Abstract
A 74-year-old man with coronary artery disease was suffering from acute nonobstructive cholecystitis and was admitted to a nearby hospital. Dual antiplatelet (aspirin and ticlopidine) therapy was discontinued before preparation for surgical resection of the gall bladder. During his time in hospital he was aware of lumbar pain and weakness in both legs. He was transferred to our hospital for further evaluation and therapy. Diffuse intra-aortic thrombi were revealed by computed tomography with contrast media, and magnetic resonance imaging showed spinal cord infarction. However, computed tomography scans of the descending aorta obtained 4 months before admission exhibited no signs of atherosclerotic plaques or intra-aortic thrombi. Laboratory data suggest that antiphospholipid antibody syndrome might have caused these acute multiple intra-arterial thrombi. By restarting dual antiplatelet therapy and increasing the dose of heparin (from 10,000 IU/day to 15,000 IU/day) we successfully managed the patient’s clinical condition and symptoms. It is important to understand that stopping antiplatelet therapy may rapidly grow thrombi in patients with a hypercoagulative state.
Introduction
Spinal cord infarction is a relatively rare condition and is caused by occlusion of the Adamkiewicz artery. This is caused by conditions such as aortic dissection, atherosclerosis in the aorta, significant hypotension, and/or unexpected mechanical occlusion of spinal circulation after abdominal surgery.Citation1–Citation4 Antiphospholipid antibody syndrome (APS) is a rare condition. Patients with this syndrome can present with both intravenous and intra-aortic thrombi; however, intra-aortic thrombi seldom progress in a manner similar to atherosclerosis. Intra-aortic thrombi have no symptoms unless embolic events occur and are detected by evaluation for embolic source by thoracic computed tomography (CT) or transesophageal echocardiography. Most of them are related to arteriosclerosis.
Case report
A 74-year-old Japanese man visited a nearby hospital because of pain in the right hypochondrium. Abdominal ultrasonography and blood chemistry led to the diagnosis of acute cholecystitis. He was admitted to the hospital and deprived of food, and antibiotics were given intravenously. His condition necessitated surgery; thus, antiplatelet therapy (aspirin and ticlopidine), which had been administered after percutaneous coronary intervention of the angina pectoris with bare metal stent 3 years previously, was discontinued. According to the Japanese guideline, cholecystectomy is considered to be a medium-risk procedure. Heparin was not started when dual antiplatelet therapy was stopped.Citation5
On the fourth day of admission to the hospital, a CT scan of the patient’s abdomen revealed the following findings. First, no stone was found in the gall bladder; thus, his condition was an acute nonobstructive cholecystitis. Second, several diffuse and multiple contrast lucent masses were present in the descending aorta, which appeared to be atherosclerotic plaques. However, CT scans of descending aorta obtained 4 months before his admission exhibited no signs of contrast lucent masses such as atherosclerotic plaques. Previous CT examination was evaluated for syncope and chest and back pain to rule out aortic dissection. Furthermore, blood chemistry data, which exhibited a high level of fibrin degradation product (FDP) and D-dimer, suggested that these masses were multiple thrombi in an acute phase. Then, unfractionated heparin was administrated. On the sixth day the patient complained of lumbar pain and weakness of both legs. Therefore, he was transferred to our hospital for further study and therapy.
On admission he was unable to sit or stand by himself. Other vital signs were unremarkable. Neurological examination revealed weakness of the lower extremities (Iliopsoas Grade 3, knee extension Grade 4, and upper arm Grade 5 [normal], according to American Spinal Injury Association classification).
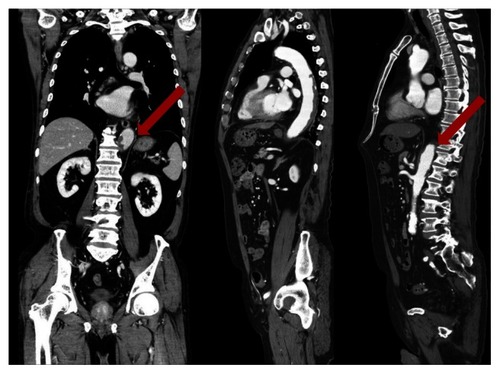
There was also sensory disturbance under the level of the tenth thoracic vertebra (Th10). Emergency dynamic thoracoabdominal contrast-enhanced CT revealed a slight progression of the intra-aortic thrombi and occlusion of the anterior spinal cord artery at the diaphragmatic level, compared with the previous reading at his former hospital ( and ). Therefore, we suspected that he had a spinal cord infarction. We administrated antiplatelet therapy (aspirin and ticlopidine) immediately and increased the dose of unfractionated heparin from 10,000 IU/day to 15,000 IU/day to achieve an activated partial thromboplastin time of 49.2 seconds (control 29.9 seconds, 1.65 times prolonged). After this treatment, his neurological symptoms did not progress. On the second day of admission to our hospital, percutaneous transhepatic gall bladder drainage (PTGBD) was performed. FDP and D-dimer values decreased on the next day of PTGBD, and we continued the antiplatelet treatment.
Figure 1 These images show abdominal computed tomography scans obtained at three different timings. Both upper and lower computed tomography images are of the same lesion in the descending aorta. Despite the high flow in his arteries, his intra-aortic thrombi rapidly expanded. After 2 weeks of anticoagulation, his thrombi reduced in size.
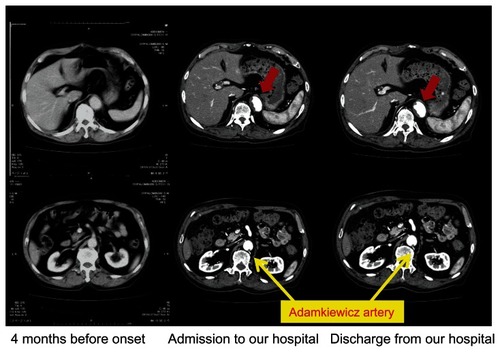
Figure 2 These images show abdominal computed tomography scans of longitudinal views at admission to our hospital.
