Abstract
We report a case of bilateral orbital hemorrhage as a complication of peribulbar anesthesia in a 78 year old man. Initially, unilateral orbital hemorrhage occurred but quickly spread to the contralateral side. Neuroophthalmological assessment revealed a proptosed tense globe with normal retinovascular findings. Visual acuity was adversely affected and this was conservatively managed with no lasting ophthalmic sequela. This patient’s case was reported as it illustrates an unusual complication of bilateral spread of orbital hemorrhage secondary to peribulbar anesthesia. It highlights how early ophthalmic assessment can ensure a good visual outcome in the setting of appropriate ophthalmic monitoring. The mechanisms of orbital hemorrhage spread and appropriate management options are discussed.
Introduction
Retrobulbar hematoma is an uncommon complication of retrobulbar/peribulbar block, which requires urgent decompression to prevent blindness from raised intraorbital pressure.Citation1 Furthermore, bilateral periorbital hemorrhage, as a complication of retrobulbar hematoma, is exceedingly rare.Citation2 To the authors’ knowledge, such a complication resulting from this form of anesthesia has not been previously reported in the current literature.
Case report
A 78-year-old man was scheduled to undergo cataract surgery in the right eye and intraocular lens insertion, but developed a right-sided retrobulbar hemorrhage followed by bilateral periorbital hematoma secondary to right peribulbar anesthesia. This occurred within 1–2 minutes following a peribulbar injection of 6 mL of 50% lignocaine (1%) with 1:100,000 adrenaline and 50% bupivicane with 1:200,000 adrenaline, plus hyalase. This technique included positioning the bevel of the needle sufficiently below the globe to avoid rupturing of the globe, ie, along the inferior orbital rim, and aspirating the syringe prior to injecting to avoid an intravenous injection.
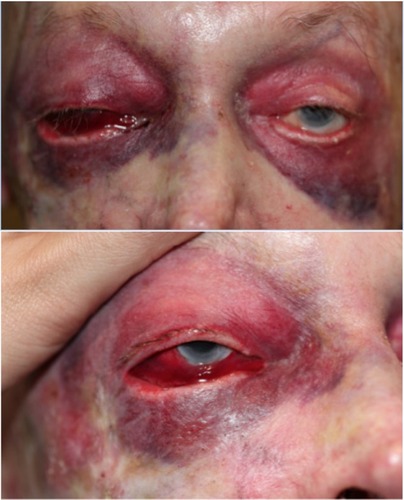
The diagnosis of retrobulbar hemorrhage is made by the presence of proptosis, a fixed dilated pupil, ophthalmoplegia, decreasing visual acuity, and a winking or ischemic optic nerve head.Citation3–Citation5 On examination, proptosis, a tense globe, and a normal optic disc with a normal pulsating central retinal artery were noted (). Marked subconjunctival hemorrhage without a posterior limit on the right side, right-sided proptosis, and bilateral periorbital ecchymosis were noted. Visual acuity, pain, ophthalmoplegia, and pupils could not be assessed accurately due to the anesthetic and mydriatic agents administered in preparation for cataract surgery.
Right visual acuity was to count fingers at 1.5 m after 3 hours of injection, although this was likely related to the local anesthetic still dissipating. The patient was admitted for investigations and monitoring, as in all cases of retrobulbar hemorrhage.Citation5 Conservative management was deemed appropriate based on the stability of intraocular pressure measurements and right visual acuity. Visual fields were grossly intact throughout. International normalized ratio, activated partial thrombin time, and platelets were all found to be normal. Visual field deficits had resolved by the following morning when facial photographs were taken ().
Medical history was found to be relatively unremarkable with no hypertension, hematological conditions, paranasal sinus surgery, or facial injury. Although he had no previous diagnosis of thrombotic or bleeding disorders, a history of one previous episode of significant bleeding following minimal surgery was elicited on extensive questioning following the incident. The month prior, he had been admitted for unremitting hemorrhage following excision of multiple basal cell carcinomas. This urgent episode was treated conservatively with compression, bed elevation, and ice packs and monitored until the following morning, when visual acuity and fields had returned to baseline. No abnormal blood test results were observed at any point, and the patient was not taking any anticoagulant medication.
On review after 2 weeks, the patient was found to have fully recovered with no persistent symptoms. On examination, intraocular pressure and visual acuity was normal, and residual ecchymosis was still present. He was rebooked for cataract surgery with a sub-Tenon anesthetic block, which was successful and uneventful. There was also an unremarkable review at 4 months, and a preexisting right-sided ectropion was found to have progressed but was asymptomatic ().
