Abstract
Type 2 diabetes is a chronic disease occurring in ever increasing numbers worldwide. It contributes significantly to the cost of health globally; however, its management remains in the most part less than optimal. Patients must be empowered to self-manage their disease, and they do this in partnership with health care professionals. Whilst the traditional role of the pharmacist has been centered around the supply of medicines and patient counseling, there is an evergrowing body of evidence that pharmacists, through a range of extended services, may contribute positively to the clinical and humanistic outcomes of those with diabetes. Further, these services can be delivered cost-effectively. This paper provides a review of the current evidence supporting the role of pharmacists in diabetes care, whilst providing a commentary of the future roles of pharmacists in this area.
Introduction
Diabetes mellitus (“diabetes”) is one of the fastest growing chronic diseases worldwide, and is associated with significant morbidity, mortality, and health care costs. Diabetes is characterized by high levels of glucose in the blood (hyperglycemia). There are three main types of diabetes:
Type 1 diabetes mellitus (T1DM) in which there is an absolute deficiency in insulin production. This disease can occur at any age, although it mostly occurs in children and young adults.Citation1
Type 2 diabetes mellitus (T2DM) which is associated with insulin resistance, with an initial increase in insulin secretion, however over time, beta cell death and insulin insufficiency. Although T2DM mainly occurs in people aged over 40 years old, the disease is also becoming increasingly prevalent in the younger age group.Citation2,Citation3
Gestational diabetes which occurs during pregnancy. The condition usually disappears once the baby is born; however, a history of gestational diabetes increases a woman’s risk of developing T2DM later in life.Citation1
The statistics related to diabetes mellitus globally are alarming. The International Diabetes Federation (IDF) Diabetes Atlas, Seventh Edition, 2015, provides the following estimates: one in 11 adults have diabetes (416 million), nearly half (46.5%) of adults with diabetes are undiagnosed, one in seven births are affected by gestational diabetes, 542,000 children have type 1 diabetes, and a person dies from diabetes every 6 seconds.Citation4 Further, the IDF estimates that by 2040, one in 10 adults (642 million) will have diabetes.Citation4
Of those people with diabetes, three quarters (75%) live in low- and middle-income countries.Citation4 The Western Pacific region (which includes Australia) has 37% of all adults living with diabetes. This includes 100 million people in the People’s Republic of China (ranked highest in number of people with diabetes), 10 million people in Indonesia (seventh highest), and 7.2 million in Japan (ninth highest). Also included in this region is the country with the highest prevalence of diabetes the Pacific Island nation of Tokelau where 30% of the adult population has diabetes. Globally, Cambodia has the lowest prevalence of diabetes at 3%.Citation4
T2DM is the greatest contributor to the burden of diabetes globally accounting for up to 90% of people with diabetes worldwide.Citation4 Further, its prevalence is increasing in all countries around the world. This increase has paralleled the global epidemic of obesity. It is estimated that since 1980 worldwide, obesity has nearly doubled. In 2008, it was estimated that there were 1.4 billion adults (35% of those 20 years or older) who were overweight, of which over half a billion (11%) were obese.Citation5 Importantly, it is reported that being overweight or obese contributes significantly to the burden of diabetes (44%), ischemic heart disease (23%), and certain cancers (range 7%–41%).Citation5 Yet, obesity is preventable, and strategies to prevent diabetes and cardiovascular disease both include the common goal to optimize peoples’ weight through diet and exercise.
