Abstract
A 72-year-old Taiwanese woman had the history of cosmetic cryopreserved autologous fat injection on her forehead ~21 years ago and was referred to our oculoplastic clinic and presented with multiple painless mass, which she had for 4 years, on both upper eyelids. Histopathology confirmed the diagnosis of foreign body granuloma on both upper eyelids. Clinicians should be aware of the potential complication of granuloma reaction and migration even many years after the injection. We advise that autologous fat injection should be performed solely by trained physicians and it should be made known that there is a possible occurrence of migration.
Introduction
We present a case of foreign body granuloma on the eyelids secondary to cosmetic filler injection on the forehead, which developed several years after the injection. Filler migration and the clinical significance and microscopic features of granuloma lesions are also discussed. Written informed consent was obtained from the patient and this study was approved by the Tri-Service General Hospital review board (affiliated to the National Defense Medical Center).
Case report
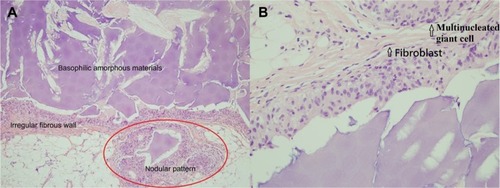
A 72-year-old Taiwanese woman was referred to our oculoplastic clinic, with swelling on both upper eyelids, with multiple painless nonmovable palpable masses, without blepharoptosis, which she had for 4 years. The best-corrected visual acuity of both eyes was 6/8.6, and intraocular pressure was normal. She had cosmetic cryopreserved autologous fat injection on her forehead ~21 years ago. She did not receive the injection around both eyelids, and there were no other specific problems after the injections. The masses were found below the eyebrow border, sized ~2.5 and ~2.0 cm in diameter in the right and left eyes, respectively, with well-defined, irregular-shaped borders firm on palpation. There was no sign of acute inflammation of the overlying skin (). Excisional biopsy was performed 1 week after the first visit. The excised mass was yellowish with an irregular border and had a rubbery consistency (indicated by arrows in ). The size of the mass detected in the subcutaneous region in the right eye was 2 cm × 1 cm (). Microscopic examination showed that foreign body granuloma was composed of multiple nodules characterized by basophilic amorphous materials surrounded by an irregular fibrous border (; hematoxylin and eosin [H&E], ×100). The fibrous border was composed of histiocytes, multinucleated giant cells, and fibroblasts (, ×400). After 1 year postoperative follow-up, the patient recovered well without obvious disfigurement and had only slight scar from the surgery.
Figure 1 Clinical photographs of the right eye.

Figure 2 Microscopic examinations.
Abbreviation: H&E, hematoxylin and eosin.
Discussion
Eyelid problems range from benign, self-resolving processes to malignant, possibly metastatic, tumors. In the past few decades, more and more people have been resorting to facial enhancement with dermal fillers for cosmetic purposes. Clinically, dermal fillers are composed of autologous fat, bovine collagen, paraffin, fluid silicone, polytetrafluoroethylene (Teflon; DuPont, Wilmington, DE, USA), and polymer and silicone particles. These fillers have been used to correct soft tissue defects as well as to fill in soft tissue volume around the lips and nasolabial region. For this reason, dermal fillers should have properties of biocompatibility, safety, and stability at the implant site and the abilities to maintain their volume, remain pliable, induce minimal foreign body reactions, and not cause foreign body granuloma.Citation1 Autologous fat is a nonallergenic, well-tolerated, supple, versatile implant material. Autogenous fat injection (AFI) into the periorbital or midface region is a common type of cosmetic surgery for rejuvenation in middle-aged and elderly Western subjects.Citation2 Common complications of facial AFI include unrealistic patient expectations, bruising, hematoma, undercorrection, overcorrection, and asymmetry contour of injection site.Citation3 Often these adverse reactions result from improper use of products performed by unskilled (or unlicensed) practitioners.Citation4 The complication of lipogranuloma formation at the periorbital area away from the AFI site is rarely reported.Citation5 It is plausible that the injected fat tissue on the forehead could move down to the periorbital area away from the injection site because of the movement of the frontalis muscle and gravity, as in the case of our patient. Furthermore, the fat tissue harvested for AFI is usually stored frozen at −20°C, but during such cryopreservation, ice crystals form inside the fat cell and many fat cells lose viability. Also, if the fat tissue without viability is injected, it can increase the risk for inflammation by foreign body reaction.Citation5 The patient in our report was confirmed to have used the cryopreserved AFI for the second time, and we consider this to be the cause of the lipogranuloma.
Conclusion
In conclusion, there is evidence present to show that potential complications after tissue injection of autologous fat still exist. Immediate injection of harvested fat tissue can be helpful for prevention of lipogranuloma. Also, we advise that AFI should be performed solely by trained physicians. As we treat similar cases, we should also be concerned with a possible occurrence of migration. In our study, the patient had palpable and visible masses near the upper eyelid that resulted from AFI on the forehead 21 years ago. Therefore, tracking patient’s detailed history and performing a thorough physical examination are necessarily important. If any unknown mass is detected, excisional biopsy should be immediately conducted by experienced clinicians for diagnosis to avoid severe facial disfigurement afterward.
Disclosure
The authors report no financial or conflicts of interest in this work.
References
- SankarVMcGuffHSForeign body reaction to calcium hydroxylapatite after lip augmentationJADA200713881093109617670876
- PaikJSChoWKParkGSYangSWEyelid-associated complications after autogenous fat injection for cosmetic forehead augmentationBMC Ophthalmol2013133223841959
- NiamtuJ3rdComplications in fillers and botoxOral Maxillofac Surg Clin North Am200921132119185791
- SchwartzfarbEMHamettiJMRomanelliPRicottiCForeign body granuloma formation secondary to silicone injectionDermatol Online J20081472018718204
- Ryeung ParkYChoiJAYoon LaTPeriorbital lipogranuloma after cryopreserved autologous fat injection at foreheadCan J Ophthalmol201348e166e16824314435
