Abstract
We describe a case of bilateral consecutive superior ophthalmic vein thrombosis as a presenting feature in a patient previously not known to have systemic lupus erythematosus (SLE). A 68-year-old African–American female presented with decreased vision in right eye, mild right orbital tenderness, and frontotemporal headache of 3 days duration. MRI of the orbits confirmed thrombosis of the right superior ophthalmic vein without extension into the cavernous sinus. Sequential MRI at 1 month showed interval improvement of the right superior ophthalmic vein thrombosis and a new thrombosis in the left superior ophthalmic vein. Renal biopsy revealed granular membranous and mesangial deposits of IgG, IgA, IgM, C3, and C1q and confirmed the diagnosis of SLE.
Introduction
Isolated superior ophthalmic vein thrombosis (SOVT) is a rare condition often caused by infections of the midface, Graves’ ophthalmopathy, orbital pseudotumor, vascular malformations, and Tolosa–Hunt syndrome. Orbital congestion, proptosis, chemosis, and ophthalmoplegia are seen in patients with superior ophthalmic vein (SOV) occlusion and thrombosis.Citation1 MRI and MRV confirm the diagnosis of SOV thrombosisCitation2 and exclude the presence of carotid-cavernous sinus fistula, cavernous sinus thrombosis, and sino-orbital infection.
Ocular features are common (34.6%) in systemic lupus erythematosus (SLE), and lupus retinopathyCitation3 is most frequent. Other ocular manifestations include lid involvement, mucocutaneous involvement, secondary Sjögren’s syndrome, choroidopathy, and neuro-ophthalmic disorders. SOVT is extremely rare in SLE.
In this report, we describe an isolated bilateral consecutive SOVT as a presenting feature in a patient previously not known to have SLE.
Case report
A 68-year-old African–American woman presented with nausea, vomiting, and frontotemporal headaches of 3 days duration. Associated symptoms included decreased vision in her right eye and mild right orbital tenderness. Her medical history included hypertension, hyperlipidemia, coronary artery disease, gastroesophageal reflux disease, and goiter status post left lobectomy. Department of Ophthalmology was consulted for evaluation of decreased vision and an abnormal CT scan of the head.
Best-corrected visual acuity (BCVA) was 20/80 in the right eye and 20/20 in the left eye. Visual fields were full to confrontation. Her intraocular pressure was 30 mm Hg in both eyes. Horizontal eye movements were full, except for painful restriction of up and down gaze of the right eye (). Pupils demonstrated 3+ reactivity bilaterally, and there was no relative afferent pupillary defect. Exophthalmometry with a base of 119 mm was 24 mm in the right eye and 22 mm in the left eye. Color vision was normal in both eyes. External examination revealed right superior orbital fullness () with mild tenderness on palpation. Anterior segment examination was unremarkable. Fundus examination was remarkable for increased cup-to-disc (0.6) ratio in both eyes. There were no choroidal folds or vascular congestion or disc edema.
Figure 1 Clinical picture and H & E staining.
Abbreviation: H&E, hematoxylin and eosin.
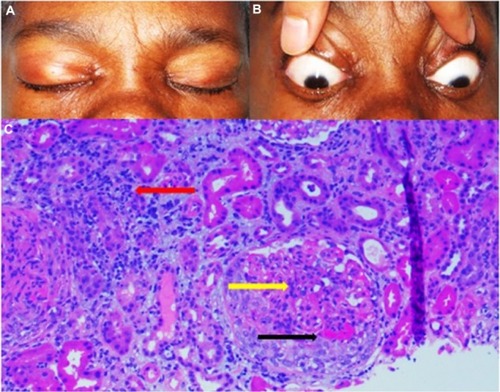
CT scan of the head showed a hyperdensity within the right SOV. MRI of the orbits confirmed thrombosis of the right SOV without extension into the cavernous sinus (). Diagnosis of SLE was confirmed on hematological examination (ANA [antinuclear antibody], anti-Smith antibody and anti-ds DNA were positive) and renal biopsy () showing histopathological/immunological changes of SLE (granular membranous and mesangial deposits [2+ to 3+] of IgG, IgA, IgM, C3, and C1q).