Adults with diabetes have a two- to threefold increased risk of suffering a heart attack or stroke compared to those without diabetes.Citation6 The microvascular complications of diabetes mellitus make it the leading cause of preventable blindness, renal disease, and amputation in developed countries.Citation6–Citation8 These complications have dramatic implications for health care costs, with the total annual cost impact of diabetes in Australia estimated to be at $14.6 billion,Citation9 whilst globally, it is estimated to account for 12% of the global health expenditure (US$673 billion).Citation4 By 2040, it is estimated that the proportion of global health expenditure will exceed US$802 billion.Citation4
Optimizing therapy in patients with diabetes is a difficult clinical task requiring considerable patient education and motivation. The goal is to improve glycemic control without adverse bodyweight gain or hypoglycemia, and with a positive or neutral effect on lipid levels and blood pressure. Proper drug selection involves identifying the drug that is most likely to improve control and least likely to cause interactions, and adverse effect or adherence problems. Consequently, it has the potential to change patients’ futures and health care systems’ costs.Citation10
Pharmacists represent the third largest health profession in the worldCitation11 after doctors and nurses. Most pharmacists work in the community with a smaller proportion in hospital pharmacy, academia, industry, and research. Community pharmacies provide a range of products (in respect to diabetes prescription and nonprescription medication, blood glucose meters and testing strips, needles and swabs, dietary supplements) and services (such as medication review, vaccination, unit dose dispensing, needle exchange, point of care testing, disposal of unwanted medicines, etc).Citation12 Community pharmacists are considered to be the most accessible health care professionals, as no appointments are required to see them, and to have the highest level of patient contact. As such, they are well placed to play a significant role in the care of patients with T2DM.
This review discusses the health care requirements of T2DM and the current and future roles of pharmacists in its management. For the purposes of the review, papers were identified from English language PubMed and ScienceDirect databases up until October 2016, and by manually reviewing the references for the papers adjudged relevant based on title and abstract, and then full paper review. The keywords used included diabetes, pharmacist, pharmacy, intervention, glycosylated hemaglobin (HbA1c), improvement, benefit, and outcomes. Papers critiqued in this review include original research papers, together with systematic reviews and meta-analyses. The paper aims to provide an overview of the current evidence for the role of pharmacists in diabetes care and insights into what roles pharmacists may fulfill in the future.
Health care for T2DM patients
The management of those with T2DM should be seen as a partnership between the patient and health care professionals, in which the latter support the former in self-managing his or her disease. Management of every patient should commence with a detailed assessment at the initial diagnosis including an appraisal of diabetes complications and risk factors for complications. This provides the basis for continuing care that includes a treatment plan, treatment administration, monitoring, and review ( and ).Citation1,Citation13–Citation16
Figure 1 Model of care for T2DM in primary care.
Abbreviation: T2DM, type 2 diabetes mellitus.
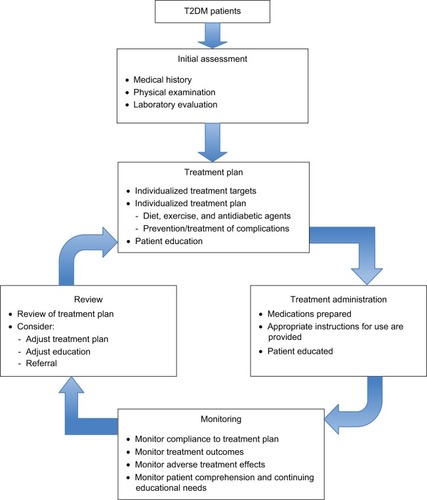
Table 1 Processes involved in the care of patients with T2DM
Pharmaceutical care is defined as “the responsible provision of drug therapy for the purpose of achieving definite outcomes that improve a patient’s quality of life”.Citation17 It provides a platform for multidisciplinary collaboration, which means that the pharmacist and the doctor (and potentially other care providers) join forces to decide on the optimal treatment of the patient so as to achieve the outcome the patient desires.Citation18 It requires that a professional relationship between the pharmacist and the patient is established and maintained, and records on patient’s medications and other specific information are collected and evaluated. In the case of prescription medicines, a therapy plan currently needs to be developed involving the doctor and the patient;Citation18 however, pharmacists may also provide input here.
Pharmacy-based services for T2DM patients
T2DM is one of a number of common complex conditions, including asthma, chronic obstructive pulmonary disease and heart failure, which require more time and expertise than one practitioner can reasonably provide to achieve optimal therapeutic outcomes for the patient.Citation1,Citation14 With the development of the concept of pharmaceutical care in which pharmacists are engaged more widely in patient care,Citation18 the opportunity exists for pharmacists to have a greater role in the care of patients with T2DM.
Evidence of the benefits of pharmacists in the care of T2DM patients
Extensive studies worldwide have evaluated the effectiveness of pharmacy-based interventions in supporting people with T2DM. Most of the studies have been conducted in developed western countries, particularly the United States of America,Citation19–Citation22 although examples can be found around the globe including the United Arab EmiratesCitation23 and Hong Kong.Citation24 Fewer studies however have been conducted in low- and middle-income countries such as Nigeria,Citation25 Iran,Citation26 India,Citation27,Citation28 Brazil,Citation29 Thailand,Citation30 Jordon,Citation31 Iraq,Citation32 and Malaysia.Citation33 The range of interventions evaluated are indicated in .
