Abstract
A 52-year-old woman presented with an 8-month history of epigastric pain, nausea, and weight loss. One year before, she was diagnosed with breast cancer. During the postoperative chemotherapy, she developed epigastric pain and nausea. As a result, she gradually lost 12 kg of her body weight. We performed upper gastrointestinal endoscopy, which revealed mild erosive gastritis. After the treatment with a proton pump inhibitor, her symptoms persisted. Before the admission, mild hypercalcemia was pointed out. Fluid replacement didn’t improve hypercalcemia. We assessed adrenocortical function, which showed that her serum cortisol and adrenocorticotropic hormone were decreased. Through loading tests, we established diagnosis of isolated adrenocorticotropic hormone deficiency. She was treated with hydrocortisone. Soon after the treatment, her serum calcium level returned to normal and her symptoms improved. In a case of hypercalcemia unresponsive to fluid replacement, we recommend ruling out adrenal insufficiency after excluding more common diseases which induce hypercalcemia.
Introduction
Adrenal insufficiency is defined by the impaired synthesis and release of adrenocortical hormones. It can be caused by diseases of the adrenal gland (primary), interference with adrenocorticotropic hormone (ACTH) secretion by the pituitary gland (secondary), or interference with corticotropin-releasing hormone secretion by the hypothalamus (tertiary). Isolated ACTH deficiency is classified as secondary adrenal insufficiency. In primary adrenocortical insufficiency, 5.5% of the patients present with hypercalcemia.Citation1 The proportion of secondary adrenal insufficiency is unknown. We report a case of isolated ACTH deficiency with hypercalcemia.
Case report
A 52-year-old Japanese woman presented with an 8-month history of epigastric pain, nausea, and weight loss. One year before, she was diagnosed with right breast cancer, which was resected with breast sparing surgery. She received postoperative chemotherapy using paclitaxel, fluorouracil, epirubicin, and cyclophosphamide. During the chemotherapy, she developed epigastric pain and nausea. As a result, she gradually lost 12 kg of her body weight over 8 months. Her oncologists consulted our department about her weight loss. At first, we performed upper gastrointestinal endoscopy, suggesting she had mild erosive gastritis. We treated her gastritis with a proton pump inhibitor, but her symptoms persisted. She was admitted because of her progressive dehydration. Before the admission, mild hypercalcemia (serum calcium 2.8 mmol/L, normal reference: 2.1–2.5 mmol/L; serum albumin 41 g/L, normal reference: 35–50 g/L) was pointed out by her oncologists. They performed contrast-enhanced computed tomography and whole body bone scintigraphy, and measured thyroid hormones (free T4 1.32 ng/dL, normal reference: 1.00–1.64 ng/dL; free T3 4.3 pg/mL, normal reference: 2.3–4.3 pg/mL; TSH 3.52 μIU/mL, normal reference: 0.45–4.95 μIU/mL), serum 1, 25-dihydroxyvitamin D (8 pg/mL, normal reference: 20–60 pg/mL), intact parathyroid hormone (9 pg/mL, normal reference: 10–65 pg/mL), and parathyroid-hormone-related protein-C (unmeasurable level, normal reference: less than 1.1 pmol/L). As a result, malignancy including bone metastasis, hyperthyroidism, hyperparathyroidism, vitamin D intoxication, and paraneoplastic syndrome were not detected. At this point, though dehydration was her oncologists’ tentative diagnosis, fluid replacement didn’t improve hypercalcemia. Considering that the appetite loss was too severe for mild hypercalcemia and the epigastric pain without remarkable endoscopic findings was refractory to the proton pump inhibitor, we suspected endocrine diseases as the cause of her symptoms and assessed adrenocortical function. As a result, her morning serum cortisol (0.12 μg/dL, normal reference: 6.2–19.4 μg/dL) and ACTH (1.2 pg/mL, normal reference: 7.2–63.3 pg/mL) were decreased remarkably. The anterior pituitary stimulation test revealed that the ACTH reactivity to corticotropin-releasing hormone was selectively impaired, while the other pituitary hormones were appropriately responded (). The result of an insulin tolerance test showed similar findings (). Further investigations revealed that magnetic resonance images showed she had no pituitary tumor () and anti-pituitary antibody was negative. We established a final diagnosis of isolated ACTH deficiency. She was treated with hydrocortisone 15 mg a day. Four days after the treatment, her serum calcium level returned to normal and her symptoms including epigastric pain and nausea improved.
Figure 1 Gadlinium-enhanced pituitary MRI (T1-weighted images).
Abbreviation: MRI, magnetic resonance imaging.
