Abstract
Introduction
Scleritis and peripheral ulcerative keratitis are ocular manifestations found in many inflammations and infections. Therefore, their association should prompt a search for inflammatory or infectious causes that may be life-threatening, especially in the context of AIDS due to HIV infection.
Findings
We report the case of a 37-year-old female, first seen in 2011 with a nodular scleritis in the right eye and a peripheral ulcerative keratitis, a necrotizing scleritis, and a granulomatous anterior uveitis in the left eye, in the context of chronic polyarthropathies that had evolved over 6 months. The patient was diagnosed with AIDS (HIV) in 2008 and was on antiretroviral therapy for the past 2 years. Ophthalmic workup was negative for opportunistic infections and potential causes of scleritis and peripheral ulcerative keratitis, and the patient was unresponsive to topical antibacterial and anti-inflammatory treatment. Ocular lesion resolution and articular swelling improvement was observed less than 6 weeks after sulfasalazine treatment. Based on American College of Rheumatology/European League Against Rheumatism classification criteria, and considering the good response to the treatment (sulfasalazine), diagnosis of rheumatoid arthritis was made in the absence of confirmatory lab tests results.
Conclusion
In the context of ocular manifestations associated with polyarthropathies, coexisting pathologies should be considered. Diagnostic workup of chronic inflammatory rheumatism should be carried out, even in the context of HIV/AIDS.
Introduction
Many reports have recently described an association between chronic inflammatory rheumatism and HIV infection in Africa.Citation1–Citation10 More specifically, although the relationship between rheumatoid arthritis (RA) and HIV/AIDS infection, both life-threatening diseases, is possible, this association is rare.Citation11 These diseases can affect different systems and can particularly lead to ocular involvement. Ocular lesions in RA and HIV/AIDS infection are well documented,Citation12,Citation13 although ocular manifestations in a combination of both diseases have not been described in the past years. We therefore report the case of a 37-year-old HIV-positive female, who exhibited an association of nodular scleritis, peripheral ulcerative keratitis, and anterior uveitis in the context of chronic polyarthropathies. To our knowledge, the coexistence of these types of ocular lesions in a similar context has not been reported previously. Written informed consent was obtained from the patient to publish this report and any accompanying images. Permission from the institutional review board of the Université des Montagnes was also obtained.
Findings
A 37-year-old female presented to an eye unit in February 2011 with a 6-week history of significant ocular discomfort, associated with bilateral red eyes and a nodule in the right one.
Past medical history revealed significant polyarticular pain with joint swelling over the past 6 months (both shoulders, elbows, and wrists, interphalangeal joints of two fingers of the left hand, both knees, and both ankles). The patient, diagnosed as positive for HIV-1 group M in 2008, was on antiretroviral treatment and sulfonamides since 2009. At the moment of consultation, she was at clinical stage 2 of HIV/AIDS (according to the World Health Organization).
