Abstract
Heterogeneity of asthma and difficulty in achieving optimal control are the major challenges in the management of asthma. To help attain the best possible clinical outcomes in patients with asthma, several guidelines provide recommendations for patients who will require a referral to a specialist. Such referrals can help in clearing the uncertainty from the initial diagnosis, provide tailored treatment options to patients with persistent symptoms and offer the patients access to health care providers with expertise in the management of the asthma; thus, specialist referrals have a substantial impact on disease prognosis and the patient’s health status. Hurdles in implementing these recommendations include lack of their dissemination among health care providers and nonadherence to these guidelines; these hurdles considerably limit the implementation of specialist referrals, eventually affecting the rate of referrals. In this review, recommendations for specialist referrals from several key international and national asthma guidelines and other relevant published literature are evaluated. Furthermore, we highlight why referrals are not happening, how this can be improved, and ultimately, what should be done in the specialist setting, based on existing evidence in published literature.
Introduction
Asthma is a chronic inflammatory disease of the airway that affects between 235 and 300 million people worldwide, with ~250,000 annual deaths worldwide attributed to this disease.Citation1,Citation2 However, asthma is not a simple airway disease; it is heterogeneous and associated with a range of phenotypes related to age of onset, triggers and type of inflammation (eosinophilic, neutrophilic and pauci-granulocytic phenotypes), and can be further defined on the basis of endotypes.Citation3,Citation4 Furthermore, asthma-related symptoms (such as shortness of breath, chest tightness, cough and wheezing that can vary over time and in intensity, together with variable expiratory airflow limitation) are shared with other conditions such as acute and long-term cardiovascular, metabolic, psychologic/psychiatric and other respiratory conditions. Owing to the complexity of the disease, certain patients with asthma will require a referral to an asthma specialist to address certain aspects of their condition. Such a referral can have a significant impact on the patient’s health status. Currently, numerous guidelines are available that provide guidance on when a patient with asthma should be referred to a specialist. For optimal management of these patients, it is important that guideline recommendations for specialist referrals are implemented fully and consistently. In this regard, an overview of the current practice of specialist referrals, possible hurdles in the implementation of referrals and possible strategies for improved rate of referrals would be helpful. This review explores the criteria set forth as reasons for referring patients to specialists from various guidelines/strategy documents and how these referrals are utilized in the management of asthma patients.
Methods for compiling asthma guidelines/strategy recommendations for specialist referral
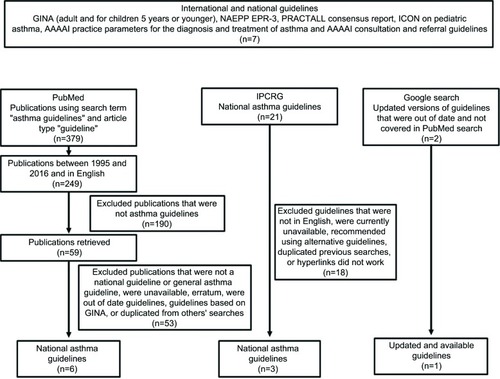
In order to compile asthma guidelines that would be reviewed, a four-step process was utilized. All well-documented international and national guidelines were obtained (). A review of the literature was also carried out by searching the PubMed database (from 1995 to 2016) using the search term “asthma guidelines” and restricting the article type to “guideline” (). The retrieved publications from this search were manually reviewed and nonrelevant publications were excluded based on several criteria as outlined in . The International Primary Care Respiratory Group asthma guideline database was also searched for national asthma guidelines (). Finally, once the asthma guidelines/consensus documentations were identified by the methods previously described, subsequent searches were conducted using the Google search engine to establish if updated versions existed ().
Figure 1 Guideline selection process.
For this review, literature searches were restricted to guidelines, as previously stated, or manuscripts in English language; limited information from regional guidelines has also been included due to their international impact (e.g., Spanish Guideline on the Management of Asthma [GEMA] and the Japanese asthma guidelines). Using the common themes from the guidelines/strategy documents that specialists can play a pivotal role in all aspects of asthma management, all the guidelines/strategy documents criteria/recommendations for referrals were examined under four categories: 1) diagnostic uncertainty, 2) asthma severity and high-risk patients, 3) use of corticosteroid treatment (high doses, long-term use and side effects) and 4) the use of add-on specialist therapy (biologics). and summarize the results of the compiled guidelines/strategy documents (specialist referral recommendations based on guideline and evidence) for adults and children, respectively.
Table 1 Guideline recommendations for referral of adult asthma patients to a specialist
Table 2 Guideline recommendations for referral of pediatric asthma patients to a specialist
Asthma guidelines as sources for indications for specialist referrals
Global and national guidelines aim to improve the diagnosis and management of asthma and ensure that the best practice is implemented consistently. The Global Initiative for Asthma (GINA) has developed a detailed recommendation on the global strategy for asthma management, but because it is only a strategy, the indications for referral may vary due to variations across health care systems.Citation5 The GINA strategy is designed to be adapted in order to improve its implementation within the local health care systems or to increase its use for a particular health care professional (HCP).Citation6,Citation7 The national guidelines include the British Thoracic Society (BTS) asthma guideline in the UK,Citation8 the National Asthma Education and Prevention Program (NAEPP) Expert Panel Report-3 in the USA,Citation9 GEMA in Spain,Citation10 the Japanese asthma guidelinesCitation11 and the South African guideline.Citation12 Guidelines that address asthma management in children include the NAEPP, the Practical Allergy (PRACTALL) consensus report, the GINA strategy document on asthma management and prevention in children aged 5 years and youngerCitation5,Citation9,Citation13 and the International Consensus on pediatric asthma,Citation14 with some countries, such as South Africa and Japan, having specific national guidelines.Citation15,Citation16 Adherence to asthma guidelines/strategy documents, such as the GINA strategy, has been shown to improve the quality of lifeCitation17 and decrease the morbidity and mortality associated with asthma.Citation18
Guideline and strategy documents recommendations for specialist referrals
Diagnostic uncertainty
Asthma diagnosis could be confounded by a lack of access to diagnostic equipment, which is also a reason to seek referral. Several of the guidelines confirm an uncertain diagnosis of asthma as a reason to refer patients to a specialist, except for the PRACTALL consensus reportCitation13 and the Japanese guideline for childrenCitation16 ().
