Abstract
Background
Despite the availability of new pharmacological options and novel combinations of existing drug therapies, the rate of suboptimal asthma control is still high. Therefore, early identification of the clinical and behavioral factors responsible for poor asthma control, and interventions during routine outpatient visits to improve asthma trigger management, are strongly recommended. This study was designed to evaluate the profiles of asthmatic patients and their inhaler treatment devices in relation to asthma control in Turkey.
Methods
A total of 572 patients with persistent asthma (mean [standard deviation] age: 42.7 [12.1] years; 76% female) were included in this prospective observational study. A baseline visit (0 month, visit 1) and three follow-up visits (1, 3 and 6 months after enrolment) were conducted to collect data on demographics, past medical and asthma history, and inhaler device use.
Results
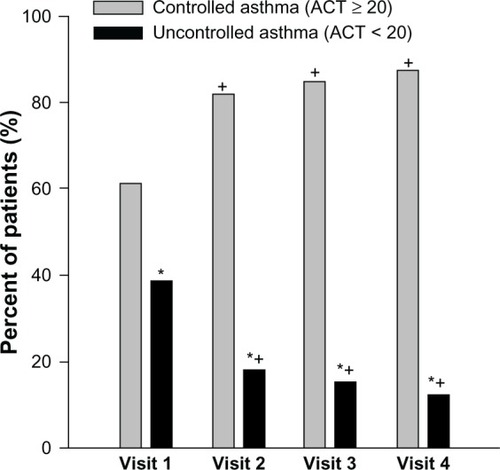
Asthma control was identified in 61.5% of patients at visit 1 and increased to 87.3% at visit 4 (P < 0.001), regardless of sociodemographics, asthma duration, body mass index or smoking status. The presence of asthma-related comorbidity had a significantly negative effect on asthma control (P = 0.004). A significant decrease was determined, in the rate of uncontrolled asthma, upon follow-up among patients who were using a variety of fixed dose combination inhalers (P < 0.001 for each). Logistic regression analysis was used to show that the presence of asthma-related comorbidity (odds ratio [OR], 0.602; 95% confidence interval [CI], 0.419; 0.863, P = 0.006) and active smoking (OR, 0.522; 95% CI, 0.330; 0.825, P = 0.005) were significant predictors of asthma control.
Conclusion
Our findings indicate that, despite ongoing treatment, asthma control rate was 61.5% at visit 1 in adult outpatients with persistent asthma. However, by the final follow-up 6 months later, this had increased to 87.3%, independent of sociodemographic and clinical characteristics. Poor asthma control was associated with asthma-related comorbid diseases, while the efficacy of fixed dose combinations was evident in the achievement of asthma control.
Introduction
As a common chronic disease that substantially burdens both patients’ lives and health economics,Citation1,Citation2 asthma has 300 million sufferers worldwide, with an additional 100 million people estimated to be affected by 2025.Citation3 The number of patients diagnosed with asthma in Turkey was estimated at 3–4 million,Citation4 while the prevalence proportion was reported at 7.4% by the Global Initiative for Asthma (GINA) – Global Burden of Asthma Report.Citation5
Although the results of clinical trials suggest that asthma control can be reached in most patients,Citation6 the epidemiologic evidence suggests a low level of disease control in many countries including Turkey,Citation7–Citation9 despite the availability of international and national asthma guidelines, and effective medications that would enable optimum control of the disease.Citation5,Citation10
Therefore, the challenge to find the best way to assess asthma control and define management strategies to ensure that this control is achieved and maintained, still remains.Citation11 The update of the GINA 2006 guidelines recommends a newly introduced asthma management approach, based on the monitoring of disease control, to facilitate the acceptance and use of asthma guidelines in clinical practice.Citation5 This approach is based on the use of combined therapies in which inhaled corticosteroids (ICS) are given, mainly in combination with long-acting beta-2-adrenoceptor agonists (LABA).Citation12–Citation14 However, despite this availability of new pharmacological options and novel combinations of existing drug therapies, suboptimal asthma control rates are persistently high. Citation15
In order to tackle this, early identification of the clinical and behavioral factors responsible for poor asthma control,Citation16 and interventions during routine outpatient visits for improving asthma trigger management,Citation17 have been recommended. In addition, follow-up consultations including checking the patients’ adherence to their medication plan, and measures to reduce the exposure to risk factors have also been strongly recommended.Citation18
Clinicians and general practitioners must be aware of the levels and determinants of asthma control in order to reflect and improve on the implementation of the asthma guidelines.Citation5,Citation19 Therefore this real-life prospective ASIT (Asthma Inhaler Treatment) study, conducted at 31 secondary and tertiary centers across Turkey, was designed to evaluate the profiles of persistent-asthma patients and their inhaler treatment devices in relation to asthma control, through a series of follow-ups.