Table 2 Components of pharmacist interventions evaluated in T2DM
The interventions were measured for their effectiveness using the following:
clinical outcomes, such as glycemic control,Citation29,Citation34–Citation43 reduction of risk factors (such as blood pressure, lipids, and body mass index [BMI]),Citation29,Citation35,Citation42–Citation44 medication adherence,Citation34,Citation38,Citation44–Citation46 screening for complications,Citation43 and drug-related problems identified/solved;Citation35,Citation37,Citation38,Citation42,Citation45
humanistic/social outcomes, such as quality of life,Citation27,Citation35,Citation36,Citation42,Citation47 satisfaction,Citation42,Citation46 belief,Citation45 knowledge,Citation27,Citation37,Citation38,Citation41,Citation42 lifestyle changes,Citation44 and self-care activity;Citation47
economic outcomes, such as health costs.Citation42,Citation43
Blenkinsopp and HasseyCitation48 undertook a systematic review to evaluate the effect of community pharmacy interventions in diabetes (types 1 and 2). They reviewed seven papers, three focused on glycemic control, two on adherence, and one each on patient knowledge and medication problems. Six of the studies demonstrated positive results (), with two being significant. Components of community pharmacy-based interventions which appeared to contribute to effectiveness included the following: patient education/consultation about their diabetes and its treatment, medications, and lifestyle changes; and monitoring/reviewing glycemic control.Citation48 Since that review, there have been several others which are summarized in . These systematic reviews have covered the impact of pharmacists in a number of settings from hospitals, outpatients clinics, primary (community) health centers, and community pharmacy.Citation19–Citation21,Citation49–Citation51 The results of all of the systematic reviews demonstrate support for the role of pharmacist in diabetes care across the various settings.
Table 3 Summary of systematic reviews of pharmacists’ interventions in diabetes care
Collins et alCitation21 reported that HbA1c levels decreased by an average of 0.76% based upon results of 14 trials involving 2,073 subjects and fasting blood glucose by an average 1.63 mmol/L based upon results of four trials involving 589 subjects as compared to control subjects. Aguiar et alCitation19 undertook a meta-analysis of 22 studies which examined the effect of pharmacist interventions on glycemic control in T2DM patients. This analysis demonstrated a statistically and clinically significant reduction in HbA1c of −0.85% (95% confidence interval [CI]: −1.06 to −0.65, P < 0.0001). When community pharmacy interventions were compared to other outpatient settings, the effect on HbA1c was similar (−0.65% vs −0.98%, P = 0.08). Interestingly, overall, the most significant effect on HbA1c was seen in those studies in which participants’ baseline HbA1c was >9%. Further, the benefit derived reduced as the age of the participants increased.Citation19
Likewise, the reviews in have demonstrated statistically significant improvements in other clinical outcomes such as reduction in risk factors and improved medication adherence. For example, Santschi et al’sCitation20 meta-analysis demonstrated significant reductions in both systolic blood pressure (SBP) (−6.2 mmHg, 95% CI −7.8 to −4.2) and diastolic blood pressure (DBP) (−4.5 mmHg, 95% CI: −6.2 to −2.8). Six of the 14 studies included in the analysis of SBP involved community pharmacies, with three showing significant falls of between −5.6 mmHg and −20.05 mmHg. Of the two community pharmacy based trials included in the same meta-analysis which reported DBP changes, both again demonstrated a positive effect, and one of them was significant (−3.90 mmHg, 95% CI: −7.18 to −0.62). Significant reductions were also reported for total cholesterol, low-density lipoprotein cholesterol, and BMI.
