Abstract
A 60-year-old male farmer was admitted to the hospital with dysphagia for 2 months, and minimally invasive McKeown esophagectomy with lymphadenectomy was initially planned. However, congenital absence of the right gastroepiploic vessels (RGEVs) was blocked surgical procedure. Fortunately, we successfully performed esophagectomy and unconventional gastric remnant reconstruction without RGEVs, and intraoperative cervical venous superdrainage.
Introduction
Esophageal cancer (ESCC) is one of the most common upper gastrointestinal malignancies in the world. Currently, the standard paradigm for treating ESCC is a comprehensive treatment, mainly based on surgery.Citation1 Clinically, the stomach is the preferred organ for digestive reconstruction after esophageal resection, and the blood supply to the gastric conduit is a crucial factor in determining the success of the reconstruction.Citation2,Citation3 During surgery, it is particularly important to explore and protect the right gastroepiploic artery (RGEA), which is the main source of blood in the reconstructed stomach. Although congenital absence of the right gastroepiploic vessels (RGEVs) is relatively rare, we encountered this case. In this case, we successfully performed esophagectomy and unconventional gastric remnant reconstruction without RGEVs, and intraoperative cervical venous superdrainage.
Case Report
A 60-year-old male farmer was admitted to the hospital due to 2 months of dysphagia with no history of abdominal trauma or surgery was admitted to the hospital for 2 months. Endoscopy revealed a neoplasm at 28–33 cm from the incisors, and biopsy confirmed squamous cell carcinoma. Further, whole-body positron emission tomography (PET) scans indicated that the uneven thickening of the middle and lower esophagus was FDG-avid, and no extraesophageal invasion was present. Therefore, the tumor was clinically staged as cT3NxM0, and minimally invasive McKeown esophagectomy with lymphadenectomy was initially planned.
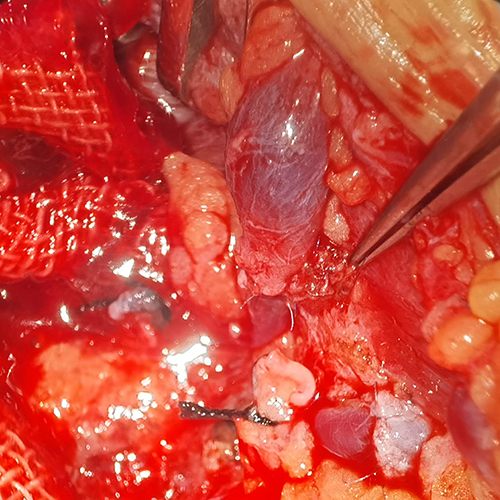
Thoracic surgery was first started with thoracoscopy through the right chest, esophageal mobilization, and mediastinal lymph node dissection, which proceeded smoothly. Subsequently, the abdominal surgery was performed laparoscopically in the supine position. Unexpectedly, RGEVs were not found in the greater curvature of the stomach near the pylorus, suggesting congenital absence of RGEVs (). After thorough exploration by laparoscopy, during which the right gastric artery was a major conduit supplying blood to the stomach, we decided to perform an open operation for whole-gastric reconstruction. The stomach was fully mobilized by dividing the left gastric artery, the short gastric arteries, and the posterior gastric artery. Subsequently, the blood supply to the gastric remnant was observed for 30 min, and only the right gastric artery was preserved. Intriguingly, because there was no ischemia of the gastric mucosa, a manual gastroesophageal anastomosis was performed via the retrosternal route to the left neck. Furthermore, microvascular anastomosis of the short gastric vein to the left anterior cervical vein was performed for superdrainage (). Finally, jejunostomy was performed to provide nutritional support.
Figure 1 Congenital absence of the right gastroepiploic vessels (RGEVs). ☆Greater curvature of stomach, ☆Lesser curvature of stomach.
