Abstract
Transfusion-associated circulatory overload (TACO) is a potentially fatal blood transfusion complication that often presents itself within 12 hours of transfusion cessation. We present a case of TACO in an orthopedic surgery patient to highlight the importance of anticipating and managing complications of blood loss and transfusion in an otherwise healthy patient.
Introduction
Pulmonary-related blood transfusion reactions have become an increasing area of study/focus since the 1990s as the ability to recognize and diagnose these reactions has improved in the following decades. National hemovigilance networks have continued to collect incidence reporting and updated diagnostic criteria to better delineate between the different transfusion reactions and standardized diagnosing. Transfusion-associated circulatory overload (TACO) was the most common cause of transfusion-associated fatalities from 2017–2021, claiming 32% of the cases. Prior to 2017, TRALI was consistently the leading cause, more likely due to under-reporting of TACO than actual incidences.Citation1 The majority of cases have been found in the critically ill population with mortality in up to 6.5% of all cases.Citation2,Citation3 From 2000 to 2010, the National Haemovigilance Office at the Irish Blood Transfusion Service found TACO incidence to be one in 9177.Citation4 The frequency of under-reporting had previously been due to poor defining criteria and overlapping symptomatology. The updated diagnostic criteria of TACO in 2021 by the National Healthcare Safety Network require new onset or exacerbation within 12 hours of transfusion cessation and either evidence of acute or worsening respiratory distress, pulmonary edema, elevated BNP, or cardiovascular system changes not explained by another underlying medical condition. The current proposed mechanism of TACO is a two-hit model: the first being the underlying pre-existing condition/risk factor and the second being the transfusion.Citation3 This case showcases an unexpected activation of the massive transfusion protocol in an orthopedic trauma surgery in an otherwise healthy patient resulting in TACO and highlights the importance of monitoring for and reporting such transfusion reactions in the operating room.
Report
Patient Presentation: A 30-year-old healthy male with no past medical or surgical history presented after a motor vehicle collision resulting in a left femoral fracture requiring an urgent surgical fixation. Other presenting injuries included pulmonary contusion of the right upper lobe and a right acetabular fracture that would require a future repair. On admission to the emergency department, the patient was GCS 15, without any neurological deficits, and he was initially managed with pain medication and a right hip reduction in the emergency department. Initial labs showed Hb 13.7, Hct 40.4, WBC 17.3 and platelets 276. General surgery was consulted to evaluate the pulmonary contusion, which was determined to be minor and did not require intervention. The patient was evaluated by the anesthesiology team and determined to be an American Society of Anesthesiology (ASA) status 1E, a healthy patient with no comorbidities requiring an urgent or emergent surgical intervention.
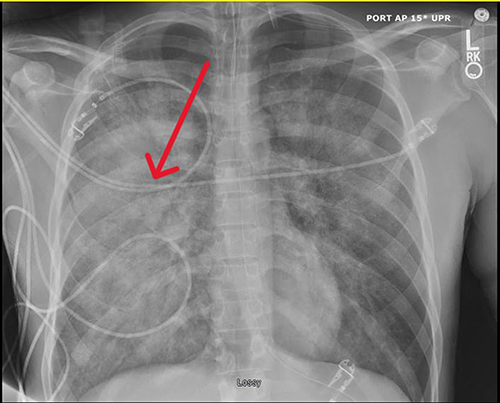
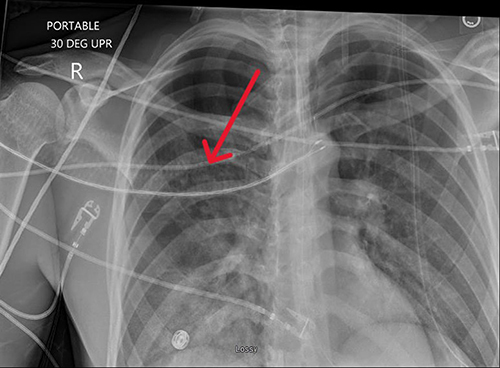
Clinical Course: The patient was taken to surgery the following morning for a surgical fixation with intramedullary nail of the left femur. Perioperatively, vitals and hemodynamics were stable through induction and the first five hours of surgery when the patient suddenly had sustained tachycardia. At that time, the surgeon noticed a large bleed from the deep vein, thought to be an iatrogenic injury from one of the bone spikes, with an estimated 1100cc of blood loss in the next thirty minutes requiring massive transfusion protocol activation and vascular surgery involvement to control venous hemorrhage. Within an hour after the first unit, pink frothy sputum was noticed in the endotracheal tube (ETT) and the patient began having increased PEEP requirements. Fiberoptic bronchoscopy was performed, the ETT was suctioned in an attempt to clear the airway. However, even though the patient was having symptoms of pulmonary edema likely secondary to volume overload of transfused products, vascular surgery was still working on controlling the bleeding and the patient required more blood products. Once the bleeding was controlled, orthopedic surgery finished the femoral fixation. By the end of the case he was transfused 23 units PRBCs, 26 units platelets and 2 units of FFP and given 4 liters of crystalloid and 500cc of albumin. With clear evidence of pulmonary edema, he was given 40mg of furosemide and a central venous line was placed with initial CVP >18. The patient ultimately remained intubated post-operatively and admitted to the surgical ICU. A post-operative chest x-ray showed bilateral lung opacification and pulmonary edema(). His postoperative course was complicated by requiring being positioned prone and paralyzed for oxygenation and ventilation requirements and three days of diuresis with furosemide, receiving a total of 120mg(). Postoperative coagulation studies were unremarkable (PTT 28.2, PT/INR: 12.6/1.2, Fibrinogen 189, D-Dimer 2.8) and BNP was unfortunately not drawn despite multiple providers citing TACO as his diagnosis in his chart. He was subsequently extubated three days after surgery. He returned to the operating room twice more for wound vacuum management and fixation of his right acetabulum fracture. He was discharged two weeks after admission, requiring a wheelchair for mobility until further physical and occupational therapy.