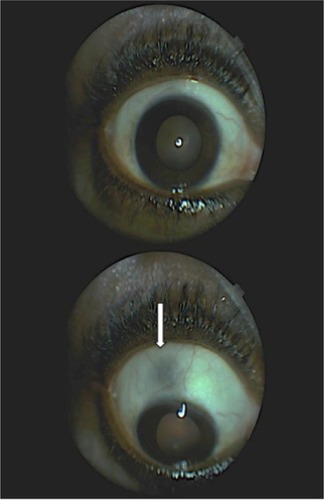
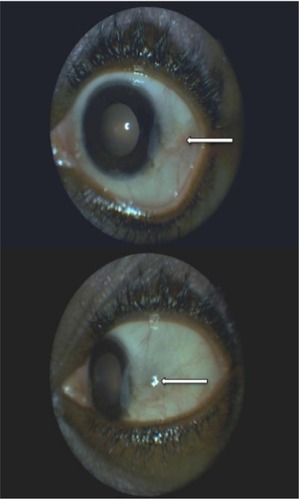
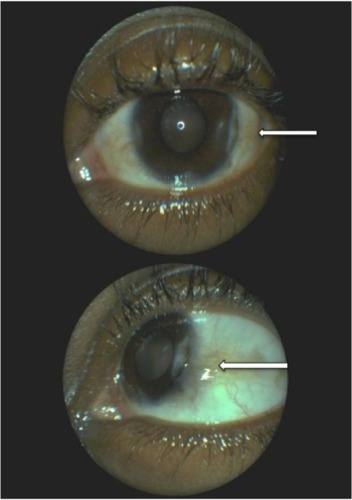
Based on ocular examination, best-corrected visual acuities were 20/20 and 20/50 in the right and left eye, respectively. Slit-lamp examination of the right eye showed a superior nodular scleritis surrounded by mild inflammation, while in the left eye, a peripheral (temporoinferior) corneal ulceration associated with scleritis and granulomatous anterior uveitis (presence of cells and flare and absence of posterior synechiae in the anterior chamber) was observed ( and ). Intraocular pressure was 15 mmHg, and the fundus examination was normal in both eyes.
Figure 1 Right eye lesion before treatment with sulfasalazine.
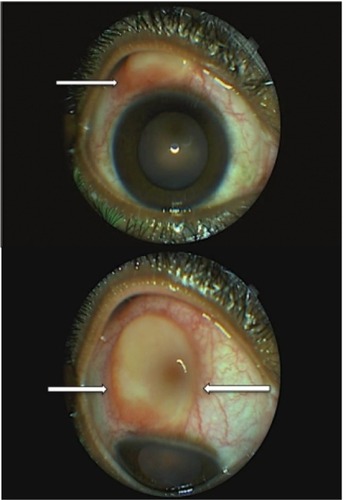
Figure 2 Left eye before treatment with sulfasalazine (use of fluorescein).
A combination of topical (ciprofloxacin and indomethacin eye drops) and systemic treatment (oral ibuprofen) was started for 3 weeks, with no improvement on the clinical signs.
Diagnostic tests revealed an inflammatory syndrome and a CD4 count of 103/µL. Systemic investigation was negative for syphilis, tuberculosis, and hepatitis B and C. Diagnostic workup of rheumatismal diseases included laboratory tests and biopsy of affected tissues. Testing for rheumatoid factor, Waaler–Rose reaction, antinuclear antibodies (ANA), anti-native DNA antibodies, antineutrophil cytoplasmic antibodies (ANCA), and anti–cyclic citrullinated peptide antibodies (anti-CCP) was negative. The assessment of the biopsied scleral nodule revealed an inflammatory lesion (vasculoexudative phase).
The patient also consulted a rheumatologist, and a diagnosis of RA was made based on the clinical findings according to American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) classification criteria (patient’s score >6).
Treatment with sulfasalazine (500 mg/d) was started, and was progressively increased (1,500 mg daily) over 3 weeks. Regression of symptoms, and ocular and articular signs was observed within 15 days ().
Figure 3 Left eye lesion 1 month after initiating the treatment with sulfasalazine.
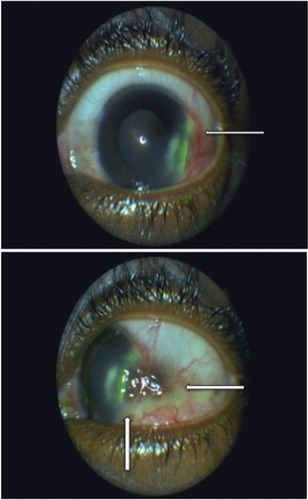
The patient was monitored every month until November 2011. Sulfasalazine treatment was stopped in September 2011, and no recurrence of clinical signs was observed at the 8-month follow-up (best visual acuity of both eyes: 20/20). The clinical examination revealed an absence of scleritis in the right eye and a disappearance of intraocular inflammation associated to a temporal degeneration of the perilimbal conjunctiva in the left eye ( and ).
