Abstract
Progressive loss of lung function and reversibility characterize chronic asthma. The conventional therapy is targeted to control the disease without targeting the loss of lung function or reversibility. In a prospective real-world observation of long-term use of add-on doxycycline as a matrix-metalloproteinase inhibitor, we documented significant improvement in lung function with possible reversal of remodeling.
Background
Chronic asthma shows progressive decline in lung function with reduction or even loss of reversibility secondary to remodeling. A set of endopeptidase enzymes known as matrix metalloproteinases are intimately related to the pathogenesis of asthma and remodeling. The inhibition of matrix metalloproteinases is recognized as a prospective way of treating asthma and its corresponding structural remodeling.
Methods
In a randomized, prospective, real-world study, we have observed the change in lung function (spirometry) with an add-on of long-term doxycycline to standard asthma therapy as per the Global Initiative for Asthma guidelines in a small asthmatic population. The change in terms of forced expiratory volume (FEV1), forced vital capacity (FVC), percent of FEV1 (FEV1%), and forced expiratory flow (FEF25–75) were noted following variable duration of doxycycline therapy.
Results
There has been a global improvement in all the parameters in all the six patients suggesting improvement in obstruction, and reduction in air trapping following a treatment of add-on doxycycline for a mean duration of 162.83 ± 83.07 days. Of the changes seen, the post bronchodilator FEV1, the FVC, and the FEF25–75 showed significant improvements with the P-value set at 0.004, 0.054, and 0.031, respectively. There was also evidence of the reversal of remodeling from the improvement in the FEV1/FVC ratio. Moreover there was a greater than expected improvement of pre-bronchodilator FEV1 after treatment that far surpassed the initial post-bronchodialator FEV1 value. Even after such a change, there were presences of some reversibility suggesting room for further improvement.
Conclusion
The results suggest significant improvements in the obstructive parameters used to evaluate asthma, with possible reversal of remodeling evident in chronic asthmatics when treated with doxycycline in addition to standard therapies. This observation needs further scientific validation.
Introduction
Asthma is a disease of airway inflammation and airway hyper-responsivenessCitation1 with progressive narrowing of the airways due to both reversible and irreversible functional and structural changes; the apparently irreversible changes in chronic asthma have been denoted as remodeling given that they result in reduction in lung function and vary in terms of the degree of reversibility.Citation2 Assessment of airways by high-resolution computerized tomography (CT) of the chest can have a good correlation to the pathological measures of remodeling.Citation3 Of late, the forced expiratory volume (FEV1) forced vital capacity (FVC) ratio (FEV1/FVC) has also been detected as a surrogate marker of remodeling that correlates well with the airway changes assessed by CT scan.Citation4 The pathophysiology of asthma inflammation and airway remodeling has been marked by different microstructural changes including abnormal extracellular matrix turnover and fibrosisCitation5,Citation6 through the participation of an enzyme system called matrix metalloproteinase (MMPs) and its tissue inhibitor.Citation7–Citation9 Since modulation of the process by inhibition of MMPs may be beneficial to the asthmatics, we used doxycycline on a long-term basis in an open, prospective, real-world observation. We conducted this pilot work to see the effect of this antibiotic for its additional property of matrix metalloproteinase inhibitionCitation10–Citation12 and suppression of immunoglobulin-E (IgE)Citation13 alongside the use of standard asthma medications.
Methods
Inclusion of patients
We selected chronic asthmatics from the outpatient department of the institute who had long standing history of asthma symptoms with documented airflow limitation and significant reversibility (200 mL and 12%) using spirometry in compliance with the American Thoracic Society guideline.Citation14 The subjects were incorporated in a real-world observation protocol (approved by the Institutional Ethics Committee) upon signing the written informed consent form to undergo treatment with doxycycline on a long-term basis. Patients younger than 13 years and older than 75 years of age, those unwilling to undergo the study, and those having previous history of doxycycline intolerance or history of exacerbation within the preceding 6 weeks were excluded. Since it was a real world observation, we kept the study in tandem with the practicing style of the physician and the logistics of the real world. All the patients were informed of the need to (a) have repeated spirometry examinations; (b) attend regular follow-up visits; and (c) report the side effects (experienced or suspected), if any, apart from the need to continue doxycycline as an add-on therapy on top of optimal asthma treatments as per the Global Initiative for Asthma guidelines.Citation15 All the patients were on inhaled long-acting beta agonists plus inhaled corticosteroids with inhaled reliever short-acting β2 agonist prior to randomization so as to stabilize symptoms for at least 6 weeks. Patients were informed about the possible side effects of doxycycline and were instructed to consume the medicine at least 1 hour after eating. The offered dose of doxycycline was 100 mg twice daily and 100 mg once daily for patients with body weight over 40 kg or less than 40 kg, respectively. Ranitidine was co-prescribed universally to lessen the chance of gastrointestinal intolerance. The baseline spirometry data were preserved and the follow up spirometry data were incorporated for statistical analysis as soon as they were available. We looked for changes in both the pre- (initial) and post-bronchodilator values of spirometric variables across the FEV1, FVC, ratio of FEV1/FVC, and FEF25–75 for documentation of improvement, and changes in the FEV1/FVC for marking the improvement of remodeling according to the observations outlined by Chae et al.Citation4
Statistical calculations were done on these spirometric variables using two-tailed paired t-tests, and significance was noted with a P-value <0.05.
