Abstract
Background
Masquerading bundle branch block (MBBB) is a rare and important electrocardiographic pattern. It consists of right bundle branch block (RBBB) in precordial leads and left bundle branch block (LBBB) in limb leads. It indicates advanced conduction system abnormality usually associated with severe underlying heart disease. MBBB is associated with poor prognosis. MBBB patients are at increased risk of complete atrioventricular (AV) block. To our knowledge, there is no previous published report of MBBB in heart failure in Nigeria.
Aim
To present a case of an African patient with heart failure and masquerading bundle branch block, a rare and important finding on 12-lead electrocardiogram.
Objective
To highlight the electrocardiographic feature of masquerading bundle branch block in a heart failure patient in our environment and the need for early recognition and close monitoring.
Patient and Methods
A 65-year-old man, known hypertensive and asthmatic, who presented with cough productive of whitish frothy sputum, bilateral leg swelling, and difficulty in breathing of 3 weeks duration. There was associated paroxysmal nocturnal dyspnea, orthopnea, and early satiety. No central chest pain on exertion or at rest.
Results
The 12-lead electrocardiography (ECG) showed precordial type MBBB with right bundle branch block in V1 and LBBB without deep and wide S waves in leads V5 and V6. Echocardiography confirmed heart failure with reduced ejection fraction of 19%, grade 3 diastolic dysfunction with E/A velocity ratio of 2.31, E/e’ of 29.7. Chest X-ray revealed unfolded aorta and cardiomegaly with cardio-thoracic ratio (CTR) of 65%. Patient was stabilized on anti-failure drugs and is being followed up.
Conclusion
We have reported electrocardiographic feature of MBBB in an African patient with heart failure. Early recognition of this rare electrocardiographic pattern, close monitoring and follow-up of these patients is important because of its association with poor prognosis.
Introduction
Masquerading bundle branch block (MBBB) is a rare but important finding on electrocardiogram.Citation1 It consists of right bundle branch block (RBBB) in precordial leads and left bundle branch block (LBBB) in limb leads.Citation2 It indicates advanced conduction system abnormality usually associated with severe underlying heart disease. MBBB is associated with poor prognosis.Citation1,Citation2 MBBB patients are at increased risk of complete atrioventricular (AV) block. To our knowledge, there is no previous published report of MBBB in heart failure in Nigeria. MBBB is classified into 2 types; the Standard and Precordial type.Citation3 The standard type is characterised by RBBB in precordial leads and LBBB pattern in limb leads without S wave in lead I. The precordial type is characterised by RBBB in right precordial leads and LBBB in left precordial leads without deep and wide S waves in leads V5, V6 and I. We report a case of heart failure with masquerading bundle branch block on 12-lead electrocardiogram.
Case Report
A 65-year-old retired civil servant and clergyman, who presented with cough productive of whitish frothy sputum, bilateral leg swelling, difficulty in breathing over 3 weeks prior to presentation. Difficulty in breathing was insidious in onset, initially on exertion, and progressed to become worse at rest, with paroxysmal nocturnal dyspnea (PND), orthopnea, easy fatigability and early satiety. No central chest pain on exertion or at rest.
Medical history shows he is a known hypertensive of 14 years, on follow-up at our cardiology outpatient clinic. He was first diagnosed with heart failure 3 years ago and this is his 2nd admission for heart failure, first was 3 months earlier. He does not take alcohol or smoke cigarette. He is not diabetic, and has not been diagnosed with myocardial infarction or angina in the past. No history of cytotoxic drug use or irradiation. He is on follow-up for benign prostatic hypertrophy at urology clinic, and he is also asthmatic. His routine medications were ramipril tablet, finasteride tablet and Seretide inhaler.
