15825539
- Choi EY, Choi W, Lee CS. A novel PAX3 mutation in a Korean patient with Waardenburg syndrome type 1 and unilateral branch retinal vein and artery occlusion: a case report. BMC Ophthalmol. 2018;18(1):266. doi:10.1186/s12886-018-0933-930314436
- Koster T, Vandenbroucke J, Rosendaal F, Briët E, Blann A. Role of clotting factor VIII in effect of von Willebrand factor on occurrence of deep-vein thrombosis. Lancet. 1995;345(8943):152–155. doi:10.1016/s0140-6736(95)90166-37823669
- Ota S, Yamada N, Ogihara Y, et al. High plasma level of factor VIII. Circ J. 2011;75(6):1472–1475. doi:10.1253/circj.cj-10-105121498909
- Butenas S, Van’t Veer C, Mann KG. “Normal” thrombin generation: presented in part at the XVIth Congress of the International Society on Thrombosis and Haemostasis. Blood. 1999;94(7):2169–2178.10498586
- Hayreh SS. Prevalent misconceptions about acute retinal vascular occlusive disorders. Prog Retin Eye Res. 2005;24(4):493–519. doi:10.1016/j.preteyeres.2004.12.00115845346
