Abstract
The increasing understanding of the molecular biology and the etiopathogenetic mechanisms of asthma helps in identification of numerous phenotypes and endotypes, particularly for severe refractory asthma. For a decade, the only available biologic therapy that met the unmet needs of a specific group of patients with severe uncontrolled allergic asthma has been omalizumab. Recently, new biologic therapies with different mechanisms of action and targets have been approved for marketing, such as mepolizumab. Other promising drugs will be available in the coming years, such as reslizumab, benralizumab, dupilumab and lebrikizumab. Moreover, since 2010, bronchial thermoplasty has been successfully introduced for a limited number of patients. This is a nonpharmacologic endoscopic procedure which is considered a promising therapy, even though several aspects still need to be clarified. Despite the increasing availability of new therapies, one of the major problems of each treatment is still the identification of the most suitable patients. This sudden abundance of therapeutic options, sometimes partially overlapping with each other, increases the importance to identify new biomarkers useful to guide the clinician in selecting the most appropriate patients and treatments, without forgetting the drug-economic aspects seen in elevated direct cost of new therapies. The aim of this review is, therefore, to update the clinician on the state of the art of therapies available for refractory asthma and, above all, to give useful directions that will help understand the different choices that sometimes partially overlap and to dispel the possible doubts that still exist.
Introduction
In the last few years, there has been an increased understanding of the etiopathogenetic mechanisms and phenotypes of asthma, particularly in the field of molecular biology and immunogenetics. Through this knowledge, it has been possible to develop new therapeutic approaches for the treatment of several asthmatic phenotypes. This is increasing the potential to meet the unmet needs of patients with unsatisfactory control of asthma. These patients suffer from the side effects of systemic steroids, and this may have a high impact on the economic resources because of frequent access to health services.
For over a decade, the only available biologic therapy has been omalizumab, a monoclonal antibody (mAb) which is targeted to anti-IgE and is used for a specific subpopulation of patients with uncontrolled IgE-mediated allergic asthma. For these patients, omalizumab has been very effective and has made it possible to change the clinical history of patients that would have otherwise been condemned to a limited and burdensome life due to their respiratory conditions.Citation1 For a long time, patients not eligible or not responsive to this treatment had to wait for the development of different therapies. Recently, new drugs and nonpharmacologic options are becoming available, showing encouraging results:
Biologic therapies with different mechanisms of action and targets. One of these molecules, the anti-interleukin 5 (anti-IL-5) mAb mepolizumab, has been recently approved for marketing. Other mAbs and new anti-inflammatory agents, such as prostaglandin receptor antagonists, will be available in the coming years.Citation2
Nonpharmacologic therapies, such as the bronchial thermoplasty (BT): This is still a controversial therapy because the efficacy is not always convincing and several aspects need to be clarified. This therapy may be applied on a large scale only after a clarification of all the concerns and doubts. As an invasive instrumental method, it may remain limited to centers with adequate experience and expertise. However, BT is showing extremely interesting results in terms of improving the quality of life (QoL) and reducing asthma exacerbation.Citation3
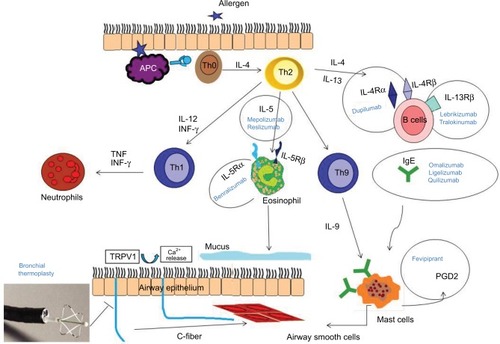
The availability of these new therapies enables addressing the patients to the most appropriate treatment and reducing therapeutic dropouts (). These important actions can be facilitated by the identification of new biomarkers.
Figure 1 Molecular targets of biologic drugs: action of the pathogenetic pathway of asthma at different levels.
In this review, we will describe the therapies previously mentioned focusing on the treatments that are already available or that are on the most advanced stage of development. We will discuss the overlapping aspects of some of these treatments and their application in clinical practice. In this regard, the future availability of new molecules that are specific for different targets is gaining attention, considering that these targets are sometimes present in the same phenotype. This will make it difficult for the clinical task to choose the most suitable and the most effective drug. Understanding the role of the various therapeutic options, their differences and similarities and the doubts that still exist will simplify the clinical decision-making process and will allow obtaining the best result for the patient.
From asthma phenotyping to personalized medicine
It is known that patients with asthma exhibit different levels of severity of their pathology, as well as several phenotypes and endotypes.Citation4 This subdivision is primarily based on several clinical and immunological characteristics: allergic and nonallergic or “T2-high” and “T2-low”. The main inflammatory phenotypes can be eosinophilic or noneosinophilic, where the latter is subdivided into neutrophil or pauci-granulocytic.Citation5
The identification and definition of the endotypes has started only recently.Citation6 This approach can be described as a single and distinct functional and physiopathologic mechanism that would enable a better use of existing drugs by identifying patient subgroups in order to find the more suitable treatment.Citation6 Each endotype includes several asthmatic phenotypes that can be considered as “phenotypic clusters”. However, further studies need to be preformed for a complete definition.Citation7,Citation8 The phenotype-based therapy will strongly benefit from the future discoveries of genomics, proteomics and transcriptomics which are the subdisciplines of systems biology that will contribute to making the customization of therapies a real possibility.Citation9
IgE-mediated asthma and anti-IgE mAbs
In IgE-mediated asthma, the exposure to allergens results in an increased inflammation and worsening of respiratory function parameters. The cardinal role of this process is carried out by the IgE antibodies that bind to high-affinity (FcεRI) and low-affinity (FcεRII or CD23) receptors on the surface of mast cells and basophils and lead to subsequent degranulation and release of mediators.Citation10
Omalizumab (Xolair®) is a murine mAb (MAE11) that has been applied in clinical practice since 2005 for the treatment of severe allergic refractory asthma in patients sensitized to perennial allergens with serum IgE levels in the range of 30–1500 IU/mL (; ). This biologic is constructed by a somatic cell hybridization method, whose main feature is to present a paratope capable of binding to FcεRI and FcεRII receptors of basophils, dendritic cells and mast cells.Citation11
Figure 2 Flowchart for the selection of different treatment options.
