Abstract
We present a series of four patients who had been admitted to two hospitals in Addis Ababa after presenting with persistent and chronic diarrhoea. All patients were subsequently diagnosed to have Clostridioides difficile-associated pseudomembranous colitis, a disease that has long been regarded as a rare diagnosis in sub-Saharan Africa, and which has not yet been reported in Ethiopia. This case series is believed to create a much-needed awareness among physicians on the existence of this treatable but potentially fatal disease.
Introduction
Clostridioides difficile infection (CDI) is a disease mainly associated with the use of antibiotics.Citation1 Not all patients develop symptoms after colonization, but in those with symptoms, the disease can vary from mild diarrhoea to life-threatening colitis. Rare manifestations of CDI like bacteraemia and peritonitis have also been reported.Citation2,Citation3 Colonization of the intestinal tract follows exposure through feco-oral route and disease develops from the subsequent alteration of the normal intestinal flora.
According to the Centre for Disease Control and Prevention (CDC), C. difficile infection is among the top public health threats associated with the use of antimicrobial agents.Citation4 In the United States (US) alone, CDI resulted in 500,000 infections and 29,000 deaths in 2011.Citation1 The annual health care-associated cost of CDI in the US is reported to be over $4 billion.Citation5
Recent observations have shown an increase in the incidence of community-acquired CDI resulting in disease in patients who were in the past thought to be at low risk.Citation6
Antibiotic use is the most common risk factor for CDI. Other factors associated with increased risk of the disease include recent hospitalization, old age, gastric acid suppression, gastrointestinal surgery, chemotherapy and hematopoietic stem cell transplantation.Citation7,Citation8
The diagnosis of CDI depends on clinical and laboratory findings. Infectious Diseases Society of America (IDSA) guidelines recommend making the diagnosis of CDI when the following criteria are met:
symptoms of diarrhoea, defined as 3 or more loose stools in 24 hours and
a stool test positive for C. difficile or its toxins, or colonoscopy or pathology findings consistent with pseudomembranous colitis.Citation9,Citation10
Management of CDI includes; prompt discontinuation of offending drugs, supportive care and use of antibiotics including metronidazole and oral vancomycin.Citation11
Case 1
A 67-year-old male patient from Dire Dawa, who gave a history of repeated intake of different oral antibiotics (ciprofloxacin, trimethoprim–sulfamethoxazole and tinidazole) for a presumed gastrointestinal and urinary tract infections (UTI) in the prior 3 months, presented with diarrhoea, abdominal pain and fever of 4 weeks duration.
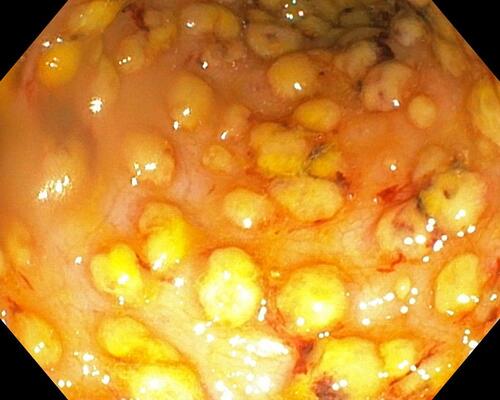
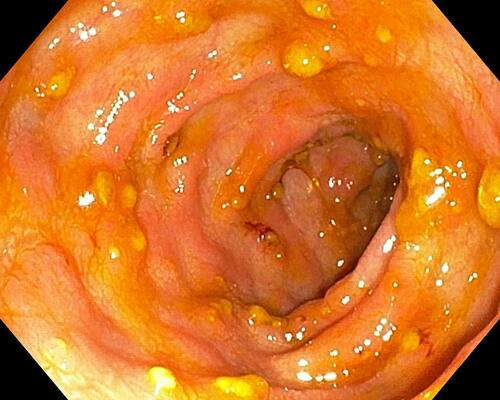
The patient was febrile and tachycardic on presentation and investigations revealed a white cell count of 36,000 cells/mm3 (N= 95%) with a Hgb of 8.9 gm./dl. BUN was 74.58 mg/dl and his creatinine was 4.8 mg/dl. Limited colonoscopy revealed extensive mucosal oedema and erythema with pseudomembranes in the rectum and sigmoid colon suggesting possible Clostridioides difficile-associated pseudomembranous colitis ().
