Abstract
We are reporting a case of a 22-year-old lady with bilateral microphthalmia and microcornea, in which a modified technique for sutureless scleral fixated intraocular lens implantation provided a successful aphakic rehabilitation alternative with a good visual outcome and significant improvement in quality of life. Management of aphakia in microphthalmic eyes is challenging due to the anatomical abnormalities and limited literature on managing such cases. Visual rehabilitation for aphakia using contact lenses is limited by intolerance and poor lens fitting. Significant optical aberrations may limit aphakic spectacle use, further exacerbated in patients with nystagmus. Thus, secondary IOL implantation seems to be a reasonable rehabilitation alternative; however, it is surgically challenging in microphthalmic eyes.
Introduction
Microphthalmos is a developmental anomaly consisting of a smaller than normal eye, which can be isolated or associated with other ocular abnormalities such as congenital cataracts and nystagmus.Citation1
Management of cataract and aphakia in microphthalmic eyes represents a challenging task due to the anatomical abnormalities and limited resources in the literature on managing such cases.Citation1 Aphakic spectacles are limited by significant optical aberrations, which are further exacerbated in patients with nystagmus.Citation1 Thus, secondary IOL (intraocular lens) implantation seems to be a reasonable rehabilitation alternative; however, it is surgically challenging in microphthalmic eyes.Citation1
Here, we report a 22-year-old lady with bilateral microphthalmia and microcornea, in which secondary IOL implantation using sutureless scleral fixation technique with modification provided good visual outcome and patient’s satisfaction.
Case Report
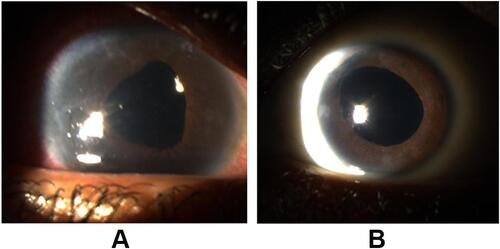
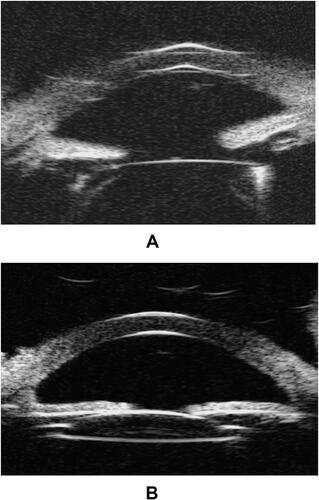
We are presenting a 22-year-old lady, with isolated bilateral microphthalmia and microcornea, associated with nystagmus and bilateral congenital cataract, for which she had undergone lensectomy at the age of two years, with resulting bilateral aphakia and secondary medically controlled glaucoma. The patient presented to our clinic seeking refractive correction, as she was dissatisfied with her thick aphakic glasses. She was intolerant to contact lenses as well, owing to her nystagmus and poor lens fitting.
Preoperatively, visual acuity, refraction, tonometry, slit-lamp biomicroscopy, dilated fundus exam, and brightness scan ultrasonography were performed. Biometry measurements using HofferQ formula were also obtained. The patient achieved a preoperative best-corrected visual acuity of 20/40 and 20/50 in the right and left eye, respectively. Her spectacle prescription was +17.00 −1.00 × 170 in the right eye and +16 −1.00 × 180 in the left eye, with an additional power of +2.00D in both eyes. Her ophthalmic exam was significant for nystagmus, small eye, aphakia, and optic disc drusen bilaterally. Axial length measured 19.56 mm and 19.03 mm in the right and left eye, respectively. Her corneal diameter measured 9.9 mm and 9.7 mm, respectively. The decision to undergo secondary IOL implantation was made, and monofocal, acrylic 3-piece IOLs were chosen. The lens has an optic diameter of 6.0 mm, a haptic–haptic diameter of 13 mm and a power of +30.0D and +29.0D, in the right and left eye, respectively.