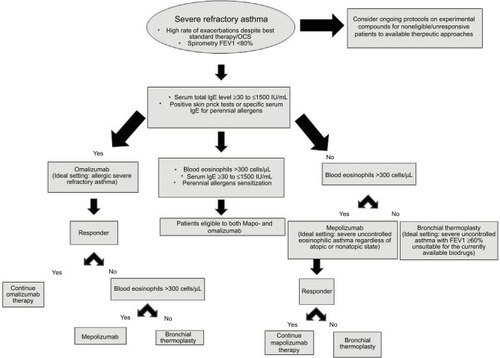
Table 1 Costs and treatment duration
To evaluate the effectiveness of omalizumab in patients with severe allergic uncontrolled asthma, several randomized clinical trials (RCTs) have been recently conducted. These studies demonstrated its efficacy and safety, with a significant reduction in the frequency of asthma exacerbations (up to 50%) and improvement in the QoL,Citation12 as well as reduction in the use of oral corticosteroids (OCSs).Citation12 The measurement of total IgE levels and body weight makes it possible to define its dosage, making this treatment the first to define a biologic treatment for asthma based on the use of a biomarker.Citation13 This treatment showed good efficacy even in patients with nonallergic asthma, most often treated for longer periods,Citation14 giving credit to the hypothesis that there is a local IgE production even without systemic sensitization.Citation15 Other studies have confirmed its effectiveness in inner city children with resistant asthma,Citation16 as well as in the prevention of seasonal exacerbations, thanks to a better interferon-α response to rhinoviruses.Citation17 Recently, omalizumab has also been approved for the treatment of spontaneous chronic urticaria,Citation18 while the increasing number of positive results on nasal polyposis provides new insights into this pathology that is often associated with asthma,Citation19 regardless of the atopic status.
Based on the current data, omalizumab is indicated for continuing the treatment for an indefinite period, as the IgE levels and the number of FcεRI receptors tend to increase 3–4 weeks after its suspension. In this regard, several studies have confirmed that discontinuation of this treatment results in a worsening of asthma control, especially in patients with higher levels of eosinophilia, periostin and FeNO. These molecules seem to better respond to omalizumab drug, but they are the first to decay after suspension of the treatment.Citation20,Citation21 Recent studies also show an increase in clinical efficacy in the long term (up to 9 years of follow-up),Citation22 with a favorable cost-effectiveness profile.Citation23
Considering the intrinsic limitations of omalizumab, the subsequent evolution could be the application of mAbs with greater avidity for IgE, such as quilizumab (RG7449). This is a newly humanized mAb that binds to the M1 segment of the membrane IgE and targets the B lymphocytes before they are activated to produce IgE. The Controlled on Inhaled Steroids and a Second Controller trial is a 36-week, Phase II, randomized, placebo-controlled, double-blind study whose results have been recently published.Citation24 These results show that quilizumab has a good safety profile and is associated with specific decrease in IgE serum levels up to 40%, without significant impact on exacerbations, respiratory functions and symptoms.Citation25
Two other RCTs were designed to determine the safety, pharmacokinetics and efficacy of quilizumab in patients with allergic rhinitis.Citation26,Citation27 In both studies, the treatment was tolerated and showed a significant reduction in persistent specific serum IgE up to 6 months after withdrawal, also blocking the production of new IgE after allergen challenge and reducing the eosinophils in induced sputum by over 50% compared to placebo.Citation28
Another anti-IgE mAb is QGE031 (ligelizumab), a novel anti-IgE agent whose first studies showed a greater suppression of free IgE than omalizumab, including those with higher IgE levels.Citation29
Despite the promising initial data, the Phase II study CQGE031B2201 failed to meet the primary objective of demonstrating superiority of QGE031 versus placebo (Novartis Pharmaceuticals, unpublished data).Citation30 Consequently, two other related Phase II trials were suspended following the failure of the core study.
Even if the premises were not positive, in a recent double-blind, parallel-group, multicenter study, 37 patients with mild allergic asthma were randomized to subcutaneous (SC) omalizumab, placebo or QGE031 at 24, 72 or 240 mg every 2 weeks for 10 weeks.Citation31 Inhaled allergen challenge and skin tests were performed before dosing at 6, 12 and 18 weeks, and blood samples were collected until 24 weeks after the first dose. Ligelizumab appears to be more effective than omalizumab in terms of skin and inhalation response, demonstrating that it may be the most effective successor to omalizumab.
Eosinophils and IL-5
The eosinophilic granulocyte maturation, their recruitment and survival in the respiratory tract are determined by IL-3 and granulocyte–macrophage colony-stimulating factor, but above all by IL-5, which is the most important IL for the determination of eosinophilic airway inflammation. IL-5 induces the final differentiation of B cells activated into antibody-forming cells and enhances the proliferation and differentiation of the eosinophil precursors into mature eosinophils.Citation32 Murine experimental models showed that it may be involved in airway remodeling, so administration of IL-5 antibodies almost completely blocks the peribronchial and subepithelial fibrosis induced by inhaled allergens.Citation33 Eosinophils play a key role in several chronic respiratory diseases and can affect their severity.Citation32 In asthma, eosinophilia is present in about 40%–60% of cases, with a direct correlation between the severity of the disease and the presence of blood eosinophils and sputum.Citation34
Eosinophilia is associated with a wide variety of conditions such as asthma, atopic diseases, viral infections, hypersensitivity to drugs and neoplastic conditions. For these reasons, several anti-IL-5 mAbs such as mepolizumab (Nucala®), reslizumab (Cinqair®) and benralizumab have been studied.
Mepolizumab is a humanized IgG1 nonglycosylated IgG1 antibody that binds to IL-5 and prevents the binding of IL-5 to its receptor. Early studies involved the application of mepolizumab for the treatment of idiopathic hypereosinophilic syndromeCitation35 and Churg–Strauss syndrome or eosinophilic granulomatosis and polyangiitis, where a significant reduction in the use of OCS and a better control of the disease was observed.Citation35 Other studies demonstrated that this molecule was ineffective in terms of improvement of respiratory function parameters (bronchial hyperresponsiveness, FEV1, PEF)Citation36 and better asthma control (decreased rate of exacerbation) despite a decline in eosinophils in the blood and sputum.Citation37 Based on later observations, described below, it was clear that there was a selection bias, concerning the blood eosinophilia and the severity of asthma criteria. The patients were not selected on the basis of blood eosinophils.