Several factors aid asthma diagnosis, such as a carefully recorded history, and clinical and diagnostic assessments (spirometry and biomarkers), and all of the guidelines presented in allude to these to some extent. GINA recommends spirometry as the preferred diagnostic test for asthma, whereby measurements of airflow limitation, reversibility or bronchial challenge are also used to establish a diagnosis of asthma,Citation5 and the involvement of a specialist can result in better access to this tool.Citation19 More recently, fractional exhaled nitric oxide (FeNO) has been identified as another diagnostic tool for establishing an asthma diagnosis;Citation20 however, depending on the health care system, not all necessary tests (e.g., spirometry, FeNO, hyperresponsiveness) may be available in primary care facilities, and BTS asthma guideline clearly indicates that referral to specialist should be sought should such diagnostic tests not be available in primary care.Citation8 Furthermore, discrepancy between guidelines and strategy documents exists on such diagnostics tools. An example of this would be the test for FeNO, where GINA states that this test has not been established as being useful in making a diagnosis of asthma.Citation5 On the other hand, in the recent BTS guidelines, a positive FeNO test increases the probability of asthma but a negative test does not exclude asthma.Citation8
A recent real-life study demonstrated that using a single test alone was not optimal for an accurate diagnosis, but rather a combination of multiple diagnostic tests in a specialist setting resulted in an increase in diagnostic accuracy, and determined that 81% of asthma cases could be confirmed objectively.Citation21 Diagnostic uncertainty in asthma is evident from the literature, as there is conflicting evidence on asthma being underdiagnosedCitation22,Citation23 or overdiagnosed,Citation24–Citation26 suggesting that the correct or accurate diagnosis of asthma, especially in children,Citation27 remains an issue among physicians. Clinical symptoms of asthma (e.g., cough and wheezing) do not definitively confirm an asthma diagnosis, especially in children.Citation5,Citation9,Citation13 Also, there is variability among physicians in identifying the standard primary symptoms of asthma.Citation28 Interestingly, the GINA strategy for children under 5 years of age suggests that several key indications should lead to a referral for further diagnostic investigations, such as therapeutic trials of inhaled medication; testing for atopy; chest X-ray; spirometry in children 4–5 years of age; FeNO; and risk profiling tools, for example, asthma predictive index ().Citation5 The American Academy of Allergy Asthma and Immunology (AAAAI) consultation and referral guidelines also suggest that patients with respiratory symptoms who have a normal lung function should be referred to an immunologist/allergist for a methacholine challenge test.Citation29 For patients with allergic asthma, the AAAAI practice parameters document indicates that there is a requirement for a referral to establish the target allergen causing asthma by using adequate tests, such as the skin prick test, which require adequate training to perform and interpret results.Citation29
Diagnosis of asthma or evaluation of symptoms can be further complicated by the presence of comorbidities, as they may cause respiratory symptoms.Citation30 For instance, gastroesophageal reflux disease, sinusitis, allergic rhinitis and nasal polyposis can all result in the worsening of asthma symptomsCitation31 and, therefore, may result in some diagnostic uncertainty. NAEPP guidelines highlight that patients with conditions such as sinusitis, nasal polyps, aspergillosis, severe rhinitis, vocal cord dysfunction, gastroesophageal reflux disease and chronic obstructive pulmonary disease should be referred to a specialist.Citation9
Asthma severity and high-risk patients
Some patients with asthma remain uncontrolled despite receiving standard-of-care therapy.Citation32 While it might seem appropriate that all patients with uncontrolled asthma should undergo specialist assessment, such a solution would overwhelm any health care system. Therefore, there is a fundamental need to select appropriate uncontrolled asthma patients for referral to a specialist.
A review of the guidelines in suggests a substantial variation in recommendations for high-risk patients seeking a referral. Prior to a referral, primary care physicians (PCPs) play a pivotal role in addressing the factors behind poor control (e.g., poor adherence, inhaler technique and comorbidities).Citation5,Citation33 The AAAAI practice document suggests that all asthma patients should be considered for a referral, which, as highlighted previously, could result in resource constraints for a health care system. Several of the guidelines recommend that certain patients seek more specialized care (); for example, GINA indicates that uncontrolled adult patients receiving step 4 asthma therapy (moderate or high-dose inhaled corticosteroid [ICS]/long-acting β2-agonist or regular asthma-related health care utilization) and frequent exacerbators should be referred for add-on treatment, that is, anti-immunoglobulin E (anti-IgE) treatment or mepolizumab (). In the guidelines addressing children with asthma, lack of control despite recommended treatment, usually medium- or high-dose ICS, is sufficient to seek a referral (). GEMA highlights that patients classified as having difficult-to-control asthma should be treated in a specialized setting.Citation10 While the BTS guidelines do not specifically mention lack of asthma control as an indicator for a referral in adults, the continuation of certain symptoms and a biomarker (blood eosinophils) are listed as indicators for a referral.Citation8 Furthermore, both AAAAI publications on asthma referrals advise that patients with uncontrolled asthma should be referred to an immunologist/allergist (). According to the NAEPP and Japanese adult guidelines, patients with other comorbidities that could affect asthma controlCitation30 constitute a high-risk group and should be referred to a specialist.