Patient consent was obtained for the purposes of facial photography and de-identified publication. No ethics approval was needed for this case report.
Discussion
We have presented a case of a 78-year-old man who experienced retrobulbar hemorrhage following peribulbar anesthetic injection for phacoemulsification, which subsequently spread to the contralateral eye. This was resolved with conservative management, and the patient later underwent successful lens extraction and intraocular lens insertion.
Successful anesthetic block for the purposes of cataract surgery requires adequate anesthesia and usually akinesia.Citation5,Citation6 A Cochrane Review concluded that there was little difference between anesthesic options with respect to akinesia, development of severe complications, patient acceptability, and failure rates requiring further injections.Citation6 Complications can include ecchymosis, retrobulbar hemorrhage, globe perforation, cranial nerve palsy, and raised intraocular pressure resulting in central retinal artery occlusion and transitory or permanent vision loss and brain stem anesthesia.Citation5–Citation9 Fortunately, these complications are exceedingly rare.Citation6–Citation12 Other documented causes of nontraumatic retrobulbar hemorrhage include vascular malformations, increased venous pressure (during childbirth or Valsalva maneuvres), coagulopathies, orbital lesions, infection, and interestingly scurvy.Citation13,Citation14
Both peribulbar anesthetic injection and topical anesthesia are well established as safe and effective methods to use prior to cataract surgery.Citation6–Citation12 It has been established that when comparing anesthetic options for cataract surgery, a variety of factors must be considered and the optimal option is situationally dependent.Citation4,Citation7 The use of nonsteroidal anti-inflammatory drug medications, aspirin, anticoagulants, and certain supplements, such as St John’s Wort, should be withheld 2 weeks prior to cataract surgery to reduce the risk of bleeding-related complications.Citation4 A 2012 meta-analysis established that topical anesthesia reduces the risk of injection-related complications, such as retrobulbar hemorrhage and chemosis and alleviates patient anxiety regarding injections.Citation7 However, it does not provide comparable analgesia and does not increase intraoperative difficulty, despite increased eye motility.Citation7
Many of these complications are a result of the confined space that is the orbit. The floor, roof, medial and lateral walls, and anteriorly the orbital septum limit the orbital cavity.Citation13,Citation15 This compartment can contain hemorrhages of various origin and they can theoretically spread in multiple ways. The most likely explanation of the spread of hemorrhage to the contralateral eye in this case is either via the loose areolar tissue of the scalp or possibly retroseptal spread.Citation16
The scalp consists of skin, connective tissue, aponeurosis, loose areolar tissue, and pericranium (periosteum of the skull). The loose areolar tissue provides a subaponeurotic potential space within which bleeding can spread. This could potentially spread hemorrhage from one eye to another as this tissue extends beneath orbicularis oculi but could penetrate dehiscences in the contralateral orbital septum.Citation17,Citation18
Retroseptally, the most likely source of spread would be emissary veins in the medial wall allowing spread via the ethmoid cavities or potentially even the cavernous sinus, which is valveless.
The ideal management of retrobulbar hemorrhage is not fully established.Citation18 Management should, however, be done in consultation with an ophthalmologist and involves a thorough clinical assessment and monitoring for deterioration.Citation5,Citation8,Citation19,Citation20 Imaging can be used to confirm diagnosis, though may unnecessarily delay urgent treatment, as retrobulbar hemorrhages can often be diagnosed clinically.Citation4,Citation5
Mild retrobulbar hemorrhages can be managed conservatively.Citation2,Citation8,Citation21–Citation23 In these circumstances, certain factors ought to be optimized in order to reduce the risk of further hemorrhage:Citation8,Citation17,Citation21
Patients should be advised to avoid coughing or straining.
The bed head should be elevated at least 45°.
Blood pressure and coagulopathies should be normalized.
Ice packs may be of benefit in reducing blood flow and edema.
Intraocular pressure-lowering medications and high-dose systemic corticosteroids may also play a role.
In the circumstances where conservative management is insufficient to preserve eyesight, surgical intervention may be required.Citation22 This initially involves a lateral canthotomy with an inferior cantholysis.Citation2,Citation3 A canthotomy is an incision of the lateral canthal tendon, and cantholysis is the disinsertion of the canthal tendon from the orbital rim. The aforementioned procedure involves cutting the lateral canthal tendon in a horizontal plane to the orbital rim and dividing the inferior limb until it releases the lower lid tension.
In the event that this does not sufficiently reduce pressure for perfusion to return, the following steps may be performed:Citation2,Citation3,Citation17
Disinsertion of the superior portion of the canthal tendon.