Two subsequent RCTs clearly showed how initially intravenous and SC mepolizumab could reduce the need for steroids and the number of exacerbations in patients with severe asthma with eosinophils >300 cells/μL, with less visible but positive effects on respiratory function parameters.Citation38,Citation39 A third registrative RCT confirmed the efficacy of mepolizumab in terms of reducing exacerbations, improving the QoL calculated by the Asthma Control Questionnaire 5 questionnaire and, above all, having an average reduction of 50% in the dose of OCS.Citation40 A recent MUSCA trial (mepolizumab add-on therapy on health-related quality of life and markers of asthma control in severe eosinophilic asthma) has confirmed that this drug significantly improved the health-related QoL in patients with severe eosinophilic asthma and had a security profile similar to placebo.Citation41 In 2015, mepolizumab was approved by the US Food and Drug Administration (FDA) and the European Medicines Agency for the treatment of severe eosinophilic asthma at a dose of 100 mg SC every 4 weeks (; ).Citation42,Citation43,Citation45
A second mAb anti-IL-5 is reslizumab. This drug has been studied in patients with uncontrolled eosinophilic asthma with a blood eosinophil level >400 cells/μL, showing a meaningful reduction of sputum eosinophil count, an improvement in QoL, FEV1 and control of the disease in terms of reducing exacerbations.Citation44 The administration of reslizumab showed improved symptoms and QoL, even in case of nasal polyposis.Citation44 The limitation of this drug may be the intravenous administration, since it is FDA approved only with this indication.Citation45
Benralizumab (MEDI-563) is an IgA1 mAb that binds the epitope on the α-subunit of the IL-5 receptor. It has been shown to reduce blood eosinophils and their precursors through the induction of antibody-mediated cell cytotoxicity (ADCC).Citation46 Therefore, its molecular mechanism is completely different from that of mepolizumab. The benralizumab constant region (Fc) is afucosylated, leading to greater affinity for the Fc-gamma III receptor (FcγRIIIa) on the surface of the mast cells, basophils and natural killer cells, through which it induces ADCC on eosinophils and basophils.Citation47 This involves a nearly complete depletion of eosinophils in sputum and tissues (90% and 96%, respectively) and a total disappearance in the bone marrow and blood.Citation48 In Phase I and II RCTs on patients with severe eosinophilic asthma and peripheral eosinophils >300 cells/μL, SC benralizumab showed promising results, especially in terms of reducing EDN and ECP inflammation and inflammatory mediators as well as causing a significant reduction in blood eosinophils.Citation49,Citation50
The main difference between benralizumab and other IL-5 mAb drugs is that benralizumab is independent of the circulating level of IL-5, which tends to increase during asthma exacerbations. The almost total depletion of eosinophils through ADCC prevents the effects caused by the activation by other related cytokines (IL-3 and granulocyte–macrophage colony-stimulating factor) that share the same receptor through the β subunit. The absence of fucose sugar residue in the molecular structure of benralizumab results in a much higher affinity for the FcγRIIIa receptor, overcoming the inhibitory effects of serum blocking IgGs.Citation47 These features resulted in excellent efficacy data in terms of reduction of exacerbation rate and improvement in FEV1,Citation51,Citation52 significant reduction (75%) of the OCSCitation53 average dose and a clear response after the first dose.Citation54
Block of IL-4/IL-13
IL-4 and IL-13 are pleiotropic T-helper type 2 cytokines with a common pathway frequently associated with asthma and other atopic diseases such as atopic dermatitis.Citation55 The main functions of IL-4 and IL-13 are the activation of the IgE isotype switch by plasma cells, the proliferation of T lymphocytes, especially Th2, in stimulation of expression of some adhesion molecules on endothelial cells (especially VCAM-1) and stimulation of smooth bronchial muscle contractility. High levels of IL-13 are found in sputum and bronchial biopsies of patients with severe asthma, often not responsive to the use of systemic and inhaled steroids. This confirms the role of this cytokine in corticosteroid resistance.Citation56 Some interesting mAbs in development aim to target these fundamental cytokines such as dupilumab, lebrikizumab and tralokinumab.
The mAb dupilumab inhibits the biologic effect of both IL-4 and IL-13 by preventing their interaction with IL-4 receptor α subunit. Recent studies have shown that this drug results in a significant decrease in exacerbations and better control of symptoms and pulmonary function, with concomitant reduction of inflammatory biomarkers related to the activity of Th2 lymphocytes, but with effects independent of eosinophils in serum in patients with severe refractory asthma.Citation57 Recent trials on dupilumab administered SC as an add-on therapy at dose ranging from 100 to 300 mg showed an increase in pulmonary function and a significant reduction in severe exacerbations in patients with persistent asthma, without any difference in counting (±300 cells/μL) but with a favorable safety profile.Citation58,Citation59 Dupilumab also confirmed a marked reduction in the biomarkers associated with Th2-driven inflammation (TARC levels, eotaxin-3, FeNo).Citation59
Lebrikizumab (MILR1444A) is another humanized mAb having a specific target of IL-13. Lebrikizumab administered SC at doses of 125, 250 and 500 mg every 4 weeks showed an improved pulmonary function in extensive Phase II studies in patients with severe refractory asthma, with improved symptom control and reduced exacerbation, especially in the group with allergic phenotype with high levels of periostin and exogenous nitric oxide (FeNO).Citation60 The improvement in FEV1 was also more apparent in the group with higher levels of periostin and FeNO, confirming the hypothesis that IL-13-driven phenomena are clinically important in these patients.Citation61,Citation62 Subsequently, two identical 52-week, Phase III studies had been conducted to assess the efficacy and safety of lebrikizumab in patients with uncontrolled asthma (LAVOLTA I and II). LAVOLTA I met its primary endpoint, showing a significant reduction in the rate of asthma exacerbations in people with higher levels of serum periostin or blood eosinophils. This study also showed a significant improvement in lung function. Unfortunately, these positive findings were not confirmed in LAVOLTA II, which did not show a significant reduction in asthma exacerbations.Citation63