Despite significant variations in the methods by which adherence was measured, pharmacist interventions were generally shown to have a positive effect, although it was unclear in many instances what impact the improvement had on clinical outcomes.Citation50 Patients’ knowledge of their disease and its complications, its treatment (pharmacological and non-pharmacological), and self-monitoring has also been shown to be increased through pharmacist-delivered educational interventions.Citation51
The ability to demonstrate improvements in the quality of life of people with diabetes is often hampered by the short duration of the studies, and the tools chosen. Despite these factors, pharmacist-managed interventions again showed positive benefits. Limited studies have investigated the economic benefits of pharmacist interventions in diabetes care. A recent meta-analysis by Wang et al,Citation22 which included 25 studies, reported that “pharmacist-managed services had a positive return in terms of economic viability”. Ten of the 25 studies were completed in community pharmacy. Benefits demonstrated included that the average cost of a 1% reduction in HbA1c was US$174 per person; such a reduction translates into a 21% reduction in macrovascular complications. Further, whilst pharmacist interventions often increased medication costs, these costs were offset by a reduction in medical costs associated with emergency department attendances and hospitalization.Citation22 In fact, compared to usual care, pharmacist-led services produced cost savings in the range of US$8 to $85,000 per year, whilst costing between US$62,803 and US$114,576 to prevent one diabetes-related macrovascular and microvascular event. Of the six studies that included cost–benefit analysis (cost-to-benefit ratio range 1:1–8.5:1), the three that were community pharmacy based were either cost neutral (1:1)Citation52 or cost effective (6.1:1Citation53 and 8.5:1Citation54). Hendrie et alCitation55 evaluated the economic benefit of reduced glycemic events (hypo- and hyperglycemia) in a group of patients who enrolled into a 6-month Diabetes Management Education Program (DMEP). They found that the intervention resulted in significantly greater reductions in the number of hyper- and hypoglycemic events relative to the control group (odds ratio [OR] 0.34, 95% CI 0.22–0.52, P = 0.001 vs OR 0.54, 95% CI 0.34–0.86, P = 0.009). This reduction translated into a net reduction of 1.86 days with glycemic episodes per patient per month. In terms of cost-effectiveness, the DMEP costs AU$43 (US$39) per day of glycemic symptoms avoided relative to standard care.
In summary, to date, pharmacist interventions to improve the care of patients with diabetes, and in particular those with T2DM, have been shown to deliver positive clinical, humanistic, and economic benefits. However, the interventions, which are often multifaceted, have varied across studies, although often education- and clinical review-based, making it difficult to determine which elements deliver the greatest benefits.
Future roles for pharmacists in T2DM management
To date, evidence supports pharmacists extending their role in diabetes care from medication supply to cognitive services which aim to assist those with diabetes achieve the best possible clinical outcomes through supporting their self-management. Realistically, pharmacists potentially have a role to play in all facets of the care of T2DM patients as depicted in . However, widespread implementation of such services in the future will depend on legislative change, adequate funding (government and nongovernment), professional commitment, interprofessional collaboration, and consumer (patient) acceptance.
The importance of the latter should not be underestimated, with recent work again illustrating that consumers do not perceive community pharmacies as a place to go to get assistance with their diabetes care. Consumers are happy to accept that pharmacists can provide them with medications and counseling; however, they have consistent concerns about the knowledge and competency of pharmacists to provide additional services, and that community pharmacies are a suitable environment to deliver them.Citation56 The findings of Dhippayom and KrassCitation57 support this, with participants in their study highlighting the main role of pharmacists is medication provision, with some enhancements in supporting adherence and continuity of supply. Therefore, for community pharmacy-based services to succeed, these perceptions must be changed; this will require action from within the pharmacy profession through further training, establishment of private consulting areas, changes to workflows, and proactively promoting pharmacists’ capability to deliver enhanced diabetes care.
Delivery of such services within other settings such as hospitals, outpatient clinics, and community-based clinics is likely to be better received by patients, with pharmacists being seen more as a care provider than a supplier of medicines. Evidence supports pharmacists working in these settings, either directing care or collaborating in care.Citation20
Targeting of services to those at greatest need would seem appropriate, such as patients with newly diagnosed diabetesCitation56 who are often overwhelmed by the diagnosis and have a poor understanding of its management. For example, general practitioners often fail to provide adequate education for patients starting oral hypoglycemics, and community pharmacists are well placed to fulfill this role. Further, the evidence suggests that patients with poorly managed diabetes, that is, those with HbA1c > 9 mmol/L,Citation19 gain the greatest benefit from pharmacist interventions, suggesting targeting such patients would be appropriate. This could be facilitated through referrals from medical practitioners or pharmacists ordering of HbA1c levels or point-of-care testing.