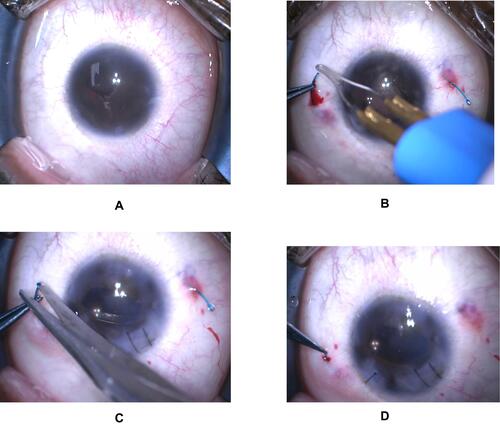
Using the Yamane technique (), a scleral fixated IOL was implanted in the right eye. A temporal corneal incision and paracentesis were created 90 degrees apart, and anterior vitrectomy was performed. The IOL was injected into the AC (anterior chamber). Two wide-lumen 30-gauge needles were inserted 180 degrees apart, 2 mm from the limbus at 12 and 6 o’clock positions. The haptics were introduced inside the lumen of both needles and externalized through the scleral tunnels. Cautery was applied to secure the haptics (). Peripheral iridotomy was performed. Two milliliters of each haptic were trimmed (), and cautery was used again to form a button-like tip at the end of each haptic. The haptics were placed in the scleral tunnel using gentle manipulation (), and centration of the IOL was achieved.
Figure 1 (A) scleral fixation using Yamane technique, (B) securing the haptics with cautery, (C) haptics trimming, (D) placing haptics in the scleral tunnel.
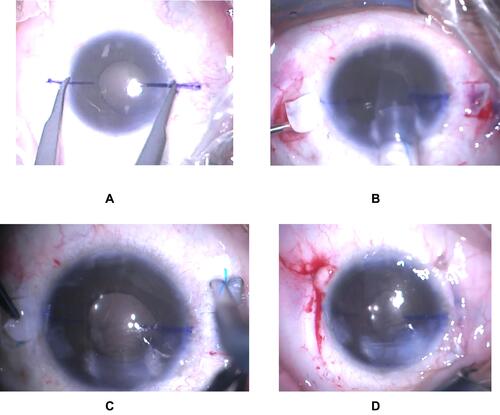
A few months after the initial surgery, a glued scleral fixated IOL was implanted in the left eye (), where two scleral flaps were created 180 degrees apart, and the AC was entered through the flap, using a supersharp blade. A temporal corneal incision was created, anterior vitrectomy was performed, and an AC maintainer was inserted. The IOL was introduced into the sulcus. Using retinal forceps, haptics were grasped and externalized under scleral flaps (). Trimmed haptics were tucked into the scleral tunnels made at the point of haptic externalization (), and scleral flaps and conjunctiva were closed using fibrin glue ().
Figure 2 (A) scleral fixation using fibrin glue, (B) introducing IOL into the sulcus and externalizing the haptics through the flap, (C) haptics trimming, (D) scleral flaps and conjunctiva closed using fibrin glue.
One year postoperatively ( and ), the patient achieved uncorrected visual acuity of 20/30 in the right eye and 20/40 in the left eye. The patient was satisfied with the results and reported subjective improvement in her vision and quality of life.