Another anti-IL-13 mAb is tralokinumab, whose development is facing major difficulties because the data that emerged from two Phase IIb RCTs are still not encouraging. Indeed, tralokinumab at doses ranging from 150 to 600 mg given every 2 weeks or every 4 weeks did not reduce asthma exacerbation rates or improve ACQ6 score in patients with uncontrolled asthma compared to placebo, although improvements in FEV1 were observed in patients receiving the drug every 2 weeks.Citation64,Citation65 A post hoc analysis in the group of patients with higher IL-13 levels (10 μg Ml-1) at the time of admission to the study showed numerically greater improvements in FEV1 than in subjects whose values were lower than these thresholds, suggesting that the presence of residual IL-13 was associated with a higher response in FEV1.Citation65
Antagonist of the prostaglandin D2 receptor
Prostaglandin D2 (PGD2) is a prostanoid produced mostly by the mast cells in allergic diseases. The PGD2-induced vasodilatation and the subsequent increase in permeability are involved in inflammatory allergies.Citation66 Prostanoid (DP) receptors and the homologous receptor mutant molecule expressed on Th2 (CRTH2) cells have been shown to be the major PGD2-related receptors that have central roles in the regulation of the functions of several cells crucial in allergic diseases.Citation66
Fevipiprant (QAW039) is an antagonist of PGD2 receptor CRTH2, which is expected to provide benefit in asthma by binding to CRTH2 receptors on eosinophils, basophils and T lymphocytes in the blood and tissues, thus inhibiting the migration and activation of these cells into the airway tissues and blocking the PGD2-driven release of Th2 cytokines.Citation67 QAW039 is an interesting and unique molecule with ongoing Phase II and III RCTs that are recruiting patients with severe refractory allergic asthma Steps 4–5 Global Initiative for Asthma 2016. Fevipiprant, compared to all other mAbs, has the advantage of daily oral administration at doses up to 500 mg. Preliminary data confirm a good safety profile and improvement of FEV1, especially in patients with more severe obstruction.Citation68 Another Phase II study in patients with uncontrolled allergic asthma showed no improvement in pulmonary function. However, a subgroup analysis revealed that patients with impaired respiratory function (FEV1 <70%) had improved pulmonary function and asthma control when treated with QAW039.Citation69 In a subsequent randomized, single-center, double-blind, parallel-group, placebo-controlled study on 61 patients with moderate-to-severe asthma, fevipiprant reduced eosinophilic airways and sputum inflammation and was well tolerated, confirming the good perspective of this drug for the near future.Citation70
Not only biologic therapies: BT
BT is an endoscopic procedure approved by the FDA in 2010 for the treatment of severe refractory asthma. This method is essentially based on the delivery of 65° radiofrequency by a disposable catheter with 2.0 mm diameter introduced into the fibrobroncoscope operating channel (Alair®).Citation70 BT is a one-time procedure that is completed after three treatments performed ~20 days apart, and several studies have demonstrated its long-term safety and effectiveness in terms of reducing serious exacerbations, improving health-related QoL and reducing the number of working/school days lost for asthma.Citation72–Citation74 BT should always be used as an add-on treatment with the best standard care (). Due to its complex procedure, BT should always be performed in centers with adequate preparation and experience to handle possible intra- and postprocedure adverse events.Citation75 Moreover, the significant increase in direct costs could represent another limiting factor. However, these costs are lower if compared with those associated with the use of biologic therapies for serious asthma (in particular, omalizumab), especially for long-term treatments, as demonstrated by several studies.Citation76,Citation77 There are still many open questions about the mechanism of action, selection of patients and their management. However, a reduction of airway smooth muscle and inflammation has been observed,Citation78,Citation79 also with regard to a possible reduction of blood eosinophils after BT.Citation80 Some evidence reveals the possible effects of BT on the small airways, which is very important in asthma pathogenesis.Citation81 It has also been argued that BT may influence the neuroendocrine epithelial cells, bronchial nerve endings, destruction of TRPV1 nerve receptors and the type-C unmyelinated fibers in the mucosa by interrupting central and local reflexes responsible for the activation of bronchospasm and bronchial hyperreactivity.Citation82 All these aspects go beyond what was first hypothesized about the mechanisms of action, but they need further confirmation. However, several questions remain open regarding the phenotyping of patients and the long-term effects, but further improvements and clarifications will be expected in the next few years.
Based on the literature data and treatments available, BT may be already proposed for several patients: 1) patients with FEV1 ≥60% of the predicted,Citation71 unsuitable for the currently available biodrugs (omalizumab or mepolizumab); 2) patients responsive to these mAbs and 3) patients who do not want to undergo biologic therapies with an indefinite duration (). There are, however, studies on small patient groups such as Doeing et al’s work on eight patients with severe functional impairment (FEV1 between 52% and 37% of the predicted), where BT was found to be effective in five of them without causing worsening of respiratory function.Citation83 BT may also be indicated in patients with frequent exacerbations and hospitalization, regardless of T1 or T2 phenotypeCitation84 or respiratory function. Another potentially suitable subgroup could be composed of patients with severe steroid-resistant refractory asthma.Citation85
Growing role of biomarkers in asthma phenotyping and for the drug choice
In clinical practice, asthma management and its follow-up are mainly based on respiratory function parameters that determine hyperreactivity and bronchial obstruction. However, these data do not always correlate with the levels and type of respiratory inflammation. Fibrobronchoscopy and bronchoalveolar lavage are the gold standard for defining inflammation, but are invasive and not routinely applicable.Citation86