Discussion
In the literature, many authors have reported associations of multiple forms of chronic inflammatory rheumatism and HIV/AIDS disease in black African patients.Citation1–Citation10 However, the physiopathogenic mechanism is still unknown.
Ocular manifestations such as scleritis and peripheral ulcerative keratitis can be related to local or systemic infectious or to inflammatory causes.Citation12 However, according to the literature, these types of ocular lesions are not specific to HIV/AIDS infection and/or to antiretroviral treatment. Scleritis is an uncommon condition that predominantly affects females. The Watson and Hayreh classification of scleritis distinguishes two forms: anterior (diffuse, nodular, and necrotizing) and posterior forms.Citation14 Much research, focused on the pathogenesis of scleritis, has suggested a link with inflammatory process mediated by Th cells.Citation15 In the presence of anterior diffuse and nodular scleritis, systemic causes are found in 40%–50%, and infectious etiologies, in 7% of cases,Citation16,Citation17 whereas in necrotizing scleritis, systemic affections are found in 50%–80% of cases.Citation16 In our case, the anterior nodular scleritis was an inflammatory process according to the pathologist (figure of the biopsied lesion not available).
RA and granulomatosis with polyangiitis are systemic diseases mainly associated with scleritis.Citation16,Citation18 Complications of anterior scleritis include anterior uveitis, peripheral ulcerative keratitis, cataract, or glaucoma. Sainz de la Maza et al,Citation19 reported that patients with scleritis also had anterior uveitis, cataract, peripheral ulcerative keratitis, and glaucoma in 42%, 17%, 14%, and 13% of cases, respectively. Peripheral ulcerative keratitis is an ocular disease that occurs less often than scleritis. It affects both sexes equally. Peripheral ulcerative keratitis is frequently associated with necrotizing scleritis and is bilateral in more than 40% of cases.Citation20 Tauber et al,Citation21 in their study, reported an association of ulcerative keratitis and RA in 34% of patients. In addition, corneal involvement was described as the first manifestation of RA.
According to Foster et al,Citation22 mortality rate at 10 years in patients affected by RA associated with peripheral ulcerative keratitis and necrotizing scleritis could be estimated at 50%. The pathogenesis of peripheral ulcerative keratitis is still unknown. However, one hypothesis is that stromal destruction could be due to the collagenases and other proteases produced by the immune cells (neutrophils and macrophages). In addition, the presence of proinflammatory cytokines induces the release of metalloproteinases by stromal keratocytes, leading to the destruction of the cornea.Citation23
Clinical, radiological, and biological investigations are similar in scleritis and peripheral ulcerative keratitis presentation. Tuberculosis, syphilis, and Lyme disease are the most frequent systemic infections related to these ocular manifestations, whereas RA and granulomatosis with polyangiitis appear to be the most common inflammations.Citation12 According to the type of ocular lesions described in our case, the patient was not worked up for Sjögren syndrome (anti-SSA and anti-SSB antibodies), which is known as a disease often associated to RA.Citation24
In accordance with our patient’s immunological status due to HIV infection, a workup of opportunistic infections in reference to ocular manifestations was first carried out, and all results were negative. Although the systemic investigation of rheumatismal affections was negative, the diagnosis of RA was retained in accordance to ACR/EULAR classification criteria (2010).Citation25 Moreover, good response to the trial treatment (sulfasalazine) was an additional contribution to this diagnosis. RA is described as an autoimmune disease characterized by chronic inflammation and articular destruction. It is the most frequent inflammatory arthritis found in females. Predisposing genetic factors of RA have been reported, although its pathophysiologic mechanism is poorly understood human leukocyte antigen (HLA)-DR. Moreover, inflammation in RA is characterized by high erythrocyte sedimentation rate and/or C-reactive protein, the presence of rheumatoid factors, and more specifically, a high level of anti-CCP, although the diagnosis of RA, is primarily based on clinical features (existence of seronegative forms).Citation26,Citation27 However, according to the literature, the association of RA with HIV infection is quite rare.Citation11 Moreover, HIV infection may lead to anti-CCP antibody positivity, and RA to false-positive HIV serology. In our case, the search for anti-CCP antibodies was negative, and the diagnosis of HIV was made few years earlier to the actual clinical presentation.