On Examination
He had bilateral pitting pedal edema. Weight was 52kg at admission. The pulse rate was 110 beats/minute, with thickened arterial wall, and extremities were not cold. The respiratory rate was 28 cycles per minute, oxygen saturation in room air was 93% (SPO2) and temperature was 37°C. The blood pressure was 90/60 mmHg with raised jugular venous pressure of 10 cmH2O and hyperdynamic precordium. Apex beat was at the sixth left intercostal space anterior axillary line (LICS AAL), heaving. The heart sounds were (HS) – 1, 2, 3, with apical pansystolic murmur. There were bibasal fine crepitations. The liver was enlarged 4cm below the right costal margin at mid-clavicular line, with a span of 14cm, tender and has a smooth surface. No splenomegaly
Investigation Results
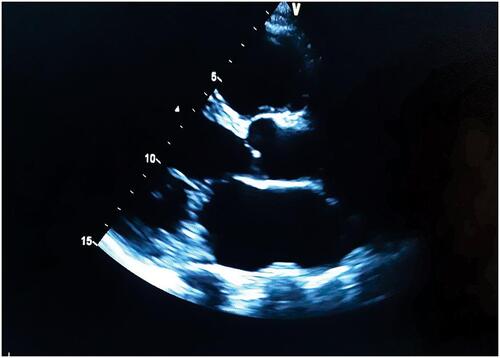
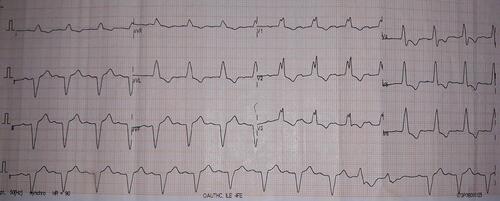
The 12-lead electrocardiogram revealed a sinus rhythm and rate of 93 bpm, with left axis deviation between −60° and −90°, 1st degree AV block with PR interval of 210ms, prolonged QRS duration of 148 ms and premature ventricular complex. Left ventricular hypertrophy (R in aVL >11mm). The right precordial leads revealed right bundle branch block, left precordial leads revealed LBBB and absence of deep and wide S waves in leads V5, V6 and I (precordial type MBBB) as shown in .
Figure 1 12 lead ECG showing MBBB precordial type. RBBB in right precordial leads, absent deep S waves in lead V5, V6 and I. LBBB in left precordial leads.
Chest X-ray revealed cardiomegaly with a cardio-thoracic ratio (CTR) of 185/285 (65%), unfolded aorta, cephalization and bilateral hilar fullness with associated peribronchial cuffing as shown in .
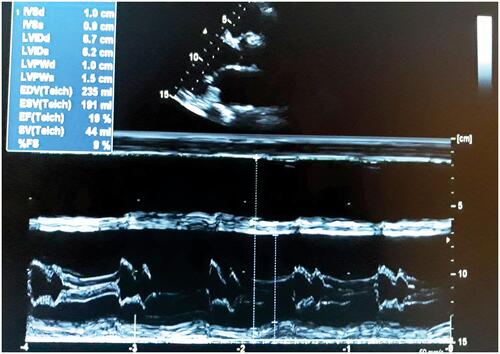
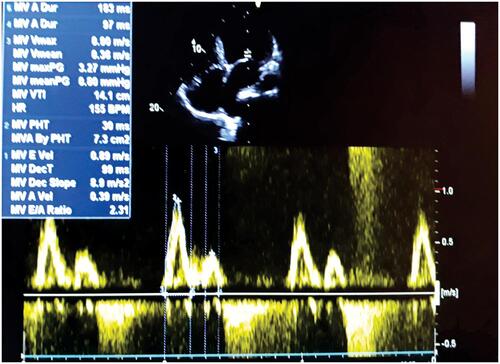
An echocardiogram as shown in – revealed enlarged left ventricle, severe left ventricular systolic dysfunction with ejection fraction of 19%, dilated left atrium, grade 3 diastolic dysfunction with E/A velocity ratio of 2.31, E/e’ of 29.7, and moderate mitral and tricuspid regurgitation. No regional wall motion abnormality. Coronary angiography could not be done.