Results
Of the 24 patients being prescribed add-on doxycycline, a total of six patients (three males and three females, mean age of 47.0 ± 14.6 years) were included for data analysis. Their follow-ups were noted during the period from March 15, 2011 to November 03, 2011. Each patient showed an improvement in their asthma symptoms and exhibited reversibility, according to spirometry results. From the rest of the 18 patients, 10 did not perform repeat spirometry before or during the period of data collection. A total of four patients consumed the medicine inconsistently, two had stopped the therapy after a few days, and one had started the drug only recently. In another patient, the drug was stopped for subsequent diagnosis of tuberculosis.
The mean duration of add-on doxycycline between the baseline and posttreatment spirometric assessment was noted as 162.83 ± 83.07 days and the changes in the spirometric variables are displayed in . There was a global improvement across all the parameters; however, the change in the post-bronchodilator FEV1 was the most significant (P = 0.004). The other significant changes noted were post-bronchodilator FVC (P = 0.054), and both pre-and post-bronchodilator FEF25–75 (P = 0.023 and P = 0.031, respectively).
Table 1 Changes in spirometric variables in response to treatment of add-on doxycycline
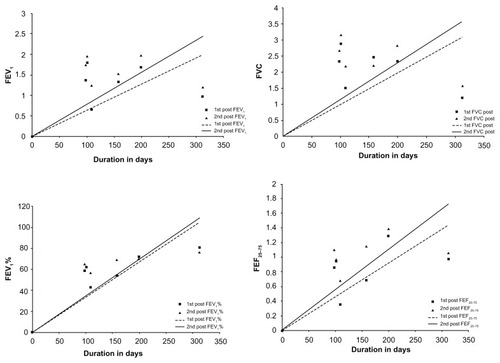
When the pre- (baseline) and posttreatment values were plotted on a duration scale, all the variables showed progressive improvement with time. However, the post-bronchodilator values exhibited more significant improvements compared to the pre-bronchodilator values for FEV1, FVC, percentage of forced exhaled volume (FEV1%), and FEF25–75 (displayed in ). No adverse effects of doxycycline were reported by the patients.
Figure 1 Changes in FEV1, FVC, FEV1%, and FEF25–75 as a function of initial and after use of add-on doxycycline treatment. (A–D) denote the changes in different parameters (FEV1, FVC, FEV1%, FEF25–75, respectively), expressed as a function of time in both their initial (dotted line) and after use of add-on doxycycline treatment (continuous line) values.
Discussion
Asthma is a global problem with a huge health care burden,Citation16 and remodeling of asthma is a universal phenomenon. The loss of lung function has been found to be accelerated in asthma despite therapy.Citation17,Citation18 So far, the treatment of asthma consists essentially of inhaled bronchodilators and inhaled corticosteroids with oral bronchodilators and anti-inflammatory agents used in certain situations as per the recommendation of treatment guidelines.Citation15 Asthma therapy has been targeted to achieve symptom ‘control’ and there has been no option available to treat the accelerated loss of lung function from remodeling.Citation15 Clinically, remodeling implies a progressive loss of lung function and reversibility, while pathologically it signifies an array of micro-structural changes that include the deposition and degradation of the extracellular matrix and fibrosis.Citation2 Abnormal deposition of the extracellular matrix has been observed in the submucosal and adventitial areas in both the large and small airways.Citation5,Citation6,Citation19,Citation20
Matrix metalloproteinases, a class of Zn-endopeptidase, and their tissue inhibitors (TIMPs) play a very significant role in the process. Several MMPS are found up-regulated in asthma; of these, MMP-9 has been found in higher quantities in the sputum, bronchoalveolar lavage fluid, and serum of asthmatics,Citation7–Citation9 and is also found to be elevated in several different situations such as asthma exacerbation,Citation21 occupational asthma,Citation22 and nocturnal asthma.Citation23 Similarly, the tissue inhibitor of matrix metalloproteinase-1 (TIMP-1) has been found to be elevated in asthmatics.Citation7 The MMP/ TIMP balance is regarded as important in the development of allergy-induced asthma since it is reduced by the pulmonary administration of TIMP-1 or TIMP-2.Citation24 In animal models, different MMP inhibitors are found to reduce airway inflammationCitation24 and bronchial hyperreactivity.Citation25
Both early and late reactions in asthma have been found to be reduced in sheep models when MMP inhibitors are used, and thus MMP inhibition may be a prospective therapeutic target in asthmatics.Citation26,Citation27 We have tried to exploit this concept in a few cases of chronic asthma with the long-term use of a known MMP inhibitor, doxycycline.Citation10,Citation11,Citation12 Such use of doxycycline has been approved by the United States Food and Drug Administration for the treatment of periodontal disease,Citation28 and the long-term use of doxycycline has been documented in several other indications with few toxicities noted.Citation29–Citation32
Incidentally, doxycycline is also able to suppress IgE, and this property can also be exploited for the treatment of asthma.Citation13 Daoud et al have documented the use of minocycline among people with asthma, and they examined the effects of this drug across a number of spirometric parameters of lung function as related to IgE suppression.Citation33,Citation34 Doxycycline was found to successfully reduce the airway inflammation and hyper-responsiveness in murine model of Toluene di-isocyanate induced asthma.Citation35 Thus, we conclude that doxycycline, by virtue of its MMP inhibitory and IgE suppressive properties, can be a useful adjunct in the management of asthma.