Funding to deliver pharmacy-based cognitive services is a contentious issue, and whilst they can be funded through a user-pays model, government-funded or third-party payer models are likely to be needed for widespread implementation of such services. For example, depending on the level of remuneration, one would envisage that a limited number of community pharmacies specializing in diabetes would offer extended services. Legislative change to allow pharmacists to manage patients’ diabetes therapy either in consultation with their primary health provider or independently, which has occurred in some jurisdictions, will allow pharmacists delivering such services to have greater impact.
Diabetes screening is another area of significant need which pharmacists should engage in as many people living with the disease are undiagnosed. A large-scale trial is about to commence in Australia to evaluate community pharmacists’ role in diabetes screening. This study builds upon the work of Krass et al,Citation58 which demonstrated that a sequential screening program, that is, tick test followed by capillary blood glucose testing, was an effective means to detect prediabetic and diabetic patients.
Conclusion
There is significant evidence to support the role of pharmacists in providing a range of extended diabetes care services, from the screening to ongoing disease state management. However, despite this, the provision of such services generally remains limited and inconsistent. However, this is set to change, as the number of people with T2DM grows, and the capacity of traditional care providers to cope with these people diminishes. Governments, third-party payers, and consumers will all be looking for cost-effective ways to manage diabetes. Pharmacists are ideally placed to assist patients with their diabetes management within a range of clinical settings as demonstrated by current evidence. Needed now are models of practice which are evidence based, consistent, and scalable, such that they deliver the outcomes desired by all stakeholders.
Disclosure
The authors report no conflicts of interest in this work.
References
- American Diabetes AssociationStandards of medical care in diabetes - 2013Diabetes Care201336Suppl 1S11S6623264422
- Pinhas-HamielOZeitlerPThe global spread of type 2 diabetes mellitus in children and adolescentJ Pediatr2005146569370015870677
- American Diabetes AssociationType 2 diabetes in children and adolescentsDiabetes Care200023338138910868870
- International Diabetes FederationIDF Diabetes AtlasSeventh Edition2015 Available from: www.diabetesatlas.orgAccessed October 28, 2016
- World Health OrganizationObesity and overweight. Fact sheet [updated June 2016] Available from: http://www.who.int/mediacentre/factsheets/fs311/en/Accessed October 28, 2016
- World Health Organization DiabetesFact sheet [reviewed November 2016] Available from: http://www.who.int/mediacentre/factsheets/fs312/en/Accessed November 27, 2016
- FowlerMJMicrovascular and macrovascular complications of diabetesClin Diabetes20082627782
- KocurIResinkoffSVisual impairment and blindness in Europe and their preventionBr J Ophthalmol200286771672212084735
- Diabetes AustraliaDiabetes in Australia2015 Available from: https://www.diabetesaustralia.com.au/diabetes-in-australiaAccessed October 28, 2016
- ChloeHMMitrovichSDubayDHaywardRAKreinSLVijanSProactive case management of high-risk patients with type 2 diabetes mellitus by clinical pharmacist: a randomized controlled trialAm J Manag Care200511425326015839185
- FIP.orgGlobal pharmacy workforce and migration report: a call for action2016 Available from: https://www.fip.org/files/fip/publications/PharmacyWorkforceMigration.pdfAccessed October 28, 2016
- OECD.orgHealth at a glance 20152015 Available from: http://www.oecd.org/els/health-systems/health-at-a-glance-19991312.htmAccessed October 28, 2016
- The Royal Australian College of General PractitionersGeneral Practice Management of Type 2 Diabetes: 2016–18East Melbourne, VicRACGP2016 Available from: https://static.diabetesaustralia.com.au/s/fileassets/diabetes-australia/5d3298b2-abf3-487e-9d5e-0558566fc242.pdfAccessed December 22, 2016