Aside from uncontrolled patients, some of the guidelines suggest that other patient cohorts should be referred to a specialist. The South African guidelines for adults and the AAAAI consultation and referral guideline suggest that severe asthma is a reason to seek a specialist referral. The Australian guidelines indicate that patients who have evidence of poor lung function despite the use of a high dose of ICS for 3 months should seek a referral. GEMA recommends that patients who fail to respond to treatment must be referred to a hospital emergency department (ED).Citation10 In the case of severe asthma, guideline definitions of severe asthma and subsequent treatment recommendations are widely inconsistent because different guidelines use different criteria to define suboptimal asthma control.Citation34 The differences in criteria are broadly centered on interpreting clinical evidence and framing recommendations. For example, there is a lack of clarity on whether patients should go to step 3 or step 4 or even step 5 treatment if they are uncontrolled, clearly indicating that the threshold for change in treatment step is not clear. Currently, this threshold is so broad that approximately over 20% of patients receiving combination therapy could be referred to a specialist.Citation35 In light of the significant consequences of inconsistencies among guideline definitions and recommendations, a common set of validated and clear methods across global and regional guidelines could harmonize treatment recommendations and enable guideline implementation in the management of severe asthma.
Exacerbations are known to have a huge impact on a patient’s quality of life,Citation36 with asthma control and exacerbation history being predictors of future exacerbations.Citation37 Previously, it has been suggested that 20% of patients with asthma have had an exacerbation requiring hospitalization and these events can account for up to 80% of the costs associated with asthma.Citation38 Specialist care can reduce the number of hospitalizations and the risk of future hospitalizations.Citation39 GEMA guidelines suggest that high-risk asthma attacks or when severe asthma attacks occur and complications are suspected as a need to seek a referral to a hospital ED.Citation10 GINA, AAAAI and NAEPP guidelines indicate that patients who have frequent asthma-related health care utilization or a hospitalization/ED visit should be considered as high-risk individuals and, therefore, be referred (). The Irish guidelines follow this suggestion with some more specificity, stating that patients could be referred post-hospitalization if uncontrolled at step 3.Citation6 The only other guideline with reference to an exacerbation/hospitalization as a cause for referral is the South African guideline, which recommends that adults who have two or more exacerbations per month are a group who should seek specialist care.Citation12 The South African pediatric guideline is less specific in suggesting that frequent hospitalizations are a reason to refer ().
Furthermore, every year it is estimated that a quarter of a million deaths worldwide are asthma related.Citation2 The importance of referrals for patients has been recently highlighted in a British evaluation of asthma deaths, whereby 20% of deaths investigated were related to avoidable factors associated with referrals (including delays or failure of referral for specialist opinion) and over 50% of patients were not under specialist supervision prior to their deaths.Citation39 Of the guidelines examined in this review, only the GINA, NAEPP and AAAAI referral guidelines specifically recommend that patients who are at risk of an asthma-related death (GINA) or fatal asthma (AAAAI) or fatally prone (NAEPP) should be referred to a specialist ().
Use of corticosteroid treatment
Steroids play an important role in the management of asthma in the form of ICS and oral corticosteroids. These therapies have a positive impact on controlling symptoms and exacerbations.Citation40 However, there are side effects associated with this treatment, such as growth suppression,Citation41 hypothalamic–pituitary–adrenal axis suppression in children,Citation42 cataracts,Citation43,Citation44 diabetes,Citation45 and bone density changes and osteoporosis.Citation46,Citation47 Similar to patients with chronic obstructive pulmonary disease, there is a suggestion that ICS use is associated with higher risk for asthma patients developing pneumonia or lower respiratory tract infections, particularly when used in high doses.Citation48 More recently, it has been demonstrated that morbidity rates were increased for conditions associated with systemic steroid exposure in patients with severe asthma.Citation49
Therefore, given the risks associated with this therapy, there is a need to monitor its use. With regard to recommendations regarding the side effects in the guidelines, GINA suggests that any evidence or risk of side effects from treatments is a reason to refer adults or children aged between 6 and 11 years ().Citation5 A similar statement is made by the AAAAI, using the example of oral corticosteroids and ICS in children.Citation29 The Canadian guidelines also highlight the use of high-dose ICS in children and its possible side effects as an indication for referral ().Citation50
Long-term use of high doses of corticosteroids is associated with the development of systemic side effects.Citation49,Citation51 It is evident that there is a high use of ICS in asthma, and some of these patients are not severe enough to require this treatment, as observed in a British study where 90% of the patients were receiving ICS despite the fact that over 50% were classified as having intermittent asthma, and thus did not warrant controller therapy.Citation52 A specialist referral could provide the opportunity to review the dosage of ICS prescribed, and possibly to step down the dose when asthma control is maintained. GINA further elaborates on seeking a specialist referral at step 5 when there is need for add-on treatment, which is a preferred option to oral corticosteroids, if there is long-term use of oral corticosteroids or frequent use of oral corticosteroids (e.g., two or more courses in 1 year; ). For children with asthma, both the South African and Singaporean guidelines provide more specificity on the doses of ICS prescribed that would justify these patients being referred to a specialist (). The AAAAI practice document states that long-term use of any medication should be an indication for a referral.Citation29
PRACTALL covers the topic of prescribing unlicensed dose of steroids in children as a reason to seek a referral to a specialist (). Such use of steroids has been documented in an observational study, where ~5% of children aged between 5 and 11 years and 4% of children aged <5 years were prescribed unlicensed high doses of ICS, which could potentially expose these patients to treatment-related adverse effects.Citation53 An examination of the Australian, BTS, Japanese and GINA guidelines for children ≤5 years of age reveals that these guidelines do not offer any recommendations on when to refer patients with corticosteroid use in asthma, despite the fact that some of the recommendations are adapted from guidelines that do cover this topic.
