Abstract
A 46-year-old man with bicuspid aortic valve and severe calcific aortic stenosis was submitted to aortic valve replacement with a stented bioprosthesis. He developed Staphylococcus epidermidis prosthetic valve endocarditis a month later, presenting in the emergency room with acute myocardial infarction. The mechanism of myocardial ischemia was a large aortic root abscess causing left main extrinsic compression. He was urgently taken to the operating room, and an aortic root replacement with cryopreserved homograft was performed, associated with autologous pericardium patch closure of aortic to right atrium fistula and coronary artery bypass grafting of the left anterior descending. After a difficult postoperative period with multiple problems, he was eventually discharged home. At 36-month follow-up, he is asymptomatic with no recurrent infection, and the left main coronary artery is widely patent on control chest computed tomography.
Introduction
Although infrequent (1% to 4% in the first year), infective endocarditis may occur after aortic valve replacement.Citation1–Citation3 When present, prosthetic valve endocarditis is a severe problem that is associated with considerable morbidity, especially related to peripheral embolism, perivalvular abscess, and sepsis.Citation4–Citation9
Acute coronary syndromes are uncommon in prosthetic valve endocarditis, with a prevalence of between 1% and 3%.Citation10 The most likely mechanisms responsible for myocardial ischemia are the presence of preexisting coronary artery disease and coronary emboli from aortic vegetations. Other less frequent mechanisms have been described, such as obstruction of the coronary ostium due to large vegetation and severe aortic insufficiency.Citation10–Citation14 External coronary artery compression due to infective endocarditis is also a described mechanism, but is a rare occurrence with only few cases reported in medical literature.Citation11,Citation14–Citation21
We report a 46-year-old patient who presented with acute myocardial infarction caused by an aortic root abscess, which resulted in the external compression of the left main coronary artery.
Case description
A 46-year-old man presented at Instituto de Cardiologia do Distrito Federal, Brasilia, Brazil with a history of dyspnea and fatigue exacerbated by a recent hospitalization related to pulmonary edema. Diagnosis was confirmed by echocardiography, which revealed the presence of a bicuspid aortic valve with mixed lesion, predominantly stenotic. The left ventricle had moderate systolic dysfunction and severe concentric hypertrophy. Past medical history was consistent with hypertension. Surgery was indicated for symptomatic severe aortic stenosis. A preoperative coronary angiogram did not reveal any abnormalities. The patient was submitted to aortic valve replacement with a stented bioprosthesis. The operation and his postoperative recovery were uneventful, and the patient was discharged home on the sixth day after the procedure in good condition. He was prescribed the following medications to take at home: enalapril 5 mg twice daily, carvedilol 6.25 mg twice daily, furosemide 20 mg daily, and ferrous sulfate 300 mg daily (orally).
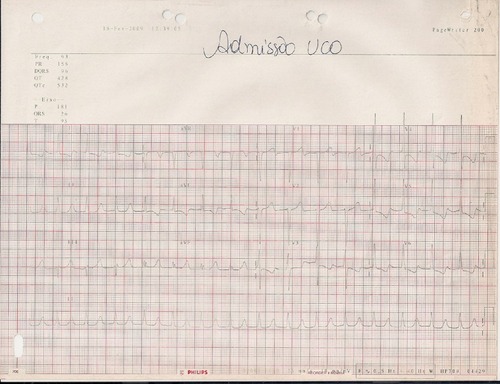
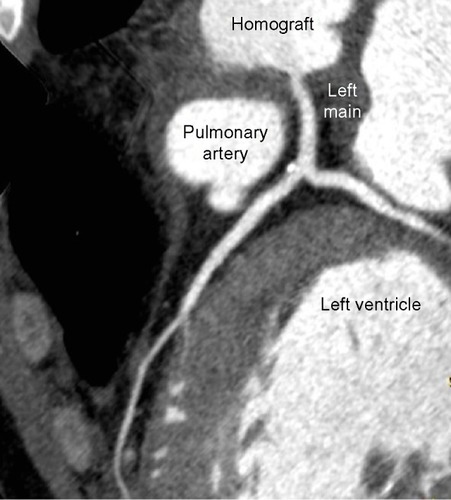
Approximately 1 month later, the patient returned, complaining of a high-grade fever and chills for a few days. He was admitted to the emergency department with acute onset chest pain, dyspnea, and vomiting. On physical exam, he was lethargic, febrile, pale, and hemodynamically unstable, with cold extremities and faint pulses. Admitting electrocardiogram revealed normal sinus rhythm, signs of left ventricle hypertrophy, and ST depression on posterior and lateral leads (). Laboratory values on admission demonstrated remarkable elevation of cardiac enzymes (). The cardiologist on call interpreted the patient as having non-ST elevation acute coronary syndrome, and treated him with aspirin, clopidogrel, morphine, and heparin. An emergent coronary angiogram () revealed a long, complex lesion on the left main coronary artery (80% lumen obstruction) with tapering contor, suggesting extrinsic compression. Due to ongoing myocardial ischemia and hemodynamic compromise, an intra-aortic balloon pump was inserted. The patient was further managed with intravenous fluids, inotropes, and mechanical ventilation. Blood cultures were drawn and identified as oxacillin-resistant Staphylococcus epidermidis. Before the blood cultures results were available, broad-spectrum anti biotics (vancomycin, rifampicin, and imipenem) and also an anti-fungal drug (amphotericin B) were initiated empirically. Renal function was impaired. Transesophageal echocardiog-raphy showed vegetations attached to the prosthesis, aortic root abscess, and an aortic-to-right-atrium fistula. Left ventricle ejection fraction was 36%, and there were wall motion abnormalities on lateral and anterior walls. Chest computed tomography () suggested that left main compression was due to aortic root abscess or hematoma.