Therapy for RA combines the use of anti-inflammatory and immunosuppressive drugs. Local and systemic anti-inflammatory drugs essentially act on the acute phase by stopping the inflammation (nonsteroidal anti-inflammatory, corticosteroids). Systemic disease modifying antirheumatic drugs (DMARDs),Citation28 more often combined to anti-inflammatory ones, slow down, or even stop the clinical course of the disease. There are two types of DMARDs, conventional ones (cyclosporine, cyclophosphamide, gold injections, hydroxychloroquine, leflunomide, methotrexate, mycophenolate, sulfasalazine) and biological therapies (anti-TNF [tumour necrosis factor] drugs). DMARDs should be started as soon as the diagnosis of RA is made.Citation29 Many authors evoke the complexity of therapeutic management in chronic inflammatory rheumatisms due to numerous side effects and potential complications (myelosuppression, renal and liver toxicity, skin rash, gastrointestinal disturbance, infections).Citation10,Citation28 Thus, therapy with DMARDs should be initiated by rheumatologists. Moreover, patients treated with these drugs should be monitored regularly, and any complications seen should be the motive for stopping the treatment.Citation28
In this case, the treatment choice of the rheumatologist was sulfasalazine, and a favorable response was obtained within few weeks. Sulfasalazine is a well-known treatment for RA. Its efficacy has been demonstrated in several clinical trials.Citation30 It acts by inhibiting arachidonic acid synthesis (anti-inflammatory action), and it also has an immunosuppressive action with a poorly understood mechanism. It is well tolerated and remains the first line treatment in many countries. Its main contraindication is salicylate hypersensitivity. It can be used alone or in association with immunosuppressive drugs.Citation29,Citation30 Although, there is little evidence to recommend the use of DMARDs when RA coexists with HIV/AIDS infection,Citation11 sulfasalazine was well-tolerated by our patient with a complete recovery of ocular lesions (duration of treatment: 6 months).
Conclusion
We have described the clinical course of ocular manifestations (nodular scleritis, peripheral ulcerative keratitis, and anterior uveitis) in the context of polyarthropathies in a HIV-positive female. In this case report, RA diagnosis was based on ACR/EULAR classification criteria. Coexisting pathologies should always be considered, and diagnosis of chronic inflammatory rheumatism workup combined to a complete ocular examination should be made, even in the context of HIV disease.