Use of add-on specialist therapies
Referring a patient to a specialist may allow them access to additional health care resources and add-on therapies, such as omalizumab, which are not available in the primary care setting. A recent Italian and German study highlighted that 12% of patients who were being treated by PCPs and office-based respiratory consultants were eligible for omalizumab, but were not receiving this therapy.Citation54 Access to additional health care resources and treatments not available in the primary care setting could prevent the chronic use of oral corticosteroids by patients, thus reducing their exposure to the associated side effects of this treatment.Citation5 This has been well documented with omalizumab, where a reduction in the use of ICSCitation55–Citation57 and oral corticosteroids in adultsCitation58 and childrenCitation59 was observed. The use of this specialized add-on therapy has only been captured in a few guidelines. GINA specifically recommends asthma treatment to be on the basis of the level of asthma control, and it further suggests referring patients in step 5 (severe asthma) to a specialist, so that they can be assessed for additional add-on treatment, such as anti-IgE therapy or mepolizumab, which is preferred over oral corticosteroids.Citation5 The BTS, AAAAI, Canadian, Japanese and South African guidelines also indicate that patients should be referred to a specialist if anti-IgE therapy is being considered. The specialist will also provide a vital checkpoint whereby, when required for certain patients, there would be an appropriate escalation to additional therapies such as omalizumab for severe allergic asthma patients. In the near future, there will be more biologics indicated for use in asthma, such as anti-interleukin (IL)-4/IL-13 (dupilumab), anti-IL13 (lebrikizumab) and new anti-IL-5 therapies (reslizumab and benralizumab)Citation60 and guidelines will have to be updated accordingly. The use of biologics will require a broader diagnostic setup, potentially with biomarkers, in order to define eligible patients for each entity, which might only be available in a specialized center. This would allow for more personalized medicine, as well as the involvement of a specialist, which would ensure that they are prescribed to the correct patient population.
Evidence that specialist referrals are not occurring
Irrespective of the difference in details and information on specialist referral, it is evident that the asthma guidelines and strategy documents provide clear recommendations on when a referral should be sought. However, evidence suggests that there is a lack of specialist referrals or a failure to refer in practice. As highlighted previously, an evaluation of asthma deaths in the UK found that 20% of deaths investigated were related to avoidable factors associated with referrals.Citation39 A review of asthma management in the US, based on NAEPP guidelines, observed that the majority of patients were uncontrolled and only 22% of patients had visited a specialist regarding their asthma care. Approximately 50% of patients had never visited a specialist.Citation61 This is likely to be an important contributor to suboptimal management, given that specialist treatment can result in more favorable outcomes.Citation62 It has been shown in a retrospective review of a pediatric asthma population that only 44% visited an asthma specialist within 12 months of the initial ED visit, contrary to guideline recommendations.Citation63
Why are guidelines not adhered to and how can adherence be improved?
Besides documented differences in asthma guideline or strategy documents, the lack of knowledge on key referral guidelines and/or lack of implementation of these guidelines can ultimately impact the rate of referrals. Despite the obvious benefits of guidelines, evidence suggests that both the utilization of and adherence to these documents in the management of patients with asthma among HCPs are poor.Citation64–Citation70 A review of the possible reasons for poor adherence to asthma guideline recommendations highlighted the multifactorial barriers that physicians encounter, which could be grouped into three main areas: lack of physician knowledge about recommendations, inertia toward implementation of guidelines and clinical practice-related difficulties.
The lack of awareness or knowledge of guidelines by physicians is a barrier to physician adherence and implementation.Citation65–Citation70 In a study by Pinnock et al, the lack of knowledge of asthma guidelines among HCPs in the UK resulted in a low average score of 5.2 out of 11 in a web-based questionnaire that assessed their familiarity with guideline recommendations.Citation65 Aside from knowledge, physicians may also disagree with certain guidelines and, therefore, may not follow the recommendations.Citation69 Furthermore, external or practical barriers (e.g., lack of time and limited staff resources) can also impact guideline adherence.Citation70 It should also be noted that PCPs encounter patients with different asthma severities and control, and implementation of guideline recommendations needs to be modulated accordingly.Citation71 Other significant barriers such as lack of self-efficacy and lack of belief in outcomes of referrals have also been noted.Citation70
The lack of adherence to referral guidelines could be overcome with continuing medical education and discussions with colleagues.Citation72 A recent study demonstrated that a facilitator-led group self-assessment activity involving physicians led to improved quality of asthma care and adherence to guidelines.Citation73 Furthermore, interventions such as decision support tools, feedback and audit, and clinical pharmacy support could improve HCP adherence to asthma guidelines.Citation74 Finally, a recent study by Lugtenberg et al highlighted that to implement guidelines, suitable and accepted interventions that are appealing to the targeted physician group need to be identified.Citation75
It should be noted that, while guidelines and their implementation have an impact on referrals, there are other unassociated factors that can impact referrals, which have not been addressed in this review. The referral process, in general, may have breakdowns and inefficiencies in terms of decision making, coordination and access to specialty care.Citation76 For example, it has been shown that patients utilized other hospital facilities such as ED due to a defective referral system.Citation77 Specifically, the referral process has inconsistencies among the initiator and facilitatorCitation78 as well as the patient.Citation79 There could be financial disincentives to refer, especially with regards to physicians with ownership stakes in a practice.Citation80 There can also be an inadequate availability of specialists to provide advanced care to patients.Citation81
What should be done in the specialist setting?