- Indonesian Society of EndocrinologyConsensus on the Management and Prevention of Type 2 DM in IndonesiaJakartaIndonesian Society of Endocrinology2011
- PowerADouglasEMcGregorAHudsonSProfessional development of pharmaceutical care in type 2 diabetes mellitus: a multidisciplinary conceptual modelInt J Pharm Pract2006144289299
- Department of Health, WA, AustraliaDiabetes Model of CareHealth Networks Branch, Department of HealthPerth, WA, Australia2008 Available from: http://www.healthnetworks.health.wa.gov.au/model-sofcare/docs/Diabetes_Model_of_Care.pdfAccessed November 27, 2016
- HelperCDStrandLMOpportunities and responsibilities in pharmaceutical careAm J Hosp Pharm19904735335432316538
- BerenguerBLa CasaCde la MattaMMartin-CaleroMJPharmaceutical care: past, present and futureCurr Pharm Des200410313931394615579081
- AguiarPMBrito GdeCLima TdeMSantosAPLyraDPJrStorpirtisSInvestigating sources of heterogeneity in randomized controlled trials of the effects of pharmacist interventions on glycemic control in type 2 diabetic patients: a systematic review and meta-analysisPLoS One2016113e015099926963251
- SantschiVChioleroAParadisGColosimoALBurnandBPharmacist interventions to improve cardiovascular disease risk factors in diabetes: a systematic review and meta-analysis of randomized controlled trialsDiabetes Care201235122706271723173140
- CollinsCLimoneBLSchooleJMColemanCIEffect of pharmacist intervention on glycemic control in diabetesDiabetes Res Clin Pract201192214515220961643
- WangYYeoQQKoYEconomic evaluations of pharmacist-managed services in people with diabetes mellitus: a systematic reviewDiabet Med201633442142726433008
- Al MazrouiNRKamalMMGhabashNMYacoutTAKolePLMcElnayJCInfluence of pharmaceutical care on health outcomes in patients with type 2 diabetes mellitusBr J Clin Pharmacol200967554755719552750
- ChanCWSiuSCWongCKLeeVWA pharmacist care program: positive impact on cardiac risk in patients with type 2 diabetesJ Cardiovasc Pharmacol Ther2012171576421335480
- AdibeMOUkweCVAguwaCNThe impact of pharmaceutical care intervention on the quality of life of Nigerian patients receiving treatment for type 2 diabetesValue Health Reg Issues201322240247
- FarsaeiSSabzghabaeeAMZargarzadehAHAminiMEffect of pharmacist-led patient education on glycemic control of type 2 diabetics: a randomized controlled trialJ Res Med Sci2011161434921448382
- AdepuRRasheedANagaviBGEffect of patient counseling on quality of life in type-2 diabetes mellitus patients in two selected South Indian community pharmacies: a studyIndian J Pharm Sci2007694519524
- VenkatesanRDeviASParasuramanSSriramSRole of community pharmacists in improving knowledge and glycemic control of type 2 diabetesPerspect Clin Res201231263122347699
- CorrerCJMelchiorsACFernandez-LlimosFPontaroloREffects of a pharmacotherapy follow-up in community pharmacies on type 2 diabetes patients in BrazilInt J Clin Pharm201133227328021394570
- PhumipamornSPongwecharakJSoorapanSPattharachayakulSEffects of the pharmacist’s input on glycaemic control and cardiovascular risks in Muslim diabetesPrim Care Diabetes200821313718684418
- JarabASAlqudahSGMukattashTLShattatGAl-QirimTRandomized controlled trial of clinical pharmacy management of patients with type 2 diabetes in an outpatient diabetes clinic in JordanJ Manag Care Pharm201218751652622971205
- MahwiTOObiedKARole of the pharmaceutical care in the management of patients with type 2 diabetes mellitusInt J Pharm Sci Res20134413631369
- ChungWWChuaSSLaiPSChanSPEffects of a pharmaceutical care model on medication adherence and glycemic control of people with type 2 diabetesPatient Prefer Adherence201481185119425214772
- BerringerRShibleyMCCaryCCPughCBPowersPARafiJAOutcomes of a community pharmacy based diabetes monitoring programJ Am Pharm Assoc (Wash)199939679179710609444
- KrassIArmourCLMitchellBThe Pharmacy Diabetes Care Program: assessment of a community pharmacy diabetes service model in AustraliaDiabet Med200724667768317523968
- ArmourCLTaylorSJHourihanFSmithCKrassIImplementation and evaluation of Australian pharmacists’ diabetes care servicesJ Am Pharm Assoc2004444455466