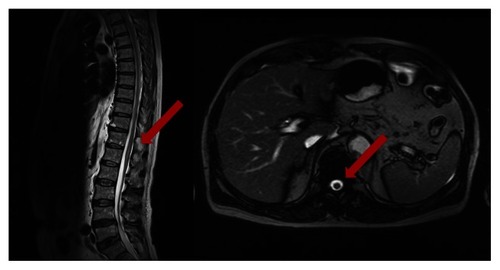
On the third day, magnetic resonance imaging of the spinal cord revealed high intensity in the spinal cord from Th9 to the first lumbar vertebra (L1) on a diffusion-weighted image, as well as a T2-weighted image. Magnetic resonance images supported the diagnosis of spinal cord infarction caused by anterior spinal artery occlusion (). Heparin and antiplatelet medications were continued, and his laboratory data (FDP and D-dimer) improved stably; therefore, additional anticoagulant therapy was deemed unnecessary. Paralysis of both legs and the senses near the anus and the incomplete passage of stool improved gradually. On the tenth day he could stand up with a little support. Twenty days after PTGBD, follow-up CT revealed regression of the intra-aortic thrombi. Finally, he moved back to his former hospital to continue rehabilitation.
Discussion
Spinal cord infarction is a rare condition, and systematic reviews on this condition are few.Citation1 Nearly two-thirds of spinal cord infarctions are caused by acute or chronic spinal disease.Citation6 Aortic dissection is one of the major causes of this condition; however, the absolute number of patients with spinal cord infarction is low. Aortic dissection rarely obstructs the Adamkiewicz artery resulting in spinal cord infarction. In many cases, etiologies are not identified. We were able to diagnose our patient as having early-phase spinal cord infarction due to arterial thrombi by the findings of previous and present CT images, laboratory data, and neurological examinations.
Previous studies have suggested that most lucent masses in the aorta observed by CT evaluation are atherosclerosis that has usually existed for a long period of time. Thrombi rarely grow in high-flow areas such as in the arterial system. However, we observed a case of rapidly progressive multiple thrombi in the descending aorta resulting in spinal cord infarction. We made two important observations. First, it was difficult to identify the contrast lucent masses in the patient’s aorta as thrombi. They exhibited a similar appearance to atherosclerosis, and many physicians were unable to distinguish these masses. Only with the contrast-enhanced CT images obtained 4 months before could we diagnose thrombi in our case. If diagnosis had been delayed, the patient might have been rendered completely paraplegic. Second, identifying the cause of thrombosis was difficult. Many previous studies have suggested that arterial thrombi are caused by many factors, including infection, blood coagulation abnormality, APS, and malignancy. Infections such as cholecystitis or other infections with sepsis usually do not generate multiple thrombi in the aorta. The patient’s thoracoabdominal CT did not reveal malignant tumors; however, laboratory data upon admission to our hospital revealed APS, because his anticardiolipin antibody was positive. In this case, definitive diagnosis was confirmed with a positive value of anticardiolipin antibody after 6 months. APS is known to be a leading cause of both arterial and venous thrombosis. However, patients with this syndrome do not usually develop diffuse and severe intra-aortic thrombi, except in a few case reports of myocardial infarctions and strokes.Citation7,Citation8 We speculate that the sudden stopping of antiplatelet therapy might have caused arterial thrombi in this case.
Our patient was treated with warfarin and dual antiplatelets and had no complication of hemorrhage. Following continuous rehabilitation he was able to stand up by himself with a holding rail. Thus, we were able to successfully treat spinal cord infarction caused by rapidly progressive diffuse intra-aortic thrombus in a patient with acute nonobstructive cholecystitis.
Conclusion
We successfully managed aortic thrombi resulting in spinal cord infarction associated with APS in a patient with acute cholecystitis. APS should be taken into consideration if systemic thrombi are observed for unexplained reasons.
Disclosure
No conflicts of interest exist.
References
- ClouseWDHallettJWJrSchaffHVAcute aortic dissection: population-based incidence compared with degenerative aortic aneurysm ruptureMayo Clin Proc20047917618014959911
- WangCMTsaiWLLoYLChenJYWongAMUnilateral right occipital condyle to C2 level spinal cord infarction associated with ipsilateral vertebral artery stenosis and contralateral vertebral artery dissection: a case reportJ Spinal Cord Med201134111812121528635
- FairheadJFPhillipsDHandaAEmbolic spinal cord infarction as a presentation of abdominal aortic aneurysmJ R Soc Med2005982596015684355
- HarlanderMBajroviäFFBlincASabovicMMonoparesis due to spinal cord infarction associated with thoracoabdominal aneurysmHeart Vessels200823535936218810586
- JSC Joint Working GroupGuidelines for preoperative cardiovascular evaluation and management for noncardiac surgery (JCS2008)Circ J201175989108921427501
- KumralEPolatFGüllüogluHUzunköprüCTuncelRAlpaydinSSpinal ischaemic stroke: clinical and radiological findings and short-term outcomeEur J Neurol20111823223920402756
- HasegawaMYamashitaJYamashimaTIkedaKFujishimaYYamazakiMSpinal cord infarction associated with primary antiphospholipid syndrome in a young child. Case reportJ Neurosurg1993794464508360745
- OhtomoYMatsubaraTNishizawaKUnnoAMotohashiTYamashiroYNephropathy and hypertension as manifestations in a 13-y-old girl with primary antiphospholipid syndromeActa Paediatrica1998879039079736241