Discussion
The International Clearinghouse for Birth Defects Monitoring Systems defined anophthalmia and microphthalmia as “apparently absent or small eyes”.Citation2 The term microphthalmia can be used to describe eyes with axial length two standard deviations below the age-adjusted mean, which is less than 21 mm in adult eyes.Citation3 Microphthalmic eyes have a corneal diameter of less than 10 mm.2
Simple microphthalmia refers to a small eye that is structurally normal,Citation3 while in complex microphthalmia, associated anterior or posterior segment abnormalities or both are present.Citation3 These may include sclerocornea, Peters anomaly, persistent primary vitreous, or retinal dysplasia.Citation3 Other ocular abnormalities such as congenital cataract and nystagmus may be present, as well.Citation1
Patient’s intolerance and poor fitting may limit the use of contact lenses for aphakic rehabilitation in microphthalmic eyes.Citation1 Furthermore, aphakic spectacles are limited by significant optical aberrations, especially in the presence of nystagmus,Citation1 while surgically challenging, secondary IOL appears to be a reasonable alternative.Citation1
Options for secondary IOL such as AC IOL, in the bag placement with or without capsular tension devices, or ciliary sulcus IOL in these small eyes are limited by insufficient capsular support, limited AC depth and volume, and white-to-white measurements.Citation4 Sutured scleral fixation carries a risk of pseudophakodonesis, which may lead to retinal detachment (4.9%) and chronic macular edema (7.3%).Citation5 Furthermore, in cases of microphthalmos, IOL power should be calculated preoperatively using theoretical and empirical IOL formulas, as postoperative refraction shows a hypermetropic tendency compared with the predicted refraction, which can be attributed to the short axial length in microphthalmic eyes.Citation6
Kumar et al conducted a prospective case series to evaluate intraoperative modifications and visual outcomes following glued IOL implantation in 15 eyes with microcornea and concluded that glued IOL using modifications such as custom haptic trimming and 6 mm optic foldable IOLs are safe to implant in eyes with microcornea.Citation7
However, in eyes with microphthalmos, scarce cases were reported in the literature concerning sutureless scleral fixation for secondary IOL implantation as an option for aphakic correction in adults’ microphthalmic eyes with absent capsular support.
In this case, we report a 22-year-old lady with bilateral microphthalmia and microcornea, in which secondary IOL implantation provided a successful visual rehabilitation alternative for high hyperopia. Two different sutureless techniques with modification for scleral fixation were used for secondary IOL implantation in each eye, namely, Yamane technique and glued scleral fixation. Our patient showed a good visual outcome and significant improvement in her quality of life.
Abbreviations
IOL, intraocular lens; AC, anterior chamber.
Ethical Approval and Consent to Participate
No institutional approval was required to publish this case. The patient provided an informed written consent for this case to be published for educational and research purposes.
Disclosure
The authors report no conflicts of interest in this work.
References
- Sinskey R, Amin P, Stoppel J. Intraocular lens implantation in microphthalmic patients. J Cataract Refract Surg. 1992;18(5):480–484. doi:10.1016/s0886-3350(13)80102-2
- Tyl RW, Friedman MA, Schrader TJ, et al. International clearinghouse for birth defects monitoring systems, national birth defects prevention network, collaborative meeting, Friday, September 20, 2002, Atlanta, GA. Reprod Toxicol. 2003;17(1):117–136. doi:10.1016/s0890-6238(02)00096-5
- Morrison D. National study of microphthalmia, anophthalmia, and coloboma (MAC) in Scotland: investigation of genetic aetiology. J Med Genet. 2002;39(1):16–22. doi:10.1136/jmg.39.1.16
- Scharioth G, Prasad S, Georgalas I, Tataru C, Pavlidis M. Intermediate results of sutureless intrascleral posterior chamber intraocular lens fixation. J Cataract Refract Surg. 2010;36(2):254–259. doi:10.1016/j.jcrs.2009.09.024
- McAllister A, Hirst L. Visual outcomes and complications of scleral-fixated posterior chamber intraocular lenses. J Cataract Refract Surg. 2011;37(7):1263–1269. doi:10.1016/j.jcrs.2011.02.023
- Inatomi M, Ishii K, Koide R, Kora Y, Ozawa T. Intraocular lens power calculation for microphthalmos. J Cataract Refract Surg. 1997;23(8):1208–1212. doi:10.1016/s0886-3350(97)80317-3
- Kumar D, Agarwal A, Sivangnanam S, Chandrasekar R, Agarwal A. Implantation of glued intraocular lenses in eyes with microcornea. J Cataract Refract Surg. 2015;41(2):327–333. doi:10.1016/j.jcrs.2014.05.039