Abstract
Ovarian hyperstimulation syndrome (OHSS) is an exaggerated response to excess hormones and is also one of the life-threatening iatrogenic complications which is associated with ovulation induction. This syndrome usually occurs in women who receive injectable hormones for the stimulation of egg development in the ovaries. This study describes a rare case of moderate ovarian hyperstimulation syndrome which has been managed and treated with high-dose cabergoline. The patient was diagnosed in the Medical Imaging and Radiation Sciences Department of Kabul University of Medical Sciences and treated in Shahrara Teaching Hospital. A 26-year-old woman was diagnosed with the development of bilateral moderate ovarian hyperstimulation syndrome after receiving clomiphene citrate in dose of 100 mg BID on day 5 of period and Human Chorionic Gonadotropin (HCG) 10,000 units for egg release on day 14 of period. The patient was given a high dose of cabergoline. The dose was adjusted to 1 mg/day for eight days since she was diagnosed with ovarian hyperstimulation syndrome. Consequently, the main outcome of our intervention was complete resolution of OHSS as well as complete recovery of the patient. As a result, it is concluded that the high dose of cabergoline prevents and reduces the occurrence, prolongation, and severity of ovarian hyperstimulation syndrome. However, more assessments through randomized controlled trials regarding the efficacy and safety of cabergoline doses and treatment duration for treatment and preventive purposes are required.
Introduction
Ovarian Hyperstimulation Syndrome (OHSS) is an exaggerated response to excess hormones and is also one of the life-threatening iatrogenic complications which is associated with ovulation induction.Citation1,Citation2 This syndrome usually occurs in women who receive injectable hormones for the stimulation of egg development in the ovaries. OHSS causes ovarian swelling, enlargement, pain, development of multiple follicular cysts, and fluid leakage from intravascular to extravascular spaces.Citation3 This condition will either happen spontaneously with an unclear etiology or due to receiving fertility medicine to produce more follicles than usual. Generally, the majority of cases of OHSS are mild, which are characterized by temporary discomfort; however, the severe cases of the syndrome are rare, yet more likely to be potentially life threatening.Citation4
In terms of OHSS classification, the most accepted division is described as mild, moderate and severe by Golan et al.Citation5 Specialists should be familiar with the consequences of OHSS which could shift from a moderate to severe condition within a few hours.Citation6
In order to treat and manage Ovarian Hyperstimulation Syndrome, many treatment options are proposed that include cabergoline as a crucially important method. Cabergoline with the dopamine agonist effect can inhibit the vascular permeability and can prevent and decrease the symptoms related to the syndrome.
Objective
This study aimed to describe a case of moderate ovarian hyperstimulation syndrome which has been managed with cabergoline high-dose treatment.
Case Presentation
We report the case of a 26-year-old nulligravida woman married for 1.5 years. She presented with a chief complaint of moderate suprapubic and abdominal pain and history of taking 50 mg BID clomiphene citrate for ovulation induction to treat primary infertility and 10,000 units of HCG for release of egg after maturation of two oocytes in both ovaries. Moreover, it is worth mentioning that the patient received clomiphene citrate for 3 consecutive months before this complication. The response to this dosage of clomiphene citrate was maturation of one follicle each time. There was no history of OHSS during those cycles.
Physical examination results were considered unremarkable. Patient’s vital signs were monitored and the results were: blood pressure, 110/70 mm Hg, pulse rate of 72 beats per minute, body temperature of 36.2°C, respiration rate of 17/min, and BMI of 26.2 kg/m2. Furthermore, serum prolactin, TSH, FSH, LH levels, estrogen levels, electrolytes and serum creatinine were within normal ranges. Coagulation profile and platelets count were also in normal limits.
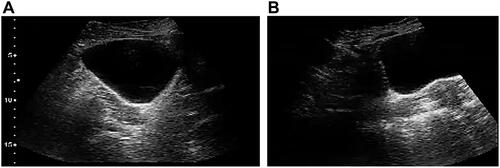
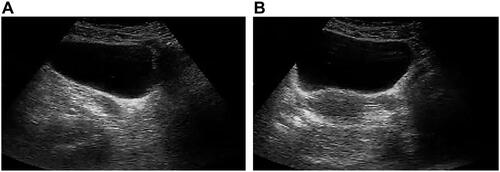
Ultrasound findings revealed bilateral ovarian hyperstimulation with multiple dilated cystic structures on both sides of ovaries, as seen in and .
Figure 1 (A) Right ovary transverse ultrasound image shows enlarged right ovary with multiple cysts of various size consistent with ovarian hyperstimulation. (B) Left ovary transverse ultrasound image shows enlarged left ovary with multiple cysts of various size consistent with ovarian hyperstimulation.