The benefits for patients with asthma being referred to specialists should result in several positive outcomes: most importantly, the correct identification of disease to ensure appropriate treatment administration as well as the maintenance of symptom control, and a reduction in health care utilization and associated costs.Citation82
Several studies have demonstrated that when patients received care from an asthma specialist, the number of hospitalizations or the chance of these patients being hospitalized was reduced.Citation62,Citation83,Citation84 A recent study involving children with moderate or severe asthma suggested that improving referral and attendance at asthma specialty clinics (asthma, respiratory or allergy clinic) for these children had the potential to improve clinical outcomes.Citation63 Asthma specialists could also provide patients with a more enhanced education,Citation85 which is an essential component of asthma management and results in enhanced quality of life of patients.Citation83,Citation85 It has been reported that referral to a specialist led to more effective treatment as a higher percentage of specialists consider pharmacotherapies to be essential in asthma management compared with general practitioners.Citation86 Overall, specialist referral has been shown to be effective in improving asthma management.Citation71
To facilitate appropriate referrals, more frequent monitoring should be considered for patients with moderate and severe persistent asthma.Citation8 For example, in patients with an acute asthma attack, a respiratory specialist should follow-up patients admitted with a severe asthma attack for at least 1 year after the admission. Systematic assessment of patients with severe asthma has increasingly been taken up by severe asthma clinics,Citation87 which have expertise in diagnosis, assessment of severity, comorbidities, adherence and devices, and individualized treatment of these patients. Guidelines and strategy documentsCitation5,Citation8 now recommend that all patients with severe persistent asthma or a history of severe exacerbations requiring hospitalization be referred to an asthma specialist or a specialized asthma clinic.
Patients may have access to additional health care resources and treatments only available in the specialist setting, which could result in more appropriate treatment being administered and prevent the chronic use of oral corticosteroids by patients, thus reducing their exposure to the associated side effects of this treatment.Citation5 Furthermore, referring patients with severe or uncontrolled asthma to a specialist also provides a vital checkpoint whereby, when required for certain patients, there would be an appropriate escalation to additional therapies, for example, omalizumab and mepolizumab treatment for severe allergic asthma patients. Such treatments are expensive and involvement of a specialist would ensure that they are prescribed to the correct patient population. Overall, regular follow-up communication between specialists and PCPs should lead to informed assessment of disease control, optimized treatment strategies and improved clinical outcomes in patients.
Conclusion
The increasing prevalence of asthma has directly increased morbidity, mortality and the economic burden associated with this disease. Despite advances in asthma therapies and development of several guidelines and strategy documents recommending referral of certain patients to a specialist in order to improve their asthma control and reduce health resources utilization, the management of asthma remains suboptimal. To achieve appropriate referrals, there needs to be additional proper dissemination, translation, training, implementation and adherence of appropriate asthma guidelines that suit the health care landscape. Furthermore, an effective specialist referral system requires better coordination between health care providers and patients in different settings, which will allow for a better and more appropriate treatment for patients with asthma. The discrepancy across different asthma guidelines/strategy documents for specialist referrals also needs to be addressed through development of consensus-based strategies. In particular, optimizing referral processes in severe asthma should be given priority by the health care systems in order to minimize the significant morbidity and mortality associated with the disease. Ultimately, an improved process of specialist referrals would benefit patients with asthma with unmet needs in improving their asthma control and reducing health care resource utilization.
Acknowledgments
The authors thank Rahul Lad, PhD of Novartis for providing medical writing support, which was funded by Novartis Pharma AG in accordance with Good Publication Practice (GPP3) guidelines.
Disclosures
Professor David Price has board membership with Aerocrine, Amgen, AstraZeneca, Boehringer Ingelheim, Chiesi, Meda, Mundipharma, Napp, Novartis and Teva Pharmaceuticals; consultancy agreements with Almirall, Amgen, AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Meda, Mundipharma, Napp, Novartis, Pfizer, Teva Pharmaceuticals and Theravance; grants and unrestricted funding for investigator-initiated studies (conducted through Observational and Pragmatic Research Institute Pte Ltd) from Aerocrine, AKL Research and Development Ltd, AstraZeneca, Boehringer Ingelheim, British Lung Foundation, Chiesi, Meda, Mundipharma, Napp, Novartis, Pfizer, Respiratory Effectiveness Group, Takeda, Teva Pharmaceuticals, Theravance, UK National Health Service, Zentiva; payment for lectures/speaking engagements from Almirall, AstraZeneca, Boehringer Ingelheim, Chiesi, Cipla, GlaxoSmithKline, Kyorin, Meda, Merck, Mundipharma, Novartis, Pfizer, Skyepharma, Takeda and Teva Pharmaceuticals; payment for manuscript preparation from Mundipharma and Teva Pharmaceuticals; payment for the development of educational materials from Mundipharma and Novartis; payment for travel/accommodation/meeting expenses from Aerocrine, AstraZeneca, Boehringer Ingelheim, Mundipharma, Napp, Novartis and Teva Pharmaceuticals; funding for patient enrollment or completion of research from Chiesi, Novartis, Teva Pharmaceuticals and Zentiva; stock/stock options from AKL Research and Development Ltd which produces phytopharmaceuticals; owns 74% of the social enterprise Optimum Patient Care Ltd, UK and 74% of Observational and Pragmatic Research Institute Pte Ltd, Singapore; and is a peer reviewer for grant committees of the Efficacy and Mechanism Evaluation program, Health Technology Assessment, and Medical Research Council. Professor Leif Bjermer has, during the last 5 years, given lectures and/or attended advisory board for the following companies: AKL Research and Development Ltd, AstraZeneca, Airsonette, Chiesi, Boehringer, GlaxoSmith Kline, Meda, Merck, Mundipharma, Novartis and Teva. David A Bergin and Rafael Martinez are employees of Novartis.