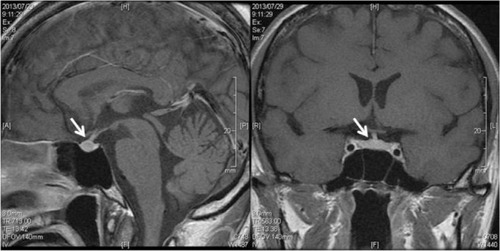
Table 1 Endocrinological findings. Basal endocrinological value and responses of pituitary hormones to intravenous injection of 100 μg corticotropin-releasing hormone, 100 μg growth hormone (GH)-releasing factor, 100 μg luteinizing hormone (LH)-releasing hormone, and 200 μg thyrotropin-releasing hormone
Table 2 Insulin tolerance test
Discussion
Isolated ACTH deficiency is a rare disorder, classified as secondary adrenocortical insufficiency and has various clinical presentations.Citation2,Citation3 Wide varieties of presenting symptoms were reported, including depressive disorder,Citation4 lower extremities’ motion abnormality,Citation5 and stress-induced cardiomyopathy.Citation6,Citation7 Compared with primary adrenocortical insufficiency, which has clinical presentations, skin pigmentation, and electrolyte abnormalities including hyponatremia and hyperkalemia, the symptoms and physical findings of secondary adrenocortical insufficiency are nonspecific and difficult to diagnose. Hypercalcemia was reported in 5.5% of primary adrenocortical insufficiency. The proportion of hypercalcemia is unknown in secondary adrenocortical insufficiency. Though the mechanism of hypercalcemia in adrenocortical insufficiency was unknown in detail, lack of serum cortisol is considered to be related to the increase of calcium reabsorption from renal tubules and release from bone.
We found three case reports about hypercalcemia caused by isolated ACTH deficiency. Grossman et al reported on a 64-year-old woman who presented with a 2-month history of nausea and weight loss.Citation8 Her corrected serum calcium level was 3.29 mmol/L and serum cortisol and ACTH were at abnormally low values. After the administration of hydrocortisone, hypercalcemia was improved. Kato et al reported on a 44-year-old female hemodialysis patient.Citation9 Her serum calcium level was elevated to 3.72 mmol/L for 3 months. Without glucocorticoid supplementation, her hypercalcemia was normalized. After the normalization, she was diagnosed as having isolated ACTH deficiency. Strachan et al reported on a 45-year-old male who presented with altered consciousness due to severe hypercalcemia (total serum calcium 3.56 mmol/L, albumin 35 g/L).Citation10 Initially, he was diagnosed as having hyperthyroidism. After extensive investigations, he also had isolated ACTH deficiency. Glucocorticoid administration resulted in dramatic improvement of his clinical state and serum calcium level.
In this case, regarding symptoms, appetite loss that was too severe for mild hypercalcemia and refractory epigastric pain without remarkable endoscopic gastrointestinal abnormalities were important clues to suspect metabolic or endocrine diseases. With regard to laboratory findings, except for the hypercalcemia, electrolyte abnormalities were very trivial. Compared with past case reports, the severity of hypercalcemia was so mild that it is quite reasonable to consider dehydration as the cause. It was a pitfall to make the diagnosis challenging. In a case of hypercalcemia unresponsive to fluid replacement, we recommend ruling out adrenocortical insufficiency including isolated ACTH deficiency after excluding more common diseases: malignancy, hyperparathyroidism, hyperthyroidism, and vitamin D intoxication.
Disclosure
The authors report no conflicts of interest in this work.
References
- NerupJAddison’s disease-clinical studies: A report for 108 casesActa Endocrinol (Copenh)19747611271414406578
- AndrioliMPecori GiraldiFCavagniniFIsolated corticotrophin deficiencyPituitary20069428929517077949
- HannonMJO’HalloranDJIsolated acquired ACTH deficiency and primary hypothyroidism: a short series and reviewPituitary201114435836119110973
- HiraoKKikawadaMOtoguroMElderly case of isolated ACTH deficiency presenting with depression and digestive symptomsNihon Ronen Igakkai Zasshi2007441117121 Japanese17337864
- OdagakiTNoguchiYFukuiTFlexion contractures of the legs as the initial manifestation of adrenocortical insufficiencyIntern Med200342871071312924497
- SakiharaSKageyamaKNigawaraTKidaniYSudaTAmpulla (Takotsubo) cardiomyopathy caused by secondary adrenal insufficiency in ACTH isolated deficiencyEndocr J200754463163617664847
- UkitaCMiyazakiHToyodaNKosakiANishikawaMIwasakaTTakotsubo cardiomyopathy during acute adrenal crisis due to isolated adrenocorticotropin deficiencyIntern Med200948534735219252360
- GrossmannMFullerPHunterATeedeHIsolated ACTH deficiency presenting with hypercalcaemiaClin Endocrinol (Oxf)200766460360417371483
- KatoAShinozakiSGogaTHishidaAIsolated adrenocorticotropic hormone deficiency presenting with hypercalcemia in a patient on long-term hemodialysisAm J Kidney Dis2003422E32E3612900850
- StrachanMWWalkerJDPatrickAWSevere hypercalcaemia secondary to isolated adrenocorticotrophic hormone deficiency and subacute thyroiditisAnn Clin Biochem200340Pt 329529712803848