In our observations, we noted significant improvements across measures of obstruction (FEV1), and also across the surrogate marker of remodeling FEV1/FVC.Citation3 The changes in FEF25–75 and FEV1 suggest that the observed changes took place both in medium and small-sized airways. Given that the improvement exceeded the expected post-bronchodilator value and yet maintaining some reversibility, it suggests some structural changes that may have resulted from the use of the intervention to the benefit of the patients. Such supranormal improvement in the posttreatment spirometry with demonstration of existence of some reversibility suggests the scope of further improvement. Our results clearly exceeded our expectations, and this implies that the so-called remodeling is not necessarily a fixed structural change.
Our observation may be the first of its kind to show a change in the natural history of asthma by pharmacotherapy. Subsequent research should try to address how long this therapy can be continued and how far the natural history of asthma can be changed. It is not possible to speak about the side effects of doxycycline in this observation given that our sample size included a small number of patients. In addition, the chances of gastrointestinal toxicities and the reflux related to the administration of this drug were, perhaps, lessened by the universal use of ranitidine. A good prospective, randomized, double blind study with a much larger sample population might be able to address these questions.
Despite several weaknesses in the current study (ie, small sample size, real-world observation, no control group, no histological proof, and no high-resolution CT assessment of remodeling), our observations warrant attention and further validation.
Disclosure
The authors report no conflicts of interest in this work.
References
- Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease (COPD) and asthmaThis official statement of the American Thoracic Society was adopted by the ATS Board of Directors, November 1986Am Rev Respir Dis19871362252443605835
- EliasJAZhuZChuppGHomerRJAirway remodeling in asthmaJ Clin Invest199910481001100610525034
- AysolaRSHoffmanEAGieradaDAirway remodeling measured by multidetector CT is increased in severe asthma and correlates with pathologyChest200813461183119118641116
- ChaeEJKimTBChoYSAirway measurement for airway remodeling defined by post-bronchodilator FEV1/FVC in asthma: investigation using inspiration-expiration computed tomographyAllergy Asthma Immunol Res20113211111721461250
- MauadTXavierACSaldivaPHDolhnikoffMElastosis and fragmentation of fibers of the elastic system in fatal asthmaAm J Respir Crit Care Med1999160396897510471626
- ParameswaranKWillems-WidyastutiAAlagappanVKRadfordKKranenburgARSharmaHSRole of extracellular matrix and its regulators in human airway smooth muscle biologyCell Biochem Biophys2006449113914616456242
- CataldoDMunautCNoelAMMP-2- and MMP-9-linked gelatinolytic activity in the sputum from patients with asthma and chronic obstructive pulmonary diseaseInt Arch Allergy Immunol2000123325926711112863
- MautinoGHenriquetCGougatCIncreased expression of tissue inhibitor of metalloproteinase-1 and loss of correlation with matrix metalloproteinase-9 by macrophages in asthmaLab Invest199979139479952109
- VignolaAMRiccobonoLMirabellaASputum metalloproteinase-9/ tissue inhibitor of metalloproteinase-1 ratio correlates with airflow obstruction in asthma and chronic bronchitisAm J Respir Crit Care Med19981586194519509847290
- PiresPWRogersCTMcClainJLGarverHSFinkGDDorranceAMDoxycycline, a matrix metalloprotease inhibitor, reduces vascular remodeling and damage after cerebral ischemia in stroke-prone spontaneously hypertensive ratsAm J Physiol Heart Circ Physiol20113011H87H9721551278
- RenSGuoLLYangJDoxycycline attenuates acrolein-induced mucin production, in part by inhibiting MMP-9Eur J Pharmacol2011650141842321036164