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- SteinMDavisPHIV and arthritis – causal or casual acquaintances?J Rheumatol19891610128712902681756
- BileckotRMouayaAMakuwaMPrevalence and clinical presentations of arthritis in HIV-positive patients seen at a rheumatology department in Congo-BrazzavilleRev Rhum Eng Ed19986510549554
- NjobvuPMcGillPKerrHJellisJPobeeJSpondyloarthropathy and human immunodeficiency virus infection in ZambiaJ Rheumatol1998258155315599712100
- SteinCMDavisPArthritis associated with HIV infection in ZimbabweJ Rheumatol19962335065118832993
- NjobvuPMcGillPHuman immunodeficiency virus related reactive arthritis in ZambiaJ Rheumatol20053271299130415996068
- ChinniahKModyGMBhimmaRAdhikariMArthritis in association with human immunodeficiency virus infection in Black African children: causal or coincidental?Rheumatology (Oxford)20054491592015827039
- NjobvuPMcGillPSoft tissue rheumatic lesions and HIV infection in ZambiansJ Rheumatol200633122493249717143983
- EkwomPEOyooGOAmayoEOMurilithiIMPrevalence and characteristics of articular manifestations in human immunodeficiency virus infectionEast Afr Med J2010871040841423057274
- NtsibaHNgandeu-SingwéMMakita-BagamboulaCYalaFLes arthrites liées au virus de l’immunodéficience humaine au Congo Brazzaville [Human immunodeficiency virus associated arthritis in Congo Brazzaville]Médecine et Maladies Infectieuses20073711758761 French17150323
- TiklyMNjobvuPMcGillPSpondyloarthritis in sub-Saharan AfricaCurr Rheumatol Rep20141642124744085
- CunhaBMMotaLMPileggiGSSafeIPLacerdaMVHIV/AIDS and rheumatoid arthritisAutoimmun Rev201514539640025578483
- GalorAThorneJEScleritis and peripheral ulcerative keratitisRheum Dis Clin North Am200733483585418037120
- GovenderPHansrajRNaidooKSVisserLOcular manifestations of HIV/AIDS: a literature reviewS Afr Optom20117028188
- WatsonPGHayrehSSScleritis and episcleritisBr J Ophthalmol19766031631911268179
- FongLPSainz de la MazaMRiceBAKupfermanAEFosterCSImmunopathology of scleritisOphthalmology19919844724791828871
- SchwamBScleritisKrachmerJMannisMHollandECornea and External Disease: Clinical Diagnosis and Management2St Louis, MOMosby199714791491
- AkpekEKThorneJEQaziFADoDVJabsDAEvaluation of patients with scleritis for systemic diseaseOphthalmology2004111350150615019326
- TuftSJWatsonPGProgression of scleral diseaseOphthalmology19919844674712052300
- Sainz de la MazaMJabburNSFosterCSSeverity of scleritis and episcleritisOphthalmology199410123893968115160
- Sainz de la MazaMFosterCSJabburNSBaltatzisSOcular characteristics and disease associations in scleritis-associated peripheral keratopathyArch Ophthalmol20021201151911786052
- TauberJSainz de la MazaMHoang-XuanTFosterCSAn analysis of therapeutic decision making regarding immunosuppressive chemotherapy for peripheral ulcerative keratitisCornea19909166732297997
- FosterCSForstotSLWilsonLAMortality rate in rheumatoid arthritis patients developing necrotizing scleritis or peripheral ulcerative keratitis: effects of systemic immune suppressionOphthalmology198491125312636514289
- DanaMQianYHamrahPTwenty-five-year panorama of corneal immunology: emerging concepts in the immunopathogenesis of microbial keratitis, peripheral ulcerative keratitis, and corneal transplant rejectionCornea200019562564311009315
- HeJDingYFengMCharacteristics of Sjogren syndrome in rheumatoid arthritisRheumatology (Oxford)20135261084108923382356
- AletahaDNeogiTSilmanAJ2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiativeArthritis Rheum20106292569258120872595
- RozinAPHasinTToledanoKGuralnikLBalbir-GurmanASeronegative polyarthritis as severe systemic diseaseNeth J Med201068623624120558853
- OuédraogoDDSingboJDialloOSawadogoSATiénoHDraboYJRheumatoid arthritis in Burkina Faso: clinical and serological profilesClin Rheumatol201130121617162121887490
- ChakravartyKMcDonaldHPullarTBSR/BHPR guideline for disease-modifying anti-rheumatic drug (DMARD) therapy in consultation with the British Association of DermatologistsRheumatology (Oxford)200847611618077485
- SmolenJSLandewéRBreedveldFCEULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease modifying anti rheumatic drugs: 2013 updateAnn Rheum Dis10.1136/annrheumdis-2013-204573
- PloskerGLCroomKFSulfasalazine: a review of its use in the management of rheumatoid arthritisDrugs200565131825184916114981