Omalizumab has been helping the definition of asthma phenotypes and endotypes, thanks also to the identification of new and useful biomarkers to guide the choice of treatment. Therefore, for omalizumab, the selection of patients and the predictability of drug response are still based on the total free IgE level. In this regard, it is demonstrated that a high percentage of patients with severe bronchial obstruction often have total IgE values >400 IU/mLCitation87 and that low IgE levels, on the other hand, usually have little therapeutic benefit with omalizumab.Citation88 Although lower baseline levels of total IgE were potentially predictive of poor response to omalizumab as emerged from the INNOVATE study, subsequent pooled analysis did not clearly confirm this conclusion and showed treatment benefits regardless of the IgE levels.Citation88
As for other possible biomarkers, the level of blood eosinophilia is a parameter that effectively correlates with the response to anti-IL-5 mAbs, especially with >300 cells/μL or better than 500 cells/μL,Citation38 while the FeNO reliability data are still partially controversial in determination and follow-up of eosinophilic inflammation.Citation89 However, the EXTRA study showed that high values of blood eosinophilia and FeNO can positively predict the response to omalizumab,Citation20 and patients with these phenotypic characteristics lose treatment benefits more quickly in case of its withdrawal, as demonstrated by the recent XPORT study.Citation21
All these aspects increase the difficulty in choosing from one of the two classes of biologics in case of overlapping, although several efficacy and safety data over the long-term use of omalizumab would favor this drug.Citation22 Currently, no comparative direct data are available between anti-IgE and anti-IL5; so, considering a possible partial overlap between omalizumab- and mepolizumab-ineligible patients, head-to-head comparative trials will be needed to evaluate the efficacy of the two classes of mAbs. For this reason, switch studies from omalizumab to mepolizumab are currently on recruitment. The aim will be to compare these two drugs in terms of improving the QoL and reducing the frequency of clinically significant exacerbations, which may provide additional data to select the most suitable drug.Citation90 From a recent meta-analysis study, it has been found that the observed heterogeneity and the different selection criteria for the use of the two drugs do not allow to formulate definitive recommendations for the preferential use of omalizumab versus mepolizumab, and no significant differences in effectiveness were detected.Citation91
However, it is important to remember that the atopic condition and the total IgE level at baseline do not affect the efficacy of mepolizumab, as demonstrated by a subanalysis of the DREAM trial.Citation39 A recent post hoc analysis of patients treated with mepolizumab after an ineffective omalizumab treatment and enrolled in the DREAM, MENSA and SIRIUS studies showed that these patients positively responded to mepolizumab, regardless of the prior use of omalizumab. This result confirms and reinforces the conclusions of previous studies.Citation92
An extensive interventional cross-sectional study on a cohort of 670 patients was intended to estimate the potential overlap of patients eligible for treatment with mepolizumab and those eligible for treatment with omalizumab and/or reslizumab. Preliminary data showed a 53% potential overlap between mepolizumab and omalizumab and a 16.8% overlap with reslizumab, confirming that common eligibility is often present between the two drug classes.Citation93
Promising biomarkers such as periostin will be able to help the clinician. Periostin is an extracellular matrix protein that is also associated with eosinophilic flogosis and is primarily studied to predict the response and monitor the biodrugs such as lebrikizumab and omalizumab.Citation94 However, the correlation with eosinophilic inflammation was not always univocal;Citation95 therefore, additional data are still needed. In addition, it has been shown that periostin is not just an indicator of type 2 inflammation activated by IL-13. Patients with asthma and high periostin levels have unique characteristics, including eosinophilia, high levels of nitric oxide, acetylsalicylic acid intolerance, nasal polyposis and late-onset asthma.Citation96 These features are probably correlated with the involvement of periostin in bronchial remodeling, and this protein may also be associated with poor response to corticosteroids, probably due to tissue remodeling.Citation93 In addition, periostin has an accurate predictive power of response to mAbs such as lebrikizumab, tralokinumab and omalizumab, especially if combined with other parameters such as the level of blood eosinophilia and FeNO.Citation20,Citation88
The increasing interest about the identification of biomarkers capable of predicting the effectiveness that guides the identification and choice of innovative therapies is represented by the Unbiased BIOmarkers for the Prediction of Respiratory Disease Outcomes project. This project is funded by the European Commission Innovative Medicines Initiative of the European Union, which has proposed a systematic algorithmic approach to patients with severe asthma.Citation97
Conclusion
The increase in therapeutic options for the treatment of asthma has made the subject of phenotyping and personalized therapy very timely. However, it is difficult to choose the right therapeutic target because of the complexity of pathogenesis, severity and inflammatory pathways. After the introduction of omalizumab, BT and mepolizumab and the advent of other biologically active drugs, the multimodal approach of the management of patients with severe asthma becomes a key point. This is due to the possible overlap between anti-IgE and anti-IL-5 mAbs (as could be the case in patients with allergy and concomitant hypereosinophilic phenotype) and the difficulty in identification of patients eligible for BT.
The development and application of a broader scale of reproducible, noninvasive, cheap and validated biomarkers will make the treatment selection easier, but those already available, if properly used, can guide the clinician to the right therapeutic option for the right patient.
Pharmacoeconomic aspects must also be considered due to the high direct cost of new therapies. These costs are partially balanced by a better control of asthma; however, they should empower the clinician to the best positioning of current and future treatments. All these actions will avoid waste of valuable resources, especially in the actual socioeconomic context.
Disclosure
Francesco Menzella participated in contracted research and the clinical trials for Novartis, Sanofi and GlaxoSmithKline. Nicola Facciolongo served as a consultant for Boston Scientific. The other authors report no conflicts of interest in this work.