Discussion
Orthopedic surgery procedures on femur fractures are routine and are not usually at high risk of complications leading to TACO, especially in younger patient populations. TACO incidence varies across patient cohorts, with rates ranging from 1% in admitted patients to 5.5% in those undergoing intra-operative transfusions and can lead to substantial morbidity, leading to outcomes like intensive care admission, intubation, mechanical ventilation, and, in severe cases, mortality, reaching up to 6.5%.Citation3 Up to 8% of the TACO cases in admitted patients occur in orthopedic cases, and the patient population affected is often the critically ill and elderly.Citation5 In this patient, although he was massively transfused, his overall healthy background and no risk factors did not make him an obvious case to be complicated by TACO.
Indications of when and what products to transfuse have been widely discussed and despite multiple published guidelines, there is an unquantifiable factor of clinical judgment, which is particularly key in the rapidly changing operating room environment, when lab results may lag behind visual clinical assessment. The ASA currently recommends employing a multimodal protocol or algorithm but there are no specific recommendations on which one is superior.Citation6 Despite the widespread implementation of damage control resuscitation in the last two decades showing significant reductions in mortality after major trauma hemorrhages,Citation7 TACO remains a frequent complication in such cases. Morbidity and mortality numbers are still high and further exploration into specific risk factors, particularly those specific to perioperative periods, should be investigated. Common practice employs restrictive fluid resuscitation and permissible hypotension to minimize bleeding, and in this Report, transfusions were not started until active rapid hemorrhage which thus led to rapid massive transfusion of products. He was not being heavily fluid resuscitated earlier in the case given his stable vitals and appearance, and in addition to the massive blood loss, required a larger resuscitation than may have required if earlier resuscitation had been initiated and allowed for slower transfusion or less amount transfused.
Understanding and preventing TACO in healthy surgical patients such as this one is challenging due to limited literature on OR-specific incidences and the lack of pathognomonic signs and symptoms for TACO.Citation8 We were able to find studies that reveal under-reporting in high transfusion settings, emphasizing the need for hemovigilance and education.Citation4,Citation9 In 2016, analysis across four tertiary hospitals found only 5.1% of suspected TACO cases were reported to the transfusion service.10 A 2022 study found that only 21.8% of cases documented in the Electronic Health Record (EHR) were also recorded as cases in the Blood Bank (BB) databases, and approximately 65% of EHR cases had no data reported to transfusion medicine.Citation11 Current recommendations for TACO prevention entail limiting unnecessary transfusions and to avoid rapid transfusion rates. However, in MTPs, this is often not possible as accurate lab values are often delayed and the patients are visibly losing blood and require rapid replacement. One lab value that helps guide the diagnosis of TACO is a BNP level, with a post/pre-transfusion NT-proBNP ratio >1.5 aiding in diagnosis, or BNP<300 or NT-proBNP <2000pg/mL making diagnosis less likely. However, there is no clear cut-off to exclude TACO.Citation8
Conclusion
Addressing reporting challenges underscores the importance of educating care teams on reporting events and complications, particularly in the operating room where events may be buried in the anesthetic record and not documented elsewhere. At our institution, our EHR allows for reporting “notable events” which are evaluated separately by providers for quality improvement. However, the majority of events are often only documented in the anesthetic record and not in this separate section for further evaluation. Additionally, diagnostic criteria have been recently updated in 2018 by the CDC’s Hemovigilance Adverse Reaction Case Classification Criteria on TACO. A study on the impact of changing the TACO definition revealed that under the 2011 ISBT definition, 26 out of 48 TACO cases in 2018 would not have been classified as TACO or lacked sufficient details.Citation12 With the criteria requiring radiographic or laboratory evidence indicating TACO, it is possible that diagnosing intra-operative TACO may be difficult as treatment often starts immediately and such labs or imaging may not be drawn or evaluated until the post-operative period, after which the patient may be showing signs of improvement and no longer meet diagnostic criteria.