Figure 2 Coronary angiogram and chest computed tomography.
Abbreviation: LAD, left anterior descending.
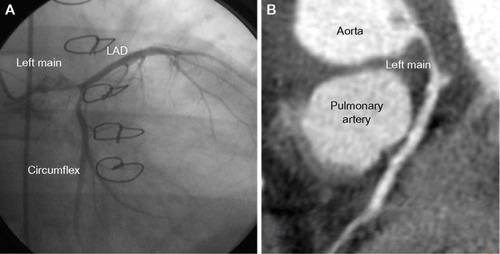
Table 1 Admitting laboratory values
Urgent reoperative aortic valve replacement was indicated. The operation was performed with the aid of hypothermic cardiopulmonary bypass with aortic and bicaval cannulation. Myocardial protection was achieved with cold blood cardioplegia delivered through the coronary ostium and coronary sinus. An oblique aortic arteriotomy revealed a large anterior aortic root abscess, which had invaded the left and right coronary cuspids. The bioprosthesis was removed, and the abscess was evacuated; complete debridement of all infected material was also performed. Both coronary buttons were carefully mobilized and cleaned of all infected tissue. The aortic annulus was severely destroyed by the infection. Aortic root replacement with cryopreserved homograft was performed using interrupted monofilament sutures. The coronary buttons were directly re-implanted on the homograft with continuous sutures. The aortic-to-right atrium fistula was closed with an autologous pericardium patch. Additionally, a coronary artery bypass grafting with a reversed saphenous vein graft to left anterior descending artery was performed. Prolonged cardiopulmonary bypass and mediastinal bleeding were problems in the operating room, requiring vigorous transfusion and delayed chest closure on the next day. Cultures drawn in the operating room were negative.
Postoperatively, the patient had acute renal failure requiring hemodialysis, sepsis, transient liver failure, prolonged mechanical ventilation, and complete atrioventricular block requiring permanent pacemaker. Antibiotic therapy, as previously mentioned, was initiated empirically with vancomycin, rifampicin, imipenem, and amphotericin B. Rifampicin was discontinued on the second day of use due to mild liver failure. Imipenem was used until the 14th postoperative day. Vancomycin was replaced by teicoplanin shortly after the operation due to acute renal failure, and it was used until the 30th postoperative day. Amphotericin B was used until the 34th postoperative day. Then, it was replaced by fluconazole, which was continued for a year thereafter. A month after the operation, the left ventricular function had improved (ejection fraction of 58%) with a mildly dilated ventricle and a normal aortic valve function.
The patient was discharged home 6 weeks after surgery in good condition, with no signs of active infection. At 36-month follow-up, the patient is currently in New York Heart Association functional class I with no recurrent infection, and the ventricular function is normal. The left main is widely patent and the saphenous vein graft is occluded on control chest computed tomography ().
Discussion
The present case describes a rare complication of prosthetic valve endocarditis, an aortic root abscess causing external coronary artery compression and acute myocardial infarction. This mechanism of myocardial infarction has already been described.Citation11,Citation14–Citation21 The most likely mechanisms responsible for myocardial infarction during infective endocarditis are preexisting coronary artery disease and coronary artery emboli from vegetations.