References
- AbrahamIAlhossanALeeCS“Real-life” effectiveness studies of omalizumab in adult patients with severe allergic asthma: systematic reviewAllergy201671559361026644231
- MenzellaFLusuardiMMontanariGClinical usefulness of mepolizumab in severe eosinophilic asthmaTher Clin Risk Manag20161290791627354806
- TrivediAPavordIDCastroMBronchial thermoplasty and biological therapy as targeted treatments for severe uncontrolled asthmaLancet Respir Med20164758559227230825
- WenzelSSevere asthma: from characteristics to phenotypes to endotypesClin Exp Allergy201242565065822251060
- ChungKFAsthma phenotyping: a necessity for improved therapeutic precision and new targeted therapiesJ Intern Med2016279219220426076339
- LotvallJAkdisCABacharierLBAsthma endotypes: a new approach to classication of disease entities within the asthma syndromeJ Allergy Clin Immunol2011127235536021281866
- MooreWCMeyersDAWenzelSEIdentification of asthma phenotypes using cluster analysis in the severe asthma research programAm J Respir Crit Care Med2010181431532319892860
- SimpsonATanVYWinnJSvensenMBeyond atopy: multiple patterns of sensitization in relation to asthma in a birth cohort studyAm J Respir Crit Care Med2010181111200120620167852
- O’NeilSELundbäckBLötvallJProteomics in asthma and COPD phenotypes and endotypes for biomarker discovery and improved understanding of disease entitiesJ Proteomics201175119220122037230
- SamitasKDelimpouraVZervasEAnti-IgE treatment, airway inflammation and remodelling in severe allergic asthma: current knowledge and future perspectivesEur Respir Rev20152413859460126621973
- HumbertMBusseWHananiaNAOmalizumab in asthma: an update on recent developmentsJ Allergy Clin Immunol Pract20142552553625213045
- RodrigoGJNeffenHCastro-RodriguezJAEfficacy and safety of subcutaneous omalizumab vs placebo as add-on therapy to corticosteroids for children and adults with asthma: a systematic reviewChest20111391283520688929
- LowePJTannenbaumSGautierARelationship between omalizumab pharmacokinetics, IgE pharmacodynamics and symptoms in patients with severe persistent allergic (IgE-mediated) asthmaBr J Clin Pharmacol2009681617619660004
- MenzellaFPiroRFacciolongoNLong-term benefits of omalizumab in a patient with severe non-allergic asthmaAllergy Asthma Clin Immunol201171921609447
- ForesterJPCalabriaCWLocal production of IgE in the respiratory mucosa and the concept of entopy: does allergy exist in nonallergic rhinitis?Ann Allergy Asthma Immunol2010105424925520934624
- BusseWWMorganWJGergenPJRandomized trial of omalizumab (anti-IgE) for asthma in inner-city childrenN Engl J Med201136411005101521410369
- TeachSJGillMATogiasAPreseasonal treatment with either omalizumab or an inhaled corticosteroid boost to prevent fall asthma exacerbationsJ Allergy Clin Immunol201513661476148526518090
- Giménez-ArnauAMToubiEMarslandAMMaurerMClinical management of urticaria using omalizumab: the first licensed biological therapy available for chronic spontaneous urticariaJ Eur Acad Dermatol Venereol201630Suppl 52532
- BachertCGevaertPHellingsPBiotherapeutics in chronic rhinosinusitis with and without nasal polypsJ Allergy Clin Immunol Pract2017 pii:S2213-2198(17)30321-5. [Epub ahead of print]
- HananiaNAWenzelSRosénKExploring the effects of omalizumab in allergic asthma: an analysis of biomarkers in the EXTRA studyAm J Respir Crit Care Med2013187880481123471469
- LedfordDBusseWTrzaskomaBA randomized multicenter study evaluating Xolair persistence of response after long-term therapyJ Allergy Clin Immunol20171401162169.e227826098
- MenzellaFGaleoneCFormisanoDReal-life efficacy of omalizumab after 9 years of follow-upAllergy Asthma Immunol Res20179436837228497924
- MenzellaFFacciolongoNPiroRClinical and pharmacoeconomic aspects of omalizumab: a 4-year follow-upTher Adv Respir Dis201262879522323442
- GenentechA Study of MEMP1972A in Patients with Allergic Asthma Inadequately Controlled on Inhaled Steroids and A Second Controller (COSTA)2012 Available from: https://clinicaltrials.gov/ct2/show/NCT01582503Accessed June 6, 2017 ClinicalTrials.gov Identifier: NCT01582503Accessed June 6, 2017
- HarrisJMMaciucaRBradleyMSA randomized trial of the efficacy and safety of quilizumab in adults with inadequately controlled allergic asthmaRespir Res20161712926993628
- GenentechA Study to Investigate the Safety, Tolerability, and Phar-macokinetics of MEMP1972A in Patients with Allergic Rhinitis2010 Available from: https://clinicaltrials.gov/ct2/show/NCT01160861Accessed June 6, 2017 ClinicalTrials.gov Identifier: NCT01160861Accessed June 6, 2017
- GenentechA Study of MEMP1972A in the Prevention of Allergen-Induced Airway Obstruction in Patients with Mild Asthma (SOLARIO)2010 Available from: https://clinicaltrials.gov/ct2/show/NCT01196039Accessed June 6, 2017 ClinicalTrials.gov Identifier: NCT01196039Accessed June 6, 2017
- GauvreauGMHarrisJMBouletLPTargeting membrane-expressed IgE B cell receptor with an antibody to the M1 prime epitope reduces IgE productionSci Transl Med20146243243ra85
- ArmJPBottoliISkerjanecAPharmacokinetics, pharmacodynamics and safety of QGE031 (ligelizumab), a novel high-affinity anti-IgE antibody, in atopic subjectsClin Exp Allergy201444111371138525200415
- Novartis PharmaceuticalsEfficacy and Safety of QGE031 versus Placebo and Omalizumab in Patients Aged 18–75 Years With Asthma2012 Available from: https://clinicaltrials.gov/ct2/show?term=CQGE031B2201Accessed July 31, 2017 NLM Identifier: NCT01716754Accessed July 31, 2017
- GauvreauGMArmJPBouletLPEfficacy and safety of multiple doses of QGE031 (ligelizumab) versus omalizumab and placebo in inhibiting allergen-induced early asthmatic responsesJ Allergy Clin Immunol201613841051105927185571
- StoneKDPrussinCMetcalfeDDIgE, mast cells, basophils, and eosinophilsJ Allergy Clin Immunol20101252 Suppl 2S73S8020176269
- TanakaHKomaiMNagaoKRole of interleukin-5 and eosinophils in allergen-induced airway remodeling in miceAm J Respir Cell Mol Biol20043116214975941