The colonic biopsy subsequently revealed chronic active colitis most likely pseudomembranous colitis and stool Clostridioides difficile DNA real-time PCR turned out to be positive.
With the above evidences, the patient was started on oral vancomycin, IV metronidazole and supportive care and he demonstrated marked improvement with the disappearance of fever and diarrhoea. He was subsequently discharged from hospital after 1 week of stay.
Case 2
A 70-year-old male patient with longstanding Type 2 diabetes mellitus (DM), hypertension, and end-stage renal disease, who was on oral cefuroxime and norfloxacin for 5 days for a presumed UTI, presented with fever and diarrhoea of 3 weeks duration. The patient was seen at a local clinic for the diarrhoea and after stool examination, he was put on IV ceftriaxone for five more days. But his symptoms persisted despite the change in antibiotics.
His physical examination was remarkable for tachycardia and lower abdominal tenderness. Investigations revealed neutrophil predominant leucocytosis and many PMN cells with few RBCs were seen on stool microscopy. An abdominal ultrasound showed left-sided colonic wall thickening and subsequent sigmoidoscopy revealed diffuse mucosal erythema with numerous patchy exudates suggestive of pseudomembranes ( and ).
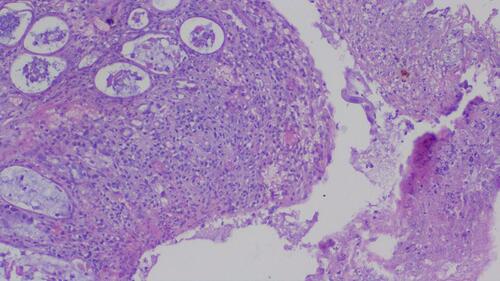
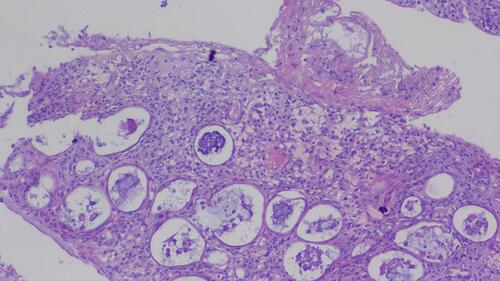
Biopsy from the colon revealed mucosal tissue fragments that had explosive necro-inflammatory pseudomembranous exudate on the surface of ulcerated mucosal fragments. Variably dilated crypts partly filled with mucus and neutrophils, with superficial epithelial loss and variably expanded lamina propria were also seen ().
Stool C. difficile toxin assay was planned but the patient could not afford the test. So, with a presumptive diagnosis of pseudomembranous colitis, he was put on oral vancomycin and he was discharged from hospital after 7 days of treatment with complete resolution of the diarrhoea.
Case 3
A 73-year-old male who had prostatectomy 7 weeks back and who was on ceftriaxone IV post-operatively developed frequent watery diarrhoea on the 6th post-operative day, which persisted for 6 weeks. Physical examination revealed an acutely sick patient with a fever of 38°C and the patient had a protuberant abdomen with mild generalized abdominal tenderness.
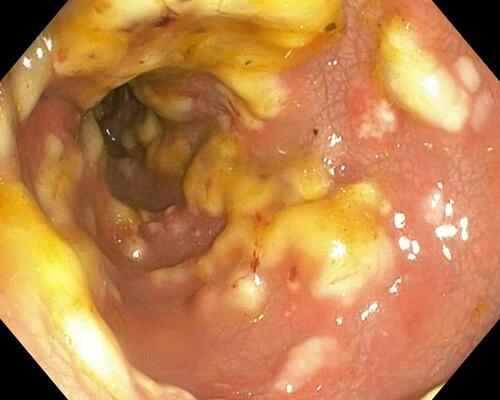
Investigation showed a WBC count of 26,800 cells/mm3 (neutrophils 83%), with normal Hgb and organ function tests. Given the abdominal tenderness, peritonitis was suspected. Abdominal CT subsequently revealed colonic and rectal wall thickening with minimal peritoneal fluid collection. So, urgent colonoscopy was performed and it revealed extensive mucosal oedema and erythema with overlying patchy exudates in the rectum and sigmoid, consistent with pseudomembranous colitis ().