Laboratory results revealed a packed cell volume (PCV) of 46%, and white blood cell count of 5600/mm3 with 60% segmented neutrophils and 40% lymphocytes. Film appearance was normal. Pre-renal azotemia with urea of 7.7mmol/l and hyponatremia with sodium of 133 mmol/l. Creatinine, potassium and bicarbonate were normal. Lipid profile parameters (total cholesterol, low-density lipoprotein, high-density lipoprotein and triglyceride) were all within normal range.
Figure 2 Posterior-anterior view of chest X-ray showing cardiomegaly with a CTR of 185/285 (65%), unfolded aorta, cephalization and bilateral hilar fullness with associated peribronchial cuffing.

The patient was diagnosed as having heart failure with reduced ejection fraction, in New York Heart Association (NYHA) functional class IV, accompanied by masquerading bundle branch block.
Treatment
He was commenced on both oral and intravenous anti-failure drugs, namely, intravenous lasix 60 mg, tablet bisoprolol 2.5mg, tablet aldactone 25 mg with daily weighing and monitoring of fluid input and output. Blood pressure could not tolerate ACE-I
He was discharged home in a stable condition 20 days after admission. At discharge, he was no longer dyspneic at rest, saturation in room air was 98%. Orthopnea, PND, cough and leg swelling had resolved. Weight was 48kg and he was in NYHA class II.
He was subsequently seen in clinic in stable condition (NYHA I). Patient is still on follow-up and close monitoring.
Discussion
The electrocardiographic pattern of right bundle branch block (RBBB) in precordial leads and left bundle branch block (LBBB) in limb leads was designated masquerading bundle branch block by Richman and Wolff,Citation4 because at that time they thought LBBB was masquerading as RBBB.
However, Unger et alCitation5 subjected 2 cases having features of MBBB on ECG to careful histologic study of the entire heart, including the conduction system, in each instance found bilateral bundle branch lesions (fibrosis) of considerable intensity, which did not completely disrupt the continuity of the branches and extensive destruction of the interventricular septum, the free walls of the left ventricle, and marked bilateral ventricular hypertrophy. They suggested MBBB pattern on electrocardiography signifies extensive myocardial damage, and with-it bilateral involvement of the bundle branches leading to partial bilateral bundle branch block. Lenègre also reported similar findings of severe damage in RBB and LBB in patients with MBBB pattern.Citation6
Tzogias et alCitation7 in their study of patients who developed RBBB from catheter induced trauma to the right bundle branch during right heart catheterization, having divided the patients into normal, left anterior or posterior fascicular block and left bundle branch block group based on their background ECG morphology. They reported that MBBB pattern (RBBB in lead V1 with absent S wave in leads I and aVL) was seen only among the group with background LBBB among the 3 groups, while the remaining groups developed the typical RBBB pattern. They concluded that an ECG pattern of RBBB in lead V1 with absent S wave in leads I and aVL indicates concomitant LBB delay.
Elizari et alCitation8 explained that MBBB is caused by the simultaneous presence of RBBB and a high-degree left anterior fascicular block (LAFB) often accompanied with severe left ventricular enlargement and/or fibrotic block in the anterolateral wall of the left ventricle. These conditions tend to re-orient the terminal electrical forces of the QRS complex towards the left and upwards, in such a way that the characteristic slurred S wave in lead I becomes smaller or even disappears. RBBB with LAFB may imitate LBBB either in the limb leads (standard masquerading) or in the precordial leads (precordial masquerading).Citation8 Cases of RBBB with LAFB in which the S wave is absent in lead I have been termed ‘standard masquerading’, and cases when the S wave disappears from V5 and V6 have been called “precordial masquerading”.Citation8 In both cases, RBBB can be recognized by the typical pattern in V1. According to Elizari et al,Citation8 this masquerading pattern can be explained very simply. The S wave in RBBB indicates the terminal forces oriented to the right produced by the delayed activation of the right ventricle. Conversely, the main LAFB forces are oriented superiorly and to the left; the higher the degree of LAFB, the smaller S1 will be. Moreover, if conduction is delayed in the anterolateral wall as a consequence of the factors already mentioned (e.g. fibrosis and focal block), the late forces originated within this area will balance or even prevail over the rightward forces of the RBBB. As a result of the close resemblance and similar ECG, clinical and pathological findings between “standard” and “precordial” types of masquerading RBBB, they should be considered variants of the same myocardial substrate.Citation8
Our patient’s ECG in this admission is consistent with the precordial type of MBBB, showing LBBB in limb leads, RBBB in right precordial leads and absent S wave in lead V5, V6 and I.