Prosthetic valve endocarditis is associated with elevated hospital mortality (approximately 40%)Citation22 and morbidity dependent on the infecting pathogen, duration of illness prior to therapy, and underlying comorbidities.Citation23 Mansur et alCitation24 presented a total of 386 complications in 223 episodes of endocarditis (74% complication rate), being 100 occurrences of cardiac complications (severe heart failure, valve injury, pericarditis, acute myocardial infarction, conduction abnormalities, fistulous communication, perivalvular abscess, and others), 72 neurologic complications (cerebral embolism, mycotic aneurysms, meningitis, stroke, intracranial hemorrhage, cerebral abscess, and others), 46 septic complications (infection unresponsive to treatment, persistent fever, disseminated intravascular coagulation, and others), 27 renal complications (renal failure, nephrotic syndrome), 16 extracranial systemic arterial complications, 26 septic pulmonary embolisms, three splenic infarctions or abscesses, and some other complications associated with infective endocarditis.
Clinical presentation of acute coronary syndromes in patients with endocarditis is similar to those with coronary artery disease. As systems attempt to meet stringent door-to-balloon initiatives, it becomes imperative that a detailed history and physical exam be performed in this narrow time window in order to avoid unnecessary tests and/or therapeutic regimens. For instance, the diagnostic work-up of a patient with a clinical history of high-grade fever and chills within a month after a straightforward aortic valve replacement with known absence of coronary artery disease includes, firstly, a transesophageal echocardiography.Citation17 It has a sensitivity and a specificity for abscess detection of 87% and 95%, respectively.Citation25 Coronary angiogram in this particular patient was indicated based on a misdiagnosis of coronary artery disease. Although the angiographic appearance is typical (complex and long lesion that often disappears on diastole), coronary angiogram should be avoided because it may cause dislodgment of septic fragments, which fortunately did not occur in this particular case.
The isolation of the causative organism of prosthetic valve endocarditis is essential, and antibiotic therapy should be delayed pending the blood culture results in cases of patients who are hemodynamically stable with an indolent clinical course. However, patients presenting hemodynamic instability or acute disease should receive empiric broad-spectrum antibiotic therapy promptly.Citation26 Therapy should be subsequently adjusted according to the culture results. The American Heart Association (AHA) and the European Society of Cardiology (ESC) guidelines recommend that prosthetic valve endocarditis should be treated for at least 6 weeks with adequate bactericidal agent.
Presence of acute coronary syndrome in the setting of prosthetic valve endocarditis carries an elevated morbidity and mortality rates.Citation27 Although uncommon, external compression of coronary artery should be considered in the differential diagnosis of these patients, and adequate diagnostic work-up and treatment should be indicated.Citation11 Treatment with anti-platelet agents increased the risk of cerebral bleeding and certainly complicated the operative treatment in this patient.Citation28 Although the patient was a very high-risk surgical candidate, the urgent operation was justified due to patient’s age and treatable heart problems, despite the presence of active infection, aortic root invasion, and abscess. Operative findings confirmed the severity of infection. The root abscess perforated the membranous septum, causing aortic to right atrium fistula, and there was a huge invasion of the left coronary cuspid around the left main coronary artery, which caused its extrinsic compression and myocardial ischemia. The treatment of prosthetic endocarditis was standard: extensive debridement, patch closure of fistula, and aortic root replacement with cryopreserved homograft.Citation29 Coronary artery bypass to left anterior descending was also performed in order to guarantee an adequate myocardial blood flow shortly after the operation. The adequate coronary button re-implant and obstruction relief established good coronary perfusion, and the saphenous vein graft has occluded due to competitive flow.
Conclusion
We experienced a rare complication of prosthetic valve endocarditis: external coronary artery compression due to aortic root abscess. Although uncommon, this mechanism should be considered in the differential diagnosis of patients presenting acute coronary syndrome in the setting of prosthetic valve endocarditis, and adequate diagnostic work-up and treatment should be indicated.