- WardlawAJBrightlingCEGreenRWoltmannGBraddingPPavordIDNew insights into the relationship between airway inflammation and asthmaClin Sci (Lond)2002103220121112149112
- LegrandFKlionADBiologic therapies targeting eosinophils: current status and future prospectsJ Allergy Clin Immunol Pract20153216717425754717
- LeckieMJten BrinkeAKhanJEffects of an interleukin-5 blocking monoclonal antibody on eosinophils,airway hyper-responsiveness, and the late asthmatic responseLancet200035692482144214811191542
- Flood-PagePMenzies-GowAPhippsSAnti-IL-5 treatment reduces deposition of ECM proteins in the bronchial subepithelial basement membrane of mild atopic asthmaticsJ Clin Invest200311271029103614523040
- OrtegaHGLiuMCPavordIDMepolizumab treatment in patients with severe eosinophilic asthmaN Engl J Med2014371131198120725199059
- PavordIDKornSHowarthPMepolizumab for severe eosinophilic asthma (DREAM): a multicentre, double-blind, placebo- controlled trialLancet2012380984265165922901886
- BelEHWenzelSEThompsonPJOral glucocorticoid-sparing effect of mepolizumab in eosinophilic asthmaN Engl J Med2014371131189119725199060
- ChuppGLBradfordESAlbersFCEfficacy of mepolizumab add-on therapy on health-related quality of life and markers of asthma control in severe eosinophilic asthma (MUSCA): a randomised, double-blind, placebo-controlled, parallel-group, multicentre, phase 3b trialLancet Respir Med20175539040028395936
- Available from: http://www.fda.gov/NewsEvents/Newsroom/PressAn-nouncements/ucm471031.htmAccessed May 27, 2017
- Available from: http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/003860/human_med_001933.jsp&mid=WC0b01ac058001d124Accessed May 27, 2017
- CastroMMathurSHargreaveFReslizumab for poorly controlled, eosinophilic asthma: a randomized, placebo-controlled studyAm J Respir Crit Care Med2011184101125113221852542
- Available from: https://www.fda.gov/NewsEvents/Newsroom/Pres-sAnnouncements/ucm491980.htmAccessed May 28, 2017
- KolbeckRKozhichAKoikeMMEDI-563, a humanized anti-IL-5 receptor alpha mAb with enhanced antibody-dependent cell-mediated cytotoxicity functionJ Allergy Clin Immunol201012561344135320513525
- MenzellaFLusuardiMGaleoneCFacciolongoNZucchiLThe clinical profile of benralizumab in the management of severe eosinophilic asthmaTher Adv Respir Dis201610653454827612492
- LavioletteMGossageDLGauvreauGEffects of benralizumab on airway eosinophils in asthmatic patients with sputum eosinophiliaJ Allergy Clin Immunol201313251086109623866823
- GhaziATrikhaACalhounWJBenralizumab – a humanized mAb to IL-5Ralpha with enhanced antibody-dependent cell-mediated cytotoxicity – a novel approach for the treatment of asthmaExpert Opin Biol Ther201212111311822136436
- CastroMWenzelSEBleeckerERBenralizumab, an anti-interleukin 5 receptor alpha monoclonal antibody, versus placebo for uncontrolled eosinophilic asthma: a phase 2b randomised dose-ranging studyLancet Respir Med201421187989025306557
- FitzGeraldJMBleeckerERNairPBenralizumab, an anti-interleukin-5 receptor α monoclonal antibody, as add-on treatment for patients with severe, uncontrolled, eosinophilic asthma (CALIMA): a randomised, double-blind, placebo-controlled phase 3 trialLancet2016388100562128214127609406
- BleeckerERFitzGeraldJMChanezPEfficacy and safety of benralizumab for patients with severe asthma uncontrolled with high-dosage inhaled corticosteroids and long-acting β2-agonists (SIROCCO): a randomised, multicentre, placebo-controlled phase 3 trialLancet2016388100562115212727609408
- NairPWenzelSRabeKFOral glucocorticoid-sparing effect of benralizumab in severe asthmaN Engl J Med2017 Epub ahead of print
- NowakRMParkerJMSilvermanRAA randomized trial of benralizumab, an antiinterleukin 5 receptor α monoclonal antibody, after acute asthmaAm J Emerg Med2015331142025445859
- AgrawalS1TownleyRGRole of periostin, FENO, IL-13, lebrikzumab, other IL-13 antagonist and dual IL-4/IL-13 antagonist in asthmaExpert Opin Biol Ther201414216568124283478
- GandhiNAPirozziGGrahamNMHCommonality of the IL-4/IL-13 pathway in atopic diseasesExpert Rev Clin Immunol201713542543728277826
- VatrellaAFabozziICalabreseCDupilumab: a novel treatment for asthmaJ Asthma Allergy2014712313025214796
- WenzelSFordLPearlmanDDupilumab in persistent asthma with elevated eosinophil levelsN Engl J Med2013368262455246623688323
- WenzelSCastroMCorrenJDupilumab efficacy and safety in adults with uncontrolled persistent asthma despite use of medium-to-high-dose inhaled corticosteroids plus a long-acting β2 agonist: a randomised double-blind placebo-controlled pivotal phase 2b dose-ranging trialLancet201638810039314427130691
- MaselliDJKeytHRogersLProfile of lebrikizumab and its potential in the treatment of asthmaJ Asthma Allergy20158879226309415
- CorrenJLemanskeRFHananiaNALebrikizumab treatment in adults with asthmaN Engl J Med2011365121088109821812663
- HananiaNANoonanMCorrenJLebrikizumab in moderate-to-severe asthma: pooled data from two randomised placebo-controlled studiesThorax201570874875626001563
- HananiaNAKorenblatPChapmanKREfficacy and safety of lebrikizumab in patients with uncontrolled asthma (LAVOLTA I and LAVOLTA II): replicate, phase 3, randomised, double-blind, placebo-controlled trialsLancet Respir Med201641078179627616196
- PiperEBrightlingCNivenRA phase II placebo-controlled study of tralokinumab in moderate-to-severe asthmaEur Respir J201341233033822743678
- BrightlingCEChanezPLeighREfficacy and safety of tralokinumab in patients with severe uncontrolled asthma: a randomised, double-blind, placebo-controlled, phase 2b trialLancet Respir Med20153969270126231288
- ArimaMFukudaTProstaglandin D2 and T(H)2 inflammation in the pathogenesis of bronchial asthmaKorean J Intern Med201126181821437156
- ChevalierE1StockJFisherTCutting edge: chemoattractant receptor-homologous molecule expressed on Th2 cells plays a restricting role on IL-5 production and eosinophil recruitmentJ Immunol200517542056206016081770
- ErpenbeckVJVetsEGheyleLPharmacokinetics, safety, and tolerability of fevipiprant (QAW039), a novel CRTh2 receptor antagonist: results from 2 randomized, phase 1, placebo-controlled studies in healthy volunteersClin Pharmacol Drug Dev20165430631327310331