The orbital septum may be further surgically detached from the orbital rim.
A surgical exploration of the lateral wall, followed by the orbital floor and medial wall, if necessary, will definitively relieve pressure within the orbital cavity in the most extreme cases.
However, orbital decompression and optic nerve fenestration are not yet established as efficacious interventions by current data.Citation8,Citation19
Conclusion
In conclusion, nontraumatic bilateral spread of retrobulbar hemorrhage has not been discussed in the current literature. We have presented such a case and speculated on the possible mechanisms of pathogenesis and potential treatments. Important issues raised by this case include the following:
Practitioners ought to delve extensively into bleeding history prior to undergoing invasive procedures with potentially significant complications.
Less-invasive anesthetic blocks, such as topical anesthesia or sub-Tenon anesthetic blocks, ought to be considered in such cases.
Retrobulbar hemorrhage can be managed conservatively in some cases but lateral canthotomy can be a relatively safe, urgent intervention.
Disclosure
The authors report no conflicts of interest in this work.
References
- KallioHPaloheimoMMaunukselaELHaemorrhage and risk factors associated with retrobulbar/peribulbar block: a prospective study in 1383 patientsBr J Anaesth20008570871111094585
- RoseGEVerityDHAcute presentation of vascular disease within the orbit-a descriptive synopsis of mechanismsEye (Lond)201327329930723370421
- LimaVBurtBLeibovitchIOrbital Compartment Syndrome: the ophthalmic surgical emergencySurv Ophthalmol200954444144919539832
- HislopWDuttonGDouglasPTreatment of retrobulbar haemorrhage in accident and emergency departmentsBr J Oral Maxillofac Surg1996342892928866062
- HayterJSugarAAn orbital observation chartBr J Oral Maxillofac Surg19912977792049359
- AlhassanMBKyariFEjereHOPeribulbar versus retrobulbar anaesthesia for cataract surgeryAnesth Analg20081076208919020164
- McCombeMHeriotWPenetrating ocular injury following local anaesthesiaAust N Z J Ophthalmol199523133367619453
- SmithRCataract extraction without retrobulbar anaesthetic injectionBr J Ophthalmol19907442052072337544
- KongsapPSuperior subconjctival anesthesia versus retrobulbar anesthesia for manual small-incision cataract surgery in a residency training program: a randomized controlled trialClin Ophthalmol201261981198623233795
- SchraderWFSchargusMSchneiderEJosifovaTRisks and sequelae of scleral perforation during peribulbar or retrobulbar anaesthesiaJ Cataract Refractive Surg201036885889
- ZhaoLQZhuHZhaoPQWuQRHuYQTopical anesthesia versus regional anesthesia for cataract surgery: a meta-analysis of randomized controlled trialsAm Acad Opthalmol2012119659667
- GrossACestariDOptic neuropathy following retrobulbar injection: a reviewSemin Ophthalmol2014295–643443925325871
- McNabANontraumatic orbital haemorrhageSurv Ophthalmol20145916618424359805
- SloanBKulwinDRKerstenRCScurvy causing bilateral orbital haemorrhageArch Ophthalmol1999117684284310369606
- NouvellonEL’HermiteJChaumeronAMedial canthus episcleral (Sub-Tenon) single injection blockOphthalmic Reg Anesth2004100370374
- BronATripathiRTripathiBWolff’s Anatomy of the Eye and Orbit8th edLondonChapman & Hall Medical1998
- SinnatambyCSLast’s Anatomy12th edNew YorkChurchill Livingstone2011
- KarabekirHSGocmen-MasNEmelEOcular and periocular injuries associated with an isolated orbital fracture depending on a blunt cranial trauma: anatomical and surgical aspectsJ Craniomaxillo Surg2012407e189e193
- OrdRAAwtyMDPourSBilateral retrobulbar haemorrhage: a short case reportBr J Maxillofacial Surg198624116
- HanJKCaugheyRJGrossCWNewmanSManagement of retrobulbar hematomaAm J Rhinol200822552252418954513
- McClenaghanFEzraDHolmesSMechanisms and management of vision loss following orbital and facial traumaCurr Opin Ophthalmol20112242643121730843
- PopatHDoylePTDaviesSJBlindness following retrobulbar haemorrhage – it can be preventedBr J Oral Maxillofacial Surg2007452163164
- MachadoRASilveiraRLBorgesHOFilhoAMde OliveiraMGRetrobulbar hemorrhages: a case reportJ Contemp Dent Pract20067213013616685304