Figure 2 MRI of orbits.
Abbreviation: SOVT, superior ophthalmic vein thrombosis; MRI, magnetic resonance imaging.
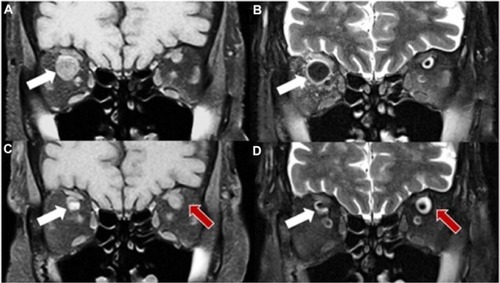
The patient’s orbital fullness and decreased vision improved dramatically after 2 days of steroid (intravenous methylprednisolone 40 mg three times a day) and anticoagulant (intravenous heparin) treatment. Sequential MRI at 1 month showed interval improvement of the right SOVT and a new thrombosis in the left SOV ().
Discussion
SOVT (a rare secondary vascular phenomena) is seen in hypercoagulable states (use of oral contraceptive pills, pregnancy, thrombocytosis), infectious diseases (infectious sinusitis, orbital cellulitis), inflammatory diseases (SLE, Behçet syndrome, sarcoidosis, idiopathic orbital inflammation), neoplasms (leukemia, lymphoma, meningioma), trauma, and carotid-cavernous fistula.Citation4 SOVT may or may not be associated with cavernous sinus thrombosis.Citation5 Congestive signs such as proptosis, ophthalmoplegia, papilledema, chemosis, intraocular hypertension, and retinal venous congestion are usually seen with SOVT. However, thrombosis of orbital veins without extension into the cavernous sinus is rareCitation5 and anticoagulation treatment is consideredCitation4 to obliterate thrombosis.
Isolated SOVT without cavernous sinus involvement is extremely rare. There is a report of a female who developed bilateral SOVTCitation6 with associated peripheral retinal hemorrhages, on oral contraceptive pills. Idrees et al,Citation7 reported recently a case of bilateral SOV thrombosis secondary to antiphospholipid syndrome in a female with good vision along with associated disc swelling and proptosis. Our patient had good vision on presentation, with minimal orbital congestive signs; BCVA improved to 20/20 after treatment with anticoagulation and steroids.
In conclusion, we report a rare case of bilateral consecutive SOVT as a presenting feature of SLE (confirmed by MRI and histopathology). Early definitive diagnosis and aggressive treatment with steroids and anticoagulants usually results in resolution of SOVT and restoration of vision.
Disclosure
No financial support was received for this submission. The authors report no conflicts of interest in this work.
References
- Duke-ElderSSystem of OphthalmologyXLondon, UKHenry Kimpton1974816819
- LimLHScawnRLWhippleKMSpontaneous superior ophthalmic vein thrombosis: a rare entity with potentially devastating consequencesEye20142834835124357838
- EL-ShereefRRMohamedASHamdyLOcular manifestation of systemic lupus erythematosusRheumatol Int2013331637164222202921
- ShinderROellersPEsmaeliBSuperior ophthalmic vein thrombosis in a patient with chronic myeloid leukemia receiving antifibrinolytic and thrombopoietin receptor agonist therapyJ Ocul Pharmacol Ther20102629329620565317
- WalkerJCSandhuAPietrisGSeptic superior ophthalmic vein thrombosisClin Exp Ophthalmol200230144146
- MichaelidesMAclimandosWBilateral superior ophthalmic vein thrombosis in a young womanActa Ophthalmol Scand2003811889012631033
- IdreesZDooleyIJacksonASimultaneous isolated bilateral superior orbital vein thrombosis as a presenting feature of antiphospholipid syndromeOrbit201433321421624568210