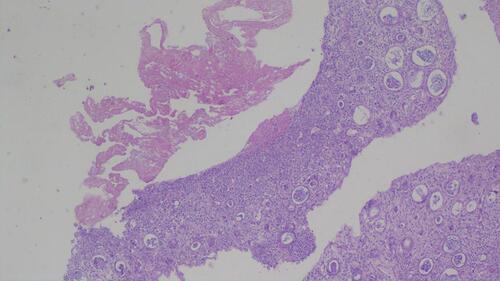
Colonic mucosal biopsy revealed mucosal fragments with expanded lamina propria and marked lympho-polymorphonuclear infiltrates associated with variably dilated crypts filled with mucus and neutrophils. In addition, surface ulceration with necro-inflammatory pseudomembranous exudate mixed with mucus was seen and these histo-pathological findings were suggestive of pseudomembranous colitis ( and ).
Given the patients’ financial constraints, stool CDI toxin assay could not be performed. So, he was admitted and started on oral vancomycin, IV metronidazole and supportive care. He showed marked improvement and he was discharged from hospital after 8 days of stay.
Case 4
A 25-year-old male patient with acute myeloid leukaemia (AML), who recently completed chemotherapy and who was on cefepime, meropenem and ciprofloxacin for neutropenic fever, developed non-bloody diarrhoea, fever and abdominal pain of 15 days duration.
Physical examination was remarkable for fever of 38–39°C, tachycardia, and lower abdominal tenderness.
Investigation revealed WBC count of 400 cells/mm3 with an absolute neutrophil count being 60 cells/mm3, a haemoglobin of 9 g/dl, and a platelet count of 14,000/microliter.
Stool microscopy showed many PMN cells but the patient’s renal and liver function tests were normal.
Abdominal CT scan showed diffuse large bowel wall thickening suggesting possible infectious pan-colitis (). Subsequent sigmoidoscopy revealed diffuse mucosal erythema with pseudomembranes ().
Determining stool Clostridioides difficile toxin assay was not possible due to financial reasons. So, the patient was given oral vancomycin and his symptoms completely subsided.
Discussion
The clinical cases presented above demonstrate that CDI can affect a variety of patient populations with different comorbidities (). Although most of the patients in this series were aged 67 years and above, younger patients can also be affected by the disease (as was the case in the last patient). In addition to age, the presence of comorbidities like end-stage kidney disease, diabetes, hematologic malignancy and chemotherapy may have contributed to the risk of developing CDI.Citation7,Citation8
Table 1 Summary of the Cases
Antibiotic exposure is a major risk factor for the development of pseudomembranous colitis and numerous groups of antibiotics including cephalosporins, penicillin, fluoroquinolones, clindamycin, macrolides, folic acid inhibitors and tetracyclines have been implicated in the development of CDI.Citation4
The above described four patients have been exposed to multiple antibiotics including ceftriaxone, cefuroxime, ciprofloxacin, norfloxacin, co-trimoxazole, carbapenems and tinidazole and most of them actually took multiple antibiotics which were prescribed empirically. Lack of proper microbiology laboratory facility often results in uncertain etiologic diagnosis of infectious diseases, thereby resulting in empiric therapy using multiple antibiotics, which increases the risk of developing pseudomembranous colitis.
Although there are many epidemiologic studies in Europe, America and Asia, the prevalence of CDI in Sub-Saharan African countries is largely unknown. In fact, no single study or case report is available in the literature on CDI in Ethiopia.