References
- World Health OrganizationChronic respiratory diseases; Scope: asthma cited 2014. Available from: http://www.who.int/respiratory/asthma/scope/en/Accessed January 18, 2017
- BousquetJKhaltaevNGlobal surveillance, prevention and control of chronic respiratory diseases: a comprehensive approachWorld Health Organization2007 Available from: http://www.who.int/gard/publications/GARD%20Book%202007.pdfAccessed January 18, 2017
- CottiniMAseroRAsthma phenotypes todayEur Ann Allergy Clin Immunol20134511724
- LotvallJAkdisCABacharierLBAsthma endotypes: a new approach to classification of disease entities within the asthma syndromeJ Allergy Clin Immunol2011127235536021281866
- Global Initiative for AsthmaGlobal Strategy for Asthma Management and Prevention2016 Available from: www.ginasthma.orgAccessed January 18, 2017
- HolohanJManningPNolanDNational Asthma ProgrammeAsthma control in general practice, 2nd Edition, 2012 Available from: http://in.bgu.ac.il/en/fohs/communityhealth/Family/Documents/ASTHMA%20%20GINA%20%20%20Asthma-Control-General-Practice-Guidelines-2012.pdfAccessed January 18, 2017
- Ministry of Health, SingaporeManagement of Asthma2008 Available from: https://www.moh.gov.sg/content/moh_web/home/Publications/guidelines/cpg/2008/management_of_asthma.htmlAccessed January 18, 2017
- British Thoracic SocietyBTS/SIGN British guideline on the management of asthma2016 Available from: https://www.brit-thoracic.org.uk/standards-of-care/guidelines/btssign-british-guideline-on-the-management-of-asthma/Accessed January 18, 2017
- National Heart Lung and Blood InstituteNational Asthma Education and Prevention ProgramUS Department of Health and Human ServicesNational Institutes of HealthExpert panel report 3: Guidelines for the diagnosis and management of asthma; Full report 2007 Available from: https://www.nhlbi.nih.gov/files/docs/guidelines/asthgdln.pdfAccessed January 18, 2017
- Executive Committee GEMA 2009GEMA 2009 (Spanish guideline on the management of asthma)J Investig Allergol Clin Immunol201020Suppl 1159
- OhtaKYamaguchiMAkiyamaKJapanese guideline for adult asthmaAllergol Int201160211514521636963
- LallooUAinslieGWongMGuidelines for the management of chronic asthma in adolescents and adultsS Afr Pharm J20074952841
- BacharierLBBonerACarlsenKHDiagnosis and treatment of asthma in childhood: a PRACTALL consensus reportAllergy2008631534
- PapadopoulosNGArakawaHCarlsenKHInternational consensus on (ICON) pediatric asthmaAllergy201267897699722702533
- MotalaCGreenRJManjraAIPotterPCZarHJSouth African Childhood Asthma Working GGuideline for the management of chronic asthma in children–2009 updateS Afr Med J20099912 Pt 289891220455316
- HamasakiYKohnoYEbisawaMJapanese guideline for childhood asthma 2014Allergol Int201463333535625178176
- BatemanEDBousquetJKeechMLBusseWWClarkTJPedersenSEThe correlation between asthma control and health status: the GOAL studyEur Respir J2007291566217050557
- Rodriguez-TrigoGPlazaVPicadoCSanchisJEl tratamiento según la guía de la Global Initiative for Asthma (GINA) reduce la morbimortalidad de los pacientes con asma de riesgo vital [Management according to the Global Initiative for Asthma guidelines of patients with near-fatal asthma reduces morbidity and mortality]Arch Bronconeumol2008444192196 Spanish18423180
- GershonASVictorJCGuanJAaronSDToTPulmonary function testing in the diagnosis of asthma: a population studyChest201214151190119622030804
- National Guideline ClearinghouseAgency for Healthcare Research and QualityUS Department of Health and Human ServicesGuideline summary: Measuring fractional exhaled nitric oxide concentration in asthma: NIOX MINO, NIOX VERO and NObreath Available from: https://www.guideline.gov/summaries/summary/48533/measuring-fractional-exhaled-nitric-oxide-concentration-in-asthma-niox-mino-niox-vero-and-nobreathAccessed January 18, 2017
- BackerVSverrildASuppli UlrikCBødtgerUSeersholmNPorsbjergCDiagnostic work-up in patients with possible asthma referred to a university hospitalEur Clin Respir J2015227768
- BrozekGMFarnikMLawsonJZejdaJEUnderdiagnosis of childhood asthma: A comparison of survey estimates to clinical evaluationInt J Occup Med Environ Health201326690090924464568
- StupkaEdeShazoRAsthma in seniors: Part 1. Evidence for underdiagnosis, undertreatment, and increasing morbidity and mortalityAm J Med2009122161119114162
- CagneyMMacIntyreCRMcIntyrePBPeatJChildhood asthma diagnosis and use of asthma medicationAust Fam Physician200534319319615799674
- LindenSmithJMorrisonDDeveauCHernandezPOverdiagnosis of asthma in the communityCan Respir J200411211111615045041
- AaronSDVandemheenKLBouletLPOverdiagnosis of asthma in obese and nonobese adultsCMAJ2008179111121113119015563
- CaveAJAtkinsonLLAsthma in preschool children: a review of the diagnostic challengesJ Am Board Fam Med201427453854825002008
- Van SickleDMagzamenSMaennerMJCraneJCordenTEVariability in the labeling of asthma among pediatriciansPLoS One201384e6239823638066