- FornosJAAndrésNFAndrésJCGuerraMMEgeaBA pharmacotherapy follow-up program in patients with type-2 diabetes in community pharmacies in SpainPharm World Sci2006282657216791717
- WermeilleJBennieMBrownIMcKnightJPharmaceutical care model for patients with type 2 diabetes: integration of the community pharmacist into the diabetes team - a pilot studyPharm World Sci2004261182515018255
- CranorCWBuntingBAChristensenDBThe Asheville Project: long-term clinical and economic outcomes of a community pharmacy diabetes care programJ Am Pharm Assoc (Wash)200343217318412688435
- BlissEACodackHBootheJDiabetes care - an evaluation of a community pharmacy based HbA1c testing servicePharm J2001267264266
- SwainJHMacklinRIndividualised diabetes care in a rural community pharmacyJ Am Pharm Assoc (Wash)200141345846111372911
- HughesJFinal report: Customised education programs for patients with diabetes mellitus - use of structured questionnaires and education modules (DMEP study)PerthCurtin University of Technology2006 Available from: http://6cpa.com.au/resources/third-agreement/customised-education-programs-for-patients-with-diabetes-mellitus-use-of-structured-questionnaires-and-education-modules/Accessed December 21, 2016
- FeraTBlumlBMEllisWMSchallerCWGarrettDGThe diabetes ten city challenge: interim clinical and humanistic outcomes of a multisite community pharmacy diabetes care programJ Am Pharm Assoc (2003)200848218119018359731
- PintoSLBechtolRAParthaGEvaluation of outcomes of a medication therapy management program for patients with diabetesJ Am Pharm Assoc (2003)201252451952322825233
- KrassIStephensonSThuisUHourihanFTaylorSArmourCIncreasing adherence to medications through delivery of a disease management service for Type 2 diabetes in community pharmaciesJ Soc Admin Pharm2002196211
- GrantRWDevitaNGSingerDEMeigsJBImproving adherence and reducing medication discrepancies in patients with diabetesAnn Pharmacother2003377–896296912841801
- AbduelkaremARSackvilleMAChanges of some health indicators in patients with type 2 diabetes: a prospective study in three community pharmacies in Sharjah, United Arab EmiratesLibyan J Med200941313621483500
- BlenkinsoppAHasseyAEffectiveness and acceptability of community pharmacy-based interventions in type 2 diabetes: a critical review of intervention design, pharmacist and patient perspectivesInt J Pharm Pract2005134231240
- PousinhoSMorgadoMFalcãoAAlvesGPharmacist interventions in the management of type 2 diabetes mellitus: a systematic review of randomized controlled trialsJ Manag Care Spec Pharm201622549351527123912
- OmranDGuirguisLMSimpsonSHSystematic review of pharmacist interventions to improve adherence to oral antidiabetic medications in people with type 2 diabetesCan J Diabetes2012365292299
- WubbenDPVivianEMEffects of pharmacist outpatient interventions on adults with diabetes mellitus: a systematic reviewPharmacotherapy200828442143618363526
- PetkovaVBPetrovaGIPilot project for education of patients with type 2 diabetes by pharmacistsActa Diabetol2006432374216865327
- BuntingBALeeGKnowlesGLeeCAllenPThe hickory project: controlling healthcare costs and improving outcomes for diabetes using the Asheville project modelAm Health Drug Benefits20114634335025126361
- WertzDHouLDeVriesAClinical and economic outcomes of the Cincinnati Pharmacy Coaching Program for diabetes and hypertensionManag Care20122134454
- HendrieDMillerTRWoodmanRJHotiKHughesJCost-effectiveness of reducing glycaemic episodes through community pharmacy management of patients with type 2 diabetes mellitusJ Prim Prev201435643944925257687
- TwiggMJPolandFBhattacharyaDDesboroughJAWrightDJThe current and future roles of community pharmacists: views and experiences of patients with type 2 diabetesRes Social Adm Pharm20139677778923127392
- DhippayomTKrassISupporting self management of type 2 diabetes: is there a role for the community pharmacist?Patient Prefer Adherence201591085109226257514
- KrassIMitchellBClarkePPharmacy diabetes care program: analysis of two screening methods for undiagnosed type 2 diabetes in Australian community pharmacyDiabetes Res Clin Pract200775333934716884811