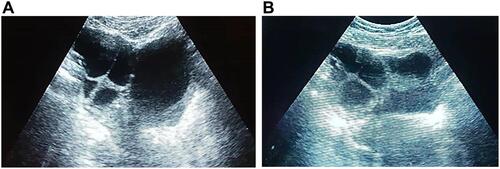
Figure 2 (A) Right ovary sagittal ultrasound image shows enlarged right ovary with multiple cysts of various size consistent with ovarian hyperstimulation. (B) Left ovary sagittal ultrasound image shows enlarged left ovary with multiple cysts of various size consistent with ovarian hyperstimulation.
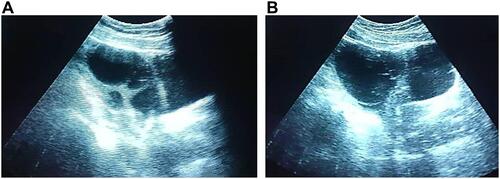
The patient was treated immediately upon diagnosis of ovarian hyperstimulation with high dose cabergoline which was administered 1 mg/day orally for 8 days. Increasing the daily Cb2 dose to the patient was for the purpose of preventing the progression of the already established syndrome by further decreasing the numbers of Vascular Endothelial Growth Factor Receptor 2 (VEGFR2) that was available for stimulation by the Vascular Endothelial Growth Factor (VEGF) molecules in the circulation. VEGFR2, a primary responder to vascular endothelial growth factor signal, regulates endothelial migration and proliferation. As a result of increasing Cb2 dose, the symptoms did not progress in the patient. Meanwhile the treatment cycle’s simultaneous ultrasound scans were monitored in order to assess the effectiveness of treatment and any sign of severity. Finally, it was found out that the patient tolerated the dose very well and the final result was resolution of OHSS and complete recovery of the patient from the condition with no complications, as shown in and . The supportive treatment in this case consisted of close observation, bed rest, provision of adequate fluids and painkillers.
Discussion
In mothers with Assisted Reproduction Treatment (ART), severe forms of ovarian hyperstimulation syndrome can rise in around 0.5–5%, which have caused maternal death. As previously indicated, this is a life-threatening syndrome because of its unknown pathophysiology and complications associated with this syndrome.Citation7 The treatment protocols of ovarian hyperstimulation syndrome are mostly symptomatic because of its unidentified pathophysiologic term. Although OHSS is a dangerous condition, all established treatments are symptomatic and there is no treatment available based on the pathophysiology of this condition. It seems that increased vascular permeability is the main pathophysiological aspect related to OHSS.Citation8
Some studies showed that egg donors and patients with high risk of ovarian hyperstimulation syndrome responded well and showed satisfactory results with a cabergoline daily dose of 0.5 mg starting from the day of HCG administration. This reduction was reported to be 20% among women at high risk of OHSS.Citation9 In another study the incidence of OHSS was reduced among women with polycystic ovaries who were undergoing cabergoline treatment due to hyperprolactinemia during ovulation induction.Citation10 A meta-analysis by Tang et al. concluded that the usage of cabergoline reduces the risk of OHSS in high-risk women particularly those suffering moderate OHSS and it has no adverse effect on pregnancy outcome (the clinical pregnancy rate and abortion rate). There is no increased risk of adverse events.Citation11
A series of experiments conducted by Gomez et al. in a rat-model of OHSS intended to examine gene expression patterns, relations between VEGF/VEGFR2 system, dopamine agonists, dopamine receptors, and vascular permeability. In the studies, it was described that the overstimulated rats shown considerable decrease in the amount of tyrosine hydroxylase enzyme which is a rate-limiting enzyme in dopamine synthesis. Dopamine administration was shown previously to reduce the vascular permeability through decreasing VEGFR2 phosphorylation in in vivo and in vitro cancer models.
Based on the findings, the analysis by the authors showed that effects associated with a dopamine agonist Cb2 with a dose of 10–25 mg/kg significantly reduces the VEGFR2 dependent vascular permeability in ovarian hyperstimulation syndrome rats. The observations which are done by the authors in animal models and the safety of Cb2 in human pregnancy necessitated further clinical studies on humans.Citation12
A randomized controlled trial study conducted by Alvarez et al. showed that the oocyte donors who are at high risk of ovarian hyperstimulation syndrome had lower incidence of moderate and severe OHSS in the Cb2 group and no adverse effects were reported on ovarian physiology. In the same study, it was reported that the women who received Cb2 for OHSS prevention had similar implantation and pregnancy rates as the woman matched for age, embryo quality, and semen parameters in a retrospective analysis.Citation9
In one more recently published randomized trial, 166 women at high risk of ovarian hyperstimulation were included and the result revealed that the administration of prophylactic Cb2 decreased the incidence of early OHSS.Citation7
The incidence reported was 31.4% (11/35) moderate or severe early OHSS in the Cb2 arm of the donor study and that none of the women developed early OHSS in the latter trial conducted in women undergoing treatment with their own gametes. However, the incidence of late onset OHSS was reported to be 10.8%.Citation13
Treatment with cabergoline seems to be effective in reducing OHSS menace in high-risk women especially women prone to moderate OHSS. In addition, treatment with cabergoline neither increases the risk of adverse effects nor affects the pregnancy outcomes.Citation14
Conclusion
It is safe to say that the high dose of cabergoline is effective in inhibiting and diminishing the development of OHSS incidence, elongation, and the intensification in severity of ovarian hyperstimulation. However, further randomized controlled trials regarding the effectiveness and safety of cabergoline dosages and treatment period for treatment and preventive purposes are needed.