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- BayerASInfective endocarditisClin Infect Dis19931733133208218670
- GroverFLCohenDJOprianCHendersonWGSethiGHammermeisterKEDeterminants of the occurrence of and survival from prosthetic valve endocarditis. Experience of the Veterans Affairs Cooperative Study on Valvular Heart DiseaseJ Thorac Cardiovasc Surg199410822072148041168
- MillaireAVan BelleEde GrootePLeroyODuclouxGObstruction of the left main coronary ostium due to an aortic vegetation: survival after early surgeryClin Infect Dis19962211921938825007
- SteckelbergJMMurphyJGBallardDEmboli in infective endocarditis: the prognostic value of echocardiographyAnn Intern Med199111486356402003709
- De CastroSMagniGBeniSRole of transthoracic and transesophageal echocardiography in predicting embolic events in patients with active infective endocarditis involving native cardiac valvesAm J Cardiol1997808103010349352973
- Snygg-MartinUGustafssonLRosengrenLCerebrovascular complications in patients with left-sided infective endocarditis are common: a prospective study using magnetic resonance imaging and neurochemical brain damage markersClin Infect Dis2008471233018491965
- ArnettENRobertsWCValve ring abscess in active infective endocarditis. Frequency, location, and clues to clinical diagnosis from the study of 95 necropsy patientsCirculation19765411401451277418
- OmariBShapiroSGinztonLPredictive risk factors for periannular extension of native valve endocarditis. Clinical and echocardiographic analysesChest1989966127312792582833
- DanielWGMüggeAMartinRPImprovement in the diagnosis of abscesses associated with endocarditis by transesophageal echocardiographyN Engl J Med1991324127958001997851
- AttiasDMessika-ZeitounDWolfMLepageLVahanianAAcute coronary syndrome in aortic infective endocarditisEur J Echocardiogr20089672772818579492
- HarinsteinMEMarroquinOCExternal coronary artery compression due to prosthetic valve bacterial endocarditisCatheter Cardiovasc Interv2014833E168E17024660223
- ManzanoMCVilacostaISan RománJASindrome coronario agudo en la endocarditis infecciosa. [Acute coronary syndrome in infective endocarditis]Rev Esp Cardiol20076012431 Spanish17288952
- KhanJAPanwarZMujtabaFShahKInfective endocarditis: a rare cause of acute coronary syndromeJ Coll Physicians Surg Pak201222424824922482383
- CrippsTGuvendikLCoronary artery compression caused by abscess formation in infective endocarditisInt J Cardiol1987141991023804511
- SchlaiferJDMartinTDHillJAKerenskyRACoronary artery obstruction caused by perivalvular abscess in aortic valve endocarditisAm Heart J199613124134168579047
- ZoffoliGGherliTPeriaortic valve abscess presenting as unstable anginaCirculation200511213e240e24116186428
- HortonCJJrNandaNCNekkantiRMukhtarOMcGiffinDProsthetic aortic valve abscess producing total right coronary artery occlusion: diagnosis by transesophageal three-dimensional echocardiographyEchocardiography200219539539812174203
- DeanJWKuoJWoodAJMyocardial infarction due to coronary artery compression by aortic root abscessInt J Cardiol19934121651678282441
- CowanSWFiserSMAlbrechtMFiferMVlahakesGJMadsenJCManagement of coronary artery compression caused by recurrent aortic root abscessJ Card Surg200823319519718435630
- WicklineCLGoliVDBuellJCCoronary artery narrowing due to extrinsic compression by myocardial abscessCathet Cardiovasc Diagn19912321211232070397
- ParasharaDKJacobsLEKotlerMNAngina caused by systolic compression of the left coronary artery as a result of pseudoaneurysm of the mitral-aortic intervalvular fibrosaAm Heart J199512924174217832123
- HoenBDuvalXInfective endocarditisN Engl J Med2013369878523964952
- BaddourLMWilsonWRBayerASInfective endocarditis: diagnosis, antimicrobial therapy, and management of complications: a statement for healthcare professionals from the Committee on rheumatic fever, endocarditis and Kawasaki diseaseCirculation200511123e394e43415956145
- MansurAJGrinbergMda LuzPLBellottiGThe complications of infective endocarditis. A reappraisal in the 1980sArch Intern Med199215212242824321456853
- DanielWGMüggeAMartinRPImprovement in the diagnosis of abscesses associated with endocarditis by transesophageal echocardiographyN Engl J Med1991324127958001997851
- ManzanoMCVilacostaISan RománJASindrome coronario agudo en la endocarditis infecciosa [Acute coronary syndrome in infective endocarditis]Rev Esp Cardiol20076012431 Spanish17288952
- NishimuraRACarabelloBAFaxonMDACC/AHA 2008 Guideline update on valvular heart disease: focused update on infective endocarditis: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic SurgeonsJ Am Coll Cardiol200852867668518702976
- HunterAJGirardDEThrombolytics in infectious endocarditis associated myocardial infarctionJ Emerg Med200121440140611728768
- LytleBWSabikJFBlackstoneEHSvenssonLGPetterssonGBCosgroveDM3rdReoperative cryopreserved root and ascending aorta replacement for acute aortic prosthetic valve endocarditisAnn Thorac Surg2002745S1754S1757 discussion S1792–S179912440658