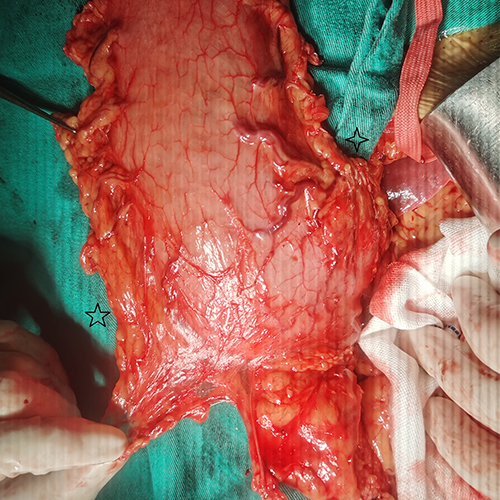
Figure 2 Microvascular anastomosis of the short gastric vein to the left anterior cervical vein to superdrainage.
Postoperatively, to prevent thrombosis, anticoagulation with low-molecular-weight heparin was started, and other routine measures such as gastrointestinal decompression, nutritional support, and infection prevention were implemented. On postoperative day 7, upper gastrointestinal radiography did not reveal any anastomotic fistula or esophageal stenosis. The patient was discharged on postoperative day 10 without complications. Histopathological examination revealed esophageal squamous carcinoma staged as pT3N2M0, and no signs of discomfort or recurrence were reported at 1-year follow-up.
Discussion
During surgery for esophageal cancer, RGEA is used as the main blood supply vessel for the gastric conduit, and intraoperative exploration and protection are particularly important. To date, the epidemiology of RGEVs absence and intraoperative injury has been unclear. To the best of our knowledge, this is the first reported case of congenital absence of RGEVs. As is known to us all, RGEA rarely varies in its origin, mainly comes from the gastroduodenal artery, and occasionally aberrantly originates from the superior mesenteric artery.
In one study of 28 cadaver dissections by Jiang et al, RGEA was found to be present in all cases, whereas the left gastroepiploic artery was absent in two cases.Citation4 In other studies of 17 specimens from Japan and 100 specimens from France, RGEA was present in all the cases.Citation5,Citation6 In this case, the patient did not find a RGEA during intraoperative exploration and had no previous history of abdominal surgery, suggesting a congenital absence, resulting in the inability to perform the planned operation. In such cases, the congenital absence of the RGEA was considered to contribute to the development of other main gastric arteries, which appeared to be larger. Therefore, we successfully performed whole-gastric reconstruction, in which the blood supply was the right gastric artery alone, and microvascular anastomosis of the short gastric vein to the left anterior cervical vein.
While congenital absence of RGEA has not been reported, there are some reports of successful esophagogastrostomy in patients with acquired absence of RGEA. Chen et al reported a case of ESCC with acquired absence of RGEA, which was attributed to a history of right hemicolectomy using an unconventional whole gastric conduit to complete cervical reconstruction. Postoperative angiography suggested that the right gastric artery was the only source of blood supply to the gastric conduit.Citation7 Charalampous et al reported a patient with ESCC without RGEA due to a duodenal bleeding ulcer treated with gastroduodenal artery ligation 10 years ago who underwent transthoracic esophagectomy using a gastric conduit to restore gastrointestinal continuity.Citation8 Neither of the two cases experienced postoperative complications, such as anastomotic leakage. Hence, it is feasible to supply the gastric replacement esophagus with the right gastric artery in the absence of RGEA.
Blood supply to the gastric conduit could be a major risk factor for complications associated with esophageal cancer treatment. Additionally, some of the reasons for anastomotic leakage are a deficient arterial blood supply and insufficient venous outflow. Uchiyama et al proposed techniques, such as arterial supercharge or venous superdrainage. After superdrainage, the color of the gastric reconstruction is usually restored, and the arterial stump pulsation is strong enough that the supercharge is no longer necessary.Citation9,Citation10 Therefore, in the absence of RGEA, it is particularly important to assess whether supercharge or superdrainage should be performed. In this case, the short gastric artery stump pulsated well. We considered supercharge in the neck unnecessary and performed microvascular anastomosis of the short gastric vein to the left anterior cervical vein to the superdrainage. Interestingly, Fujii et al performed esophagectomy and gastric remnant reconstruction with preoperative selective arterial embolization and intraoperative supercharge in a patient with an occluded RGEA.Citation11 Thus, microvascular anastomosis to the supercharge or superdrainage can reduce the incidence of gastroesophageal anastomotic complications. Further research is needed to confirm this hypothesis.