Abbreviations
ART, Assisted Reproduction Treatment; HCG, Human Chorionic Gonadotropin; OHSS, Ovarian Hyperstimulation Syndrome; VEGF, Vascular Endothelial Growth Factor; VEGFR2, Vascular endothelial growth factor receptor 2.
Ethical Consideration
A written informed consent, which was translated into the local language, was obtained from the patient with the view to publish the article and the associated ultrasound images. Ethical approval was also obtained from Institutional Review Board of Kabul University of Medical Sciences.
Disclosure
The authors report no conflicts of interest in this work.
Additional information
Funding
References
- Kasum M, Oresković S, Jezek D. Spontaneous ovarian hyperstimulation syndrome. Coll Antropol. 2013;37(2):653–656.
- Rastin Z, Ghomian N, Khadem-Rezaiyan M. Severe ovarian hyperstimulation syndrome in A spontaneous pregnancy with normal singleton fetus: a case report. Iran J Nurs Midwifery Res. 2019;24(4):310–312.
- Sansone P, Aurilio C, Pace MC, et al. Intensive care treatment of ovarian hyperstimulation syndrome (OHSS). Ann N Y Acad Sci. 2011;1221:109–118. doi:10.1111/j.1749-6632.2011.05983.x
- Carizza C, Abdelmassih V, Abdelmassih S, et al. Cabergoline reduces the early onset of ovarian hyperstimulation syndrome: a prospective randomized study. Reprod Biomed Online. 2008;17(6):751–755. doi:10.1016/S1472-6483(10)60401-4
- Golan A, Ron-el R, Herman A, Soffer Y, Weinraub Z, Caspi E. Ovarian hyperstimulation syndrome: an update review. Obstet Gynecol Surv. 1989;44(6):430–440. doi:10.1097/00006254-198906000-00004
- Abuzeid M, Warda H, Joseph S, et al. Outpatient Management of Severe Ovarian Hyperstimulation Syndrome (OHSS) with placement of pigtail catheter. Facts Views Vis Obgyn. 2014;6(1):31–37.
- Alvarez C, Alonso-Muriel I, García G, et al. Implantation is apparently unaffected by the dopamine agonist Cabergoline when administered to prevent ovarian hyperstimulation syndrome in women undergoing assisted reproduction treatment: a pilot study. Human Reprod. 2007;22(12):3210–3214. doi:10.1093/humrep/dem315
- Saharkhiz N, Akbari Sene A, Salehpour S, Tamimi M, Vasheghani Farahani M, Sheibani K. Treatment results of high dose cabergoline as an adjuvant therapy in six patients with established severe ovarian hyperstimulation syndrome. Iran J Reprod Med. 2014;12(10):713–716.
- Alvarez C, Martí-Bonmatí L, Novella-Maestre E, et al. Dopamine agonist cabergoline reduces hemoconcentration and ascites in hyperstimulated women undergoing assisted reproduction. J Clin Endocrinol Metab. 2007;92(8):2931–2937. doi:10.1210/jc.2007-0409
- Papaleo E, Doldi N, De Santis L, et al. Cabergoline influences ovarian stimulation in hyperprolactinaemic patients with polycystic ovary syndrome. Human Reprod. 2001;16(11):2263–2266. doi:10.1093/humrep/16.11.2263
- Kalampokas T, Creatsas G, Kalampokas E. Cabergoline as treatment of ovarian hyperstimulation syndrome: a review. Gynecol Endocrinol. 2013;29(2):98–100. doi:10.3109/09513590.2012.730578
- Gomez R, Gonzalez M, Simon C, Remohi J, Pellicer A. Tyroxine hydroxylase (TH) downregulation in hyperstimulated ovaries reveals the dopamine agonist bromocriptine (Br2) as an effective and specific method to block increased vascular permeability (VP) in OHSS. Fertil Steril. 2003;80:43–44. doi:10.1016/S0015-0282(03)01918-6
- Ata B, Seyhan A, Orhaner S, Urman B. High dose cabergoline in management of ovarian hyperstimulation syndrome. Fertil Steril. 2009;92(3):1168.e1–.e4. doi:10.1016/j.fertnstert.2009.05.021
- Tang H, Hunter T, Hu Y, Zhai SD, Sheng X, Hart RJ. Cabergoline for preventing ovarian hyperstimulation syndrome. Cochrane Database Syst Rev. 2012;2:Cd008605.