- KaitoKUrayamaHWatanabeGDoxycycline treatment in a model of early abdominal aortic aneurysmSurg Today200333642644312768368
- Smith-NorowitzTABluthMHDrewHEffect of minocycline and doxycycline on IgE responsesAnn Allergy Asthma Immunol200289217217912197574
- PellegrinoRViegiGBrusascoVCrapoROInterpretive strategies for lung function testsEur Respir J200526594896816264058
- http://www.ginasthma.org [homepage on the Internet]Pocket guide for asthma management and preventionGlobal Initiative for Asthma (GINA) updated 2011. Available from: http://www.ginasthma.org/guidelines-pocket-guide-for-asthma-management.htmlAccessed 18 June, 2012
- MasoliMFabianDHoltSBeasleyRfor Global Initiative for Asthma (GINA) ProgramThe global burden of asthma: executive summary of the GINA Dissemination Committee reportAllergy200459546947815080825
- PeatJKWoolcockAJCullenKRate of decline of lung function in subjects with asthmaEur J Respir Dis19877031711793569449
- LangePParnerJVestboJSchnohrPJensenGA 15-year follow-up study of ventilatory function in adults with asthmaN Engl J Med199833917119412009780339
- ChakirJShannonJMoletSAirway remodeling associated mediators in moderate to severe asthma: effect of steroids on TGF-beta, IL-11, IL-17, and type I and type III collagen expressionJ Allergy Clin Immunol200311161293129812789232
- de Medeiros MatsushitaMda SilvaLFdos SantosMAAirway proteoglycans are differentially altered in fatal asthmaJ Pathol2005207110211016041692
- LeeYCLeeHBRheeYKSongCHThe involvement of matrix metalloproteinase- 9 in airway inflammation of patients with acute asthmaClin Exp Allergy200131101623163011678864
- PalikheNSKimJHParkHSBiomarkers predicting isocyanateinduced asthmaAllergy Asthma Immunol Res201131212621217921
- PhamDNChuHWMartinRJKraftMIncreased matrix metalloproteinase-9 with elastolysis in nocturnal asthmaAnn Allergy Asthma Immunol2003901727812546341
- KumagaiKOhnoIOkadaSInhibition of matrix metalloproteinases prevents allergen-induced airway inflammation in a murine model of asthmaJ Immunol199916274212421910201949
- BruceCThomasPSThe effect of marimastat, a metalloprotease inhibitor, on allergen-induced asthmatic hyper-reactivityToxicol Appl Pharmacol2005205212613215893540
- MukhopadhyaySSypekJTavendaleRMatrix metalloproteinase- 12 is a therapeutic target for asthma in children and young adultsJ Allergy Clin Immunol20101261707620546881
- LiWLiJWuYIdentification of an orally efficacious matrix metalloprotease 12 inhibitor for potential treatment of asthmaJ Med Chem200952175408541919725580
- GolubLMLeeHMRyanMEGiannobileWVPayneJSorsaTTetracyclines inhibit connective tissue breakdown by multiple non-antimicrobial mechanismsAdv Dent Res199812212269972117
- BhattacharyyaPNagSAcharyya GhoshDChowdhurySRBardhanSMukherjeeATreatment of probable idiopathic pulmonary fibrosis with long term doxycycline, a matrix metalloproteinase inhibitorIndian Journal of Chest Disease and Allied Sciences2007493180
- BhattacharyyaPNagSBardhanSThe role of long-term doxycycline in patients of idiopathic pulmonaryfibrosis: The results of an open prospective trialLung India2009263818520442842
- NewtonPNChauletJFBrockmanAPharmacokinetics of oral doxycycline during combination treatment of severe falciparum malariaAntimicrob Agents Chemother20054941622162515793155
- http://www.hpa.org.uk [homepage on the Internet]MalariaLondonHealth Protection Agency2012 Available from: http://www.hpa.org.uk/infections/topics_az/malaria/Accessed 18 June, 2012
- DaoudAGloriaCJTaningcoGMinocycline treatment results in reduced oral steroid requirements in adult asthmaAllergy Asthma Proc200829328629418534087
- JoksRSmith-NorowitzTNowakowskiMBluthMHDurkinHGTetracycline-mediated IgE isotype-specific suppression of ongoing human and murine IgE responses in vivo and murine memory IgE responses induced in vitroInt Immunol201022428128820181654
- LeeKSJinSMKimSSLeeYCDoxycycline reduces airway inflammation and hyperresponsiveness in a murine model of toluene diisocyanate-induced asthmaJ Allergy Clin Immunol2004113590290915131573