In Conclusion, as the leading cause of transfusion related complications, TACO remains under-reported in all facilities but possibly more so in the operating room both due treatment before diagnosis and difficulty with how reports are collected. It is imperative to standardize reporting and also create avenues to report suspected and treated cases. This case highlights the need to increase investigation into more specific risk factors that may aide in the diagnosis and the importance of institutional processes that allow for streamlined reporting of cases to allow for more frequent and accurate reporting of cases to a national level.
Ethics
This case report is devoid of patient identifiable information, it is exempt from IRB review requirements and meets informed consent guidelines as per the Medical College of Wisconsin policy This article adheres to the applicable CAse REport (CARE) guidelines.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest in this work.
References
- U.S. Centers for Disease Control and Prevention. The National Healthcare Safety Network (NHSN) Manual: Biovigilance Component v2.5. Atlanta, GA: Division of Healthcare Quality Promotion, National Center for Emerging and Zoonotic Infectious Diseases; 2023.
- Bulle EB, Klanderman RB, Pendergrast J, et al. The recipe for TACO: a narrative review on the pathophysiology and potential mitigation strategies of transfusion-associated circulatory overload. Blood Rev. 2022;52:100891. doi:10.1016/j.blre.2021.100891
- Semple JW, Rebetz J, Kapur R. Transfusion-associated circulatory overload and transfusion-related acute lung injury. Blood. 2019;133(17):1840–1853. doi:10.1182/blood-2018-10-860809
- Piccin A, Cronin M, Brady R, Sweeney J, Marcheselli L, Lawlor E. Transfusion-associated circulatory overload in Ireland: a review of cases reported to the National Haemovigilance Office 2000 to 2010. Transfusion. 2015;55(6):1223–1230. PMID: 25522667. doi:10.1111/trf.12965
- Hendrickson JE, Hillyer CD. Chapter 63 - Transfusion-Associated Circulatory Overload. In: Abrams, Transfusion Medicine and Hemostasis. 2nd ed. Elsevier; 2013:413–415. doi:10.1016/B978-0-12-397164-7.00063-X
- Kwak J, Wilkey AL, Abdalla M, Joshi R, Roman PE, Greilich PE. Practice guidelines for perioperative blood management: an updated report by the American society of anesthesiologists task force on perioperative blood management*. Anesthesiology. 2015;122(2):241–275. doi:10.1097/ALN.0000000000000463
- Cole E, Weaver A, Gall L, et al. A decade of damage control resuscitation: new transfusion practice, new survivors, new directions. Ann Surg. 2021;273(6):1215–1220. doi:10.1097/SLA.0000000000003657
- Klanderman RB, Bosboom JJ, Migdady Y, et al. Transfusion-associated circulatory overload-a systematic review of diagnostic biomarkers. Transfusion. 2019;59(2):795–805. PMID: 30488959; PMCID: PMC7379706. doi:10.1111/trf.15068
- Piccin A, Spizzo G, Popovski MA, et al. Transfusion-associated circulatory overload in gastroenterology. Blood Transfusion. 2021;19(3):197–204. doi:10.2450/2020.0086-20
- Hendrickson JE, Roubinian NH, Chowdhury D, et al.; National Heart,Lung, and Blood Institute (NHLBI) Recipient Epidemiology and Donor Evaluation Study (REDS-III). Incidence of transfusion reactions: a multicenter study utilizing systematic active surveillance and expert adjudication. Transfusion. 2016;56(10):2587–2596. doi:10.1111/trf.13730
- Jhaveri P, Bozkurt S, Moyal A, et al. Analyzing real world data of blood transfusion adverse events: opportunities and challenges. Transfusion. 2022;62(5):1019–1026. doi:10.1111/trf.16880
- Yuan Y, Dennington PM, Daly J, Baidya S, Tung JP. The impact of revised definitions for transfusion-associated circulatory overload and transfusion-related acute lung injury on haemovigilance reporting. Vox sanguinis. 2023;118(3):199–206. doi:10.1111/vox.13402