Conclusion
To the best of our knowledge, this is the first reported case of congenital absence of the right gastroepiploic vessels. Fortunately, we successfully performed esophagectomy and unconventional gastric remnant reconstruction without RGEVs, and intraoperative cervical venous superdrainage.
Abbreviations
RGEVs, right gastroepiploic vessels; ESCC, Esophageal cancer; RGEA, right gastroepiploic artery; PET, positron emission tomography.
Informed Consent Statement
We have obtained the written informed consent from the patient for publication of this case report and any accompanying images. No institutional approval is required to publish case details.
Disclosure
The authors report no conflicts of interest in this work.
Additional information
Funding
References
- Qi J, Li M, Wang L, et al. National and subnational trends in cancer burden in China, 2005–20: an analysis of national mortality surveillance data. Lancet Public Health. 2023;8(12):e943–e955. doi:10.1016/s2468-2667(23)00211-6
- Blumenstein I. Gastroenteric tube feeding: techniques, problems and solutions. World J Gastroenterol. 2014;20(26):8505. doi:10.3748/wjg.v20.i26.8505
- Deana C, Vetrugno L, Bignami E, Bassi F. Peri-operative approach to esophagectomy: a narrative review from the anesthesiological standpoint. J Thorac Dis. 2021;13(10):6037–6051. doi:10.21037/jtd-21-940
- Jiang T, Li M, Zhao M, et al. Vascular anatomy of the stomach and its application in gastric tube reconstruction during esophagectomy. Chin J Clin Oncol. 2019;46(03):126–129.
- Tomioka K, Murakami M, Saito A, et al. Anatomical and surgical evaluation of gastroepiploic artery. Okajimas Folia Anat Jpn. 2016;92(3–4):49–52. doi:10.2535/ofaj.92.49
- Settembre N, Labrousse M, Magnan PE, et al. Surgical anatomy of the right gastro-omental artery: a study on 100 cadaver dissections. Surg Radiol Anatomy. 2017;40(4):415–422. doi:10.1007/s00276-017-1951-7
- Ma L, Liu C, Mei J, Chen L-Q. Successful cervical esophageal reconstruction using gastric conduit without gastroepiploic artery. Ann Thorac Surg. 2019;107(6):e409–e410. doi:10.1016/j.athoracsur.2018.09.068
- Charalampous C, Kofopoulos-Lymperis E, Pikouli A, et al. Gastric conduit reconstruction after esophagectomy with right gastroepiploic artery absence: a case report. J Surg Case Rep. 2023;2023(8). doi:10.1093/jscr/rjad474
- Uchiyama H, Shirabe K, Morita M, et al. Expanding the applications of microvascular surgical techniques to digestive surgeries: a technical review. Surg Today. 2012;42(2):111–120. doi:10.1007/s00595-011-0032-5
- Chen L, Zhang J, Chen D, Sang Y, Yang W. Simultaneous vascular reconstruction and cervical anastomosis in McKeown esophagectomy. Front Surg. 2021;8. doi:10.3389/fsurg.2021.646811
- Fujii M, Okada N, Shichinohe R, Sakurai Y, Kinoshita Y. Gastric remnant reconstruction with left gastroepiploic artery supercharge after esophagectomy in a patient with an occluded right gastroepiploic artery: a technical and case report. Int J Surg Case Rep. 2021;82:105876. doi:10.1016/j.ijscr.2021.105876