- BousquetJHeinzerlingLBachertCPractical guide to skin prick tests in allergy to aeroallergensAllergy2012671182422050279
- BisaccioniCAunMVCajuelaEKalilJAgondiRCGiavina-BianchiPComorbidities in severe asthma: frequency of rhinitis, nasal polyposis, gastroesophageal reflux disease, vocal cord dysfunction and bronchiectasisClinics200964876977319690661
- StirlingRGChungKFSevere asthma: definition and mechanismsAllergy200156982584011551247
- PetersSPFergusonGDenizYReisnerCUncontrolled asthma: a review of the prevalence, disease burden and options for treatmentRespir Med200610071139115116713224
- HaughneyJPriceDKaplanAAchieving asthma control in practice: understanding the reasons for poor controlRespir Med2008102121681119318815019
- MyersTRGuidelines for asthma management: a review and comparison of 5 current guidelinesRespir Care200853675176718501029
- PriceDFletcherMvan der MolenTAsthma control and management in 8,000 European patients: the REcognise Asthma and LInk to Symptoms and Experience (REALISE) surveyNPJ Prim Care Respir Med2014122414009
- LuskinATChippsBERasouliyanLMillerDPHaselkornTDoren-baumAImpact of asthma exacerbations and asthma triggers on asthma-related quality of life in patients with severe or difficult-to-treat asthmaJ Allergy Clin Immunol Pract201425544552e1e225213047
- MillerMKLeeJHMillerDPWenzelSETENOR Study GroupRecent asthma exacerbations: a key predictor of future exacerbationsRespir Med2007101348148916914299
- DoughertyRHFahyJVAcute exacerbations of asthma: epidemiology, biology and the exacerbation-prone phenotypeClin Exp Allergy200939219320219187331
- Royal College of Physicians; National Review of Asthma Deaths2014Why asthma still kills: the National Review of Asthma Deaths (NRAD); Confidential Enquiry Report Available from: https://www.rcplondon.ac.uk/projects/outputs/why-asthma-still-killsAccessed January 18, 2017
- ColiceGMartinRJIsraelEAsthma outcomes and costs of therapy with extrafine beclomethasone and fluticasoneJ Allergy Clin Immunol20131321455423591272
- ZhangLPrietschSODucharmeFMInhaled corticosteroids in children with persistent asthma: effects on growthCochrane Database Syst Rev20147CD009471
- BroersenLHPereiraAMJørgensenJODekkersOMAdrenal insufficiency in corticosteroids use: systematic review and meta-analysisJ Clin Endocrinol Metab201510062171218025844620
- WeatherallMClayJJamesKPerrinKShirtcliffePBeasleyRDose-response relationship of inhaled corticosteroids and cataracts: a systematic review and meta-analysisRespirology200914798399019740259
- CummingRGMitchellPLeederSRUse of inhaled corticosteroids and the risk of cataractsN Engl J Med199733718149203425
- SuissaSKezouhAErnstPInhaled corticosteroids and the risks of diabetes onset and progressionAm J Med2010123111001100620870201
- PackeGEDouglasJGMcDonaldAFRobinsSPReidDMBone density in asthmatic patients taking high dose inhaled beclomethasone dipropionate and intermittent systemic corticosteroidsThorax19924764144171496498
- KellyHWVan NattaMLCovarRAEffect of long-term corticosteroid use on bone mineral density in children: a prospective longitudinal assessment in the childhood Asthma Management Program (CAMP) studyPediatrics20081221e53e6118595975
- McKeeverTHarrisonTWHubbardRShawDInhaled corticosteroids and the risk of pneumonia in people with asthma: a case-control studyChest201314461788179423990003
- SweeneyJPattersonCCMenzies-GowAComorbidity in severe asthma requiring systemic corticosteroid therapy: cross-sectional data from the Optimum Patient Care Research Database and the British Thoracic Difficult Asthma RegistryThorax201671433934626819354
- LougheedMDLeniereCDucharmeFMCanadian Thoracic Society 2012 guideline update: diagnosis and management of asthma in preschoolers, children and adults: executive summaryCan Respir J2012196e81e8823248807
- DahlRSystemic side effects of inhaled corticosteroids in patients with asthmaRespir Med200610081307131716412623
- ThomasMMurray-ThomasTFanTWilliamsTTaylorSPrescribing patterns of asthma controller therapy for children in UK primary care: a cross-sectional observational studyBMC Pulm Med2010102920470409
- ThomasMTurnerSLeatherDPriceDHigh-dose inhaled corticosteroid use in childhood asthma: an observational study of GP prescribingBr J Gen Pract20065653178879017007710
- BuhlRMarcoAGCohenDCanonicaGWEligibility for treatment with omalizumab in Italy and GermanyRespir Med20141081505624315468
- BusseWCorrenJLanierBQOmalizumab, anti-IgE recombinant humanized monoclonal antibody, for the treatment of severe allergic asthmaJ Allergy Clin Immunol2001108218419011496232
- HolgateSTChuchalinAGHebertJEfficacy and safety of a recombinant anti-immunoglobulin E antibody (omalizumab) in severe allergic asthmaClin Exp Allergy200434463263815080818
- SolerMMatzJTownleyRThe anti-IgE antibody omalizumab reduces exacerbations and steroid requirement in allergic asthmaticsEur Respir J200118225426111529281