To our knowledge, there is no previous published report of MBBB in heart failure in Nigeria. However, several studiesCitation9–Citation12 have been published in Sub-Saharan Africa reporting various ECG patterns seen in heart failure, and some other cardiovascular disease.Citation13
Different heart diseases including hypertension, coronary artery disease, myocardial infarction, and cardiomyopathy have been associated with MBBB.Citation4–Citation6,Citation8,Citation14 In this case, patient is a known hypertensive of 14 years on medication, with displaced and heaving apex beat, aortic unfolding and cardiomegaly on X-ray, left ventricular hypertrophy on ECG. There were no symptoms suggestive of coronary artery disease now or in the past, no ST segment depression or ST segment elevation with reciprocals on ECG, no dyslipidaemia on lipid profile test, not diabetic, and does not smoke cigarette nor take alcohol. There was no regional wall motion abnormality on echo. However, a coronary angiography would have helped to further assess the possibility of ischaemic cardiomyopathy. No history of cytotoxic drug use. Patient made clinical improvement on treatment.
MBBB is usually associated with advanced heart disease and severe left ventricular dysfunction.Citation15 This patient has ventricular dilatation and severe left ventricular systolic dysfunction on echocardiography.
MBBB patients are at increased risk of complete atrioventricular (AV) block.Citation7,Citation8 They may require permanent pacemaker insertion.Citation7,Citation14 From a Brazilian registry, MBBB was associated with an estimated 4-year mortality and pacemaker insertion ratio of 41.4% and 38.9%, respectively.Citation16 MBBB sometimes present with syncope due to complete AV block necessitating pacemaker insertion.Citation7,Citation17 This patient already has a first-degree AV block, and requires close monitoring in case he develops a complete AV block requiring pacemaker insertion. Dhanse et alCitation1 reported a case of heart failure with reduced ejection fraction symptomatic over 3 months, with three vessel disease on coronary angiogram and masquerading bundle branch block on electrocardiogram whose condition deteriorated and died while on admission in the hospital awaiting coronary artery bypass grafting (CABG). Kaimoto et alCitation3 reported a case of a known hypertensive of 10 years who had heart failure with preserved ejection fraction and MBBB on ECG, who died suddenly 5 months after discharge. They further stated that the patient did not undergo electrophysiological study and the cause of her death was not elucidated, but opined that cardiac arrest due to complete heart block that developed from masquerading bundle branch block is the most likely cause.
Conclusion
We have reported electrocardiographic feature of MBBB in an African patient with heart failure. Early recognition of this rare electrocardiographic pattern, close monitoring and follow-up of these patients is important because of its association with poor prognosis.
Ethics Approval and Informed Consent
Ethical approval for this case report was obtained from the ethics and research committee of Obafemi Awolowo University Teaching Hospitals Complex (OAUTHC). A written informed consent was provided by the patient to have the case details and all accompanying images published.
Acknowledgment
This paper was presented at the July 2019 West African College of Physicians (WACP) (Nigeria chapter) Annual General and Scientific Meeting (AGSM) in Abeokuta (Page 61 of Abstract book).