Given the lack of strong antibiotic stewardship in most of our hospitals and the wide use of empiric antibiotic therapy in Ethiopia, it is fair to assume that we actually have the disease in our setups and the identification of these cases should alert the medical community on the need for improving the rational use of antibiotics.
The diagnosis of CDI was made after a significant delay in all the above-reported cases and most of the diagnosis was made indirectly using a combination of clinical evidence, imaging and colonoscopy findings, and histopathology.
Though a variety of disorders including infection with other enteric pathogens, drugs, intra-abdominal sepsis, ischemic colitis and idiopathic inflammatory bowel disease can have similar manifestations as CDI, the prompt response to discontinuation of offending antibiotics and initiation of oral vancomycin seen in all of the reported patients strongly supports the diagnosis.Citation12
The lack of diagnostic tests like stool toxin assays in most facilities in Ethiopia is believed to contribute to the delay in diagnosis and efforts need to be put forward to improve access to these important tests.
By presenting this case series, we hope to create awareness among clinicians and the public health community on the existence of this treatable but potentially life-threatening disease and we recommend further studies to investigate the incidence, prevalence, risk factors, management and possible outcomes of the disease in hospitals in Ethiopia.
Ethical Approval
According to the Institutional Review Board guidelines of Addis Ababa University, a case series does not necessarily require IRB submission and ethical approval for publication, as long as the necessary informed consent is acquired from all the involved subjects and as long as the study complies with the Declaration of Helsinki, criteria which are both fulfilled by this case series. But if documentation of exemption from IRB is required, we are willing to request the IRB board and provide one.
Consent
Written informed consent was obtained from all four patients for publication of this case series and accompanying images. All the investigations performed for all patients were done as part of their clinical care and all were done with full approval by the patients. All four patients also gave consent for the use of all their investigation results in this case series.
Disclosure
The authors report no conflicts of interest in this work.
References
- Lessa FC, Mu Y, Bamberg WM, et al. Burden of Clostridium difficile infection in the United States. N Engl J Med. 2015;372(9):825–834.
- Antibiotic resistance threats in the United States. Centers for Disease Control; 2013 [cited September 9, 2018]. Available from: https://www.cdc.gov/drugresistance/threat-report-2013/index.html. Accessed September 2, 2020
- Dubberke ER, Olsen MA. Burden of Clostridium difficile on the healthcare system. Clin Infect Dis. 2012;55(Suppl 2):S88–S92. doi:10.1093/cid/cis335
- Chitnis AS, Holzbauer SM, Belflower RM, et al. Epidemiology of community-associated Clostridium difficile infection, 2009 through 2011. JAMA Intern Med. 2013;173(14):1359–1367. doi:10.1001/jamainternmed.2013.7056
- Leffler DA, Lamont JT. Clostridium difficile infection. N Engl J Med. 2015;373(3):287–288.
- Barbut F, Corthier G, Charpak Y. Prevalence and pathogenicity of Clostridium difficile in hospitalized patients: a French multicenter study. Arch Intern Med. 1996;156:1449–1454. doi:10.1001/archinte.1996.00440120107012
- Johnson S, Gerding DN. Clostridium difficile-associated diarrhea. Clin Infect Dis. 1998;26:1027–1036. doi:10.1086/520276
- Bartlett JG. Clinical practice. Antibiotic-associated diarrhea. N Engl J Med. 2002;346:334–339. doi:10.1056/NEJMcp011603
- Kelly CP, Pothoulakis C, LaMonte JT. Clostridium difficile colitis. N Engl J Med. 1994;330:257–262. doi:10.1056/NEJM199401273300406
- Bartlett JG. Narrative review: the new epidemic of Clostridium difficile-associated enteric disease. Ann Intern Med. 2006;145:758.
- Sartelli M, Di Bella S, McFarland LV, et al. 2019 update of the WSES guidelines for management of Clostridioides (Clostridium) difficile infection in surgical patients. World J Emerg Surg. 2019;14(8).
- Bartlett JG, Gerding DN. Clinical recognition and diagnosis of Clostridium difficile infection. Clin Infect Dis. 2008;46(Supplement_1):S12–S18. doi:10.1086/521863