- ErpenbeckVJPopovTAMillerDThe oral CRTh2 antagonist QAW039 (fevipiprant): a phase II study in uncontrolled allergic asthmaPulm Pharmacol Ther201639546327354118
- GonemSBerairRSingapuriAFevipiprant, a prostaglandin D2 receptor 2 antagonist, in patients with persistent eosinophilic asthma: a single-centre, randomised, double-blind, parallel-group, placebo-controlled trialLancet Respir Med20164969970727503237
- Available from: https://www.accessdata.fda.gov/cdrh_docs/pdf8/P080032b.pdfAccessed May 30, 2017
- CoxGThomsonNCRubinASAIR Trial Study GroupAsthma control during the year after bronchial thermoplastyN Engl J Med2007356131327133717392302
- PavordIDCoxGThomsonNCRISA Trial Study GroupSafety and efficacy of bronchial thermoplasty in symptomatic, severe asthmaAm J Respir Crit Care Med2007176121185119117901415
- CastroMRubinASLavioletteMAIR2 Trial Study GroupEffectiveness and safety of bronchial thermoplasty in the treatment of severe asthma: a multicenter, randomized, double-blind, sham-controlled clinical trialAm J Respir Crit Care Med2010181211612419815809
- TrivediAPavordIDCastroMBronchial thermoplasty and biological therapy as targeted treatments for severe uncontrolled asthmaLancet Respir Med20164758559227230825
- MenzellaFZucchiLPiroRA budget impact analysis of bronchial thermoplasty for severe asthma in clinical practiceAdv Ther201431775176125009004
- ZeinJGMenegayMCSingerMECost effectiveness of bronchial thermoplasty in patients with severe uncontrolled asthmaJ Asthma201653219420026377375
- PretolaniMDombretMCThabutGReduction of airway smooth muscle mass by bronchial thermoplasty in patients with severe asthmaAm J Respir Crit Care Med2014190121452145425496106
- DennerDRDoeingDCHogarthDKDuganKNaureckasETWhiteSRAirway inflammation after bronchial thermoplasty for severe asthmaAnn Am Thorac Soc20151291302130926230374
- RyanDMFowlerSJNivenRMReduction in peripheral blood eosinophil counts after bronchial thermoplastyJ Allergy Clin Immunol2016138130831026953157
- DebrayMPDombretMCPretolaniMEarly computed tomography modifications following bronchial thermoplasty in patients with severe asthmaEur Respir J2017493160156528298402
- Arcispedale Santa Maria Nuova-IRCCSBronchial thermoplasty: effect on neuronal and chemosensitive component of the bronchial mucosa (BT-ASMN)2014 Available from: https://clinicaltrials.gov/ct2/show/NCT01839591Accessed April 30, 2017 NLM Identifier: NCT01839591Accessed April 30, 2017
- DoeingDCMahajanAKWhiteSRSafety and feasibility of bronchial thermoplasty in asthma patients with very severe fixed airflow obstruction: a case seriesJ Asthma201350221521823252954
- FajtMLWenzelSEDevelopment of new therapies for severe asthmaAllergy Asthma Immunol Res20179131427826957
- WenzelSEAsthma phenotypes: the evolution from clinical to molecular approachesNat Med201218571672522561835
- LommatzschSEMartinRJGoodJTJrImportance of fiberoptic bronchoscopy in identifying asthma phenotypes to direct personalized therapyCurr Opin Pulm Med2013191424823197289
- DavilaIValeroAEntrenasLMRelationship between serum total IgE and disease severity in patients with allergic asthma in SpainJ Investig Allergol Clin Immunol2015252120127
- BousquetJRabeKHumbertMPredicting and evaluating response to omalizumab in patients with severe allergic asthmaRespir Med200710171483149217339107
- WagenerAHde NijsSBLutterRExternal validation of blood eosinophils, FE(NO) and serum periostin as surrogates for sputum eosinophils in asthmaThorax201570211512025422384
- GlaxoSmithKlineOmalizumab to mepolizumab switch study in severe eosinophilic asthma patients2016 Available from: https://clinicaltrials.gov/ct2/show/NCT02654145. NLM Identifier: NCT02654145Accessed may 30, 2017 NLM Identifier: NCT02654145
- NachefZKrishnanAMashtareTZhuangTMadorMJOmalizumab versus Mepolizumab as add-on therapy in asthma patients not well controlled on at least an inhaled corticosteroid: a network meta-analysisJ Asthma2017112
- MagnanABourdinAPrazmaCMTreatment response with mepolizumab in severe eosinophilic asthma patients with previous omalizumab treatmentAllergy20167191335134427087007
- GlaxoSmithKlineCross-sectional study for identification and description of severe asthma patients2014 Available from: https://clinical-trials.gov/ct2/show/NCT02293265. NLM Identifier: NCT02293265Accessed May 30, 2017
- ParulekarADAtikMAHananiaNAPeriostin, a novel biomarker of TH2-driven asthmaCurr Opin Pulm Med2014201606524247042
- WesterhofGAKorevaarDAAmelinkMBiomarkers to identify sputum eosinophilia in different adult asthma phenotypesEur Respir J201546368869626113672
- IzuharaKOhtaSOnoJUsing periostin as a biomarker in the treatment of asthmaAllergy Asthma Immunol Res20168649149827582399
- BelEHSousaAFlemingLUnbiased biomarkers for the prediction of respiratory disease outcome (U-BIOPRED) consortium, consensus generation. Diagnosis and definition of severe refractory asthma: an international consensus statement from the innovative medicine initiative (IMI)Thorax2011661091091721106547
- ChungKFWenzelSEBrozeketJLInternational ERS/ATS guidelines on definition, evaluation and treatment of severe asthmaEur Respir J201443234337324337046
- A budget impact analysis of bronchial thermoplasty for severe asthma in clinical practiceAdv Ther201431775176125009004
- MenzellaFLusuardiMMontanariGGaleoneCFacciolongoNZucchiLClinical usefulness of mepolizumab in severe eosinophilic asthmaTher Clin Risk Manag20161290791627354806
- Registry of the Ministry of Health nr. 75/2017 January 19 2017, Nucala. (n. 332/2017). (17A01570) (GU nr.49 / 28-02-2017).
- WuACPaltielADKuntzKMWeissSTFuhlbriggeALCost-effectiveness of omalizumab in adults with severe asthma:Results from the asthma policy modelJ Allergy Clin Immunol200712051146115217904628
- MahajanAKHogarthDKPayer coverage for bronchial thermoplasty: shifting the traditional paradigm for refractory asthma therapyChest201314431051105424008956