- MolimardMBuhlRNivenROmalizumab reduces oral corticosteroid use in patients with severe allergic asthma: real-life dataRespir Med201010491381138520599369
- BrodlieMMcKeanMCMossSSpencerDAThe oral corticosteroid-sparing effect of omalizumab in children with severe asthmaArch Dis Child201297760460922685051
- WalshGMAn update on biologic-based therapy in asthmaImmunotherapy20135111255126424188679
- MurphyKRMeltzerEOBlaissMSNathanRAStoloffSWDohertyDEAsthma management and control in the United States: results of the 2009 Asthma Insight and Management surveyAllergy Asthma Proc2012331546422309716
- ZeigerRSHellerSMellonMHWaldJFalkoffRSchatzMFacilitated referral to asthma specialist reduces relapses in asthma emergency room visitsJ Allergy Clin Immunol1991876116011682045618
- AragonaEWangJScheckelhoffTAsthma specialty clinics decrease emergency department visits in inner-city children hospitalized for asthma exacerbationAm J Respir Crit Care Med2014189A3838
- FangXLiSGaoLZhaoNWangXBaiCA short-term educational program improved physicians’ adherence to guidelines for COPD and asthma in ShanghaiClin Transl Med2012111323369324
- PinnockHHolmesSLevyMLMcArthurRSmallIGroup UKGPAKnowledge of asthma guidelines: results of a UK General Practice Airways Group (GPIAG) web-based ‘Test your Knowledge’ quizPrim Care Respir J201019218018419826743
- PlazaVBolivarIGinerJOpinión, conocimientos y grado de seguimiento referidos por los profesionales sanitarios españoles de la Guía Española para el Manejo del Asma (GEMA). Proyecto GEMA-TEST [Knowledge of and attitudes and adherence to the Spanish Guidelines for Asthma Management (GEMA) among Spanish health care professionals: the GEMA test Project]Arch Bronconeumol2008445245251 Spanish18448015
- SunYHEunBWSimSYPoor adherence and reasons for nonadherence to the asthma guidelines among pediatricians in KoreaAsian Pac J Allergy Immunol2010282–314715421038784
- WisniveskyJPLorenzoJLyn-CookRBarriers to adherence to asthma management guidelines among inner-city primary care providersAnn Allergy Asthma Immunol2008101326427018814449
- LugtenbergMZegers-van SchaickJMWestertGPBurgersJSWhy don’t physicians adhere to guideline recommendations in practice? An analysis of barriers among Dutch general practitionersImplement Sci200945419674440
- CabanaMDLewisTCImproving physician adherence to asthma guidelinesJ Clin Outcomes Manage2001833546
- WechslerMEManaging asthma in primary care: putting new guideline recommendations into contextMayo Clin Proc200984870771719648388
- KangMKKimBKKimTWPhysicians’ preferences for asthma guidelines implementationAllergy Asthma Immunol Res20102424725320885909
- ElwardKBlackburnBPetersonLEGreenawaldMHagenMDImproving quality of care and guideline adherence for asthma through a group self-assessment moduleJ Am Board Fam Med201427339139824808118
- OkeloSOButzAMSharmaRInterventions to modify health care provider adherence to asthma guidelines: a systematic reviewPediatrics2013132351753423979092
- LugtenbergMBurgersJSHanDWestertGPGeneral practitioners’ preferences for interventions to improve guideline adherenceJ Eval Clin Pract201420682082624953439
- MehrotraAForrestCBLinCYDropping the baton: specialty referrals in the United StatesMilbank Q2011891396821418312
- WahabiHAAlziedanRAReasons behind non-adherence of healthcare practitioners to pediatric asthma guidelines in an emergency department in Saudi ArabiaBMC Health Serv Res20121222622846162
- BodenheimerTCoordinating care – a perilous journey through the health care systemN Engl J Med2008358101064107118322289
- MaultSMcDonoughBCurriePBurhanHReasons offered for nonattendance at a difficult asthma clinicThorax201267Suppl 2A187
- BarnettMLSongZLandonBETrends in physician referrals in the United States, 1999–2009Arch Intern Med2012172216317022271124
- Royal College of Physicians2003Allergy: the unmet need; A blueprint for better patient care Available from: http://www.bsaci.org/pdf/allergy_the_unmet_need.pdfAccessed January 18, 2017
- American College of Allergy Asthma and ImmunologyAsthma management and the allergist: better outcomes at lower costAllergist2008131
- EricksonSTolstykhISelbyJVMendozaGIribarrenCEisnerMDThe impact of allergy and pulmonary specialist care on emergency asthma utilization in a large managed care organizationHealth Serv Res2005405 Pt 11443146516174142
- MahrTAEvansR3rdAllergist influence on asthma careAnn Allergy19937121151208346862
- SchatzMZeigerRSMosenDImproved asthma outcomes from allergy specialist care: a population-based cross-sectional analysisJ Allergy Clin Immunol200511661307131316337464
- JansonSWeissKA national survey of asthma knowledge and practices among specialists and primary care physiciansJ Asthma200441334334815260468
- WarkPAHewMMaltbySMcDonaldVMGibsonPGDiagnosis and investigation in the severe asthma clinicExpert Rev Respir Med201610549150326967545
- National Asthma Council AustraliaThe Australian Asthma Handbook2015 Available from: http://www.asthmahandbook.org.auAccessed January 18, 2017