Disclosure
The authors report no conflicts of interest in this work.
References
- Dhanse S, Kareem H, Devasia T, Sudhakar Rao M. Masquerading bundle branch block: a poor prognostic sign revisited. J Clin Diagn Res. 2016;10(9):OD01–OD02.
- Kocabaş U, Hasdemir C. A historical electrocardiographic finding: masquerading bundle branch block. Am J Cardiol. 2017;119(8):e29. doi:10.1016/j.amjcard.2017.03.105
- Kaimoto S, Kawasaki T, Taniguchi T, Kawasaki S, Kamitani T, Sugihara H. Masquerading bundle branch block as a marker of poor prognosis. J Cardiol Case. 2013;8(1):e57–e59. doi:10.1016/j.jccase.2013.04.005
- Richman JL, Wolff L. Left bundle branch block masquerading as right bundle branch block. Am Heart J. 1953;47(3):383–393.
- Unger PN, Lesser ME, Kugel VH, Lev M. The concept of “masquerading“ bundle-branch block an electrocardiographic-pathologic correlation. Circulation. 1958;17(3):XVII.
- Lenegre J. Etiology and pathology of bilateral bundle branch block in relation to complete heart block. Prog Cardiovasc Dis. 1964;6(5):409–444. doi:10.1016/S0033-0620(64)80001-3
- Tzogias L, Steinberg LA, Williams AJ, et al. Electrocardiographic features and prevalence of bilateral bundle-branch delay. Circ Arrhythmia Electrophysiol. 2014;7(4):640–644. doi:10.1161/CIRCEP.113.000999
- Elizari MV, Baranchuk A, Chiale PA. Masquerading bundle branch block: a variety of right bundle branch block with left anterior fascicular block. Expert Rev Cardiovasc Ther. 2013;11(1):69–75. doi:10.1586/erc.12.142
- Karaye KM, Sani MU. Electrocardiographic abnormalities in patients with heart failure. Cardiovasc J Afr. 2008;19(1):22–25.
- Omotoso A, Opadijo O, Araoye M. Intraventricular conduction blocks in adult Nigerians with hypertensive heart disease. Trop Cardiol. 1999;25:75–79.
- Dzudie A, Milo O, Edwards C, et al. Prognostic significance of ECG abnormalities for mortality risk in acute heart failure: insight from the Sub-Saharan Africa survey of heart failure (THESUS-HF). J Card Fail. 2014;20(1):45–52. doi:10.1016/j.cardfail.2013.11.005
- Kofi Owusu I. Electrocardiographic abnormalities in heart failure patients at a teaching hospital in Kumasi, Ghana. J Cardiovasc Dis Diagn. 2014;02(02):2–4. doi:10.4172/2329-9517.1000142
- Adebayo RA, Ikwu AN, Balogun MO, et al. Heart rate variability and arrhythmic patterns of 24-hour holter electrocardiography among Nigerians with cardiovascular diseases. Vasc Health Risk Manag. 2015;11:353–359. doi:10.2147/VHRM
- Choudhary D, Namboodiri N, Tharakan JA. A case of “masquerading” bundle branch block: a forgotten concept. Indian Heart J. 2014;66(1):139–140. doi:10.1016/j.ihj.2013.12.025
- Daubert C, Mabo P. Bilateral bundle branch block, an old concept revisited in the light of cardiac resynchronization therapy. Heart Rhythm. 2016;13(12):2297–2298. doi:10.1016/j.hrthm.2016.08.009
- Souza TGS, Almeida RL, Targueta GP, et al. Masquerading bundle branch block: an electrocardiographic marker of poor prognosis. Circulation. 2015;132(suppl_3):A14845.
- Jiao Z, Tian Y, Yang X, Liu X. Masquerading bundle branch block as a presenting manifestation of complete atrioventricular block that caused syncope. J Int Med Res. 2017;45(5):1597–1601. doi:10.1177/0300060517708694