Material and Methods
Study population
A total of 572 patients with persistent asthma were included in this multi-center, non-interventional, single arm prospective observational study, conducted at 31 pneumology outpatient clinics across Turkey. The study was based on four consecutive visits, the first performed at the study enrolment (month 0, visit 1), and then follow-ups at 1,3, and 6 months. Female or male outpatients older than 18 years and diagnosed with persistent asthma according to the GINA criteriaCitation12 at least 6 months previously, and who had received at least one dose of ICS + LABA either in separate or fixed combinations irrespective of pharmacological agent(s), were included. The exclusion criteria were: confirmed or suspected pregnancy; breastfeeding; comorbid COPD; allergy/sensitivity or intolerance to any kind of asthma treatment; anti-immunoglobulin E treatment within the last 4 months; treatment with leukotriene receptor antagonists; hospitalization due to symptomatic respiratory infection of asthma within the last 8 weeks; chronic diseases that were likely to negatively affect the prognosis (eg, carcinoma); chronic alcohol consumption; and substance abuse.
Following detailed explanation of the objectives and protocol of the study, written informed consent was obtained from each subject. The study was conducted in accordance with the ethical principles stated in the “Declaration of Helsinki” and approved by the Kocaeli University Research Ethics Committee.
Data collection
After certifying the patients’ eligibility against the inclusion/exclusion criteria, data on sociodemographic characteristics (age, gender, educational status, and occupation), vital signs, physical examination findings, medical history, comorbid disorders, concomitant treatments, characteristics and clinical course of asthma disease, asthma control, and asthma treatment via inhaler device were collected at the initial enrollment visit. At each follow up visit, patients were evaluated for vital signs, physical examination findings, concomitant treatments, characteristics and clinical course of asthma disease, asthma control, and asthma treatment via inhaler device.
The Asthma Control Test (ACT), a standard test developed for reflecting the patient’s perspective of his/her disease,Citation20 helps determine asthma control levels, predict exacerbations, and optimize therapy for the patients.Citation21,Citation22 The ACT™ has been translated into Turkish and cultural adaptation has been completed.Citation23
In the present study, the ACT™ filled in by patients was used to assess their level of asthma control in the 4 weeks preceding the enrollment, considering an overall score of 20 or higher as controlled asthma, and a score less than 20 as uncontrolled asthma.
Statistical analysis
Sample size was calculated to include at least 1050 patients to be able to observe 40% of the difference between two different treatment alternatives or inhaler devices and standard error of 2%, confidence level of >95%, and statistical power of 90%. However, only 572 patients were enrolled in the study.
Stata Data Analysis and Statistical Software (Version 10, StataCorp LP, College Station, TX, USA) was used for statistical analysis. Data were expressed as “mean (standard deviation [SD])”, percent (%) and 95% confidence interval where appropriate. Significance levels during the categorical comparison of the groups were evaluated by the Chi-square test using cross table statistics. The Kruskal–Wallis and Mann–Whitney U tests were used for independent groups without normal distribution, while Student’s t-test was used for comparison of two independent groups. The ANOVA test and post-hoc Tukey’s HSD test were used for more than two independent groups with normal distribution. Logistic regression analysis was performed with asthma control (categorical) as the dependent variable while “Enter” was selected as the method and “simple first” as the categorical variable coding scheme. Predictors with possible influence on dependent variable were added as covariates. All tests were two-sided and P < 0.05 was considered statistically significant.
Results
Baseline demographic, clinical and asthma-related characteristics
The mean (SD) age of the 572 patients in the ASIT study was 42.7 (12.1) years and 76% (n = 435) were females. The majority of the patients (n = 440; 76.9%) were secondary school graduates and 61.9% were unemployed (55.8% housewives) (). Mean (SD) time from asthma onset was 8.0 (8.3) years while less than or equal to 5 years in 53.3% of the patients (). Active smokers represented 18.2% (n = 104) of the patients ().
Table 1 Sociodemographic characteristics of patients according to asthma control at baseline
Among the 530 patients with comorbidities, 56.1% (n = 321) had asthma-related disorders, and a single asthma-related comorbidity was noted in 67.9% of the patients ().
The evaluation of vital signs showed mean (SD) systolic blood pressure (BP) as 121.1 (15.6) mmHg, diastolic BP as 75.6 (8.9) mmHg, pulse as 81.2 (8.9)/min, and respiratory rate as 16.8 (3.2)/min. Mean (SD) body mass index (BMI) was 28.0 (5.4) (kg/m2).
Baseline characteristics associated with asthma control status
Overall, asthma was determined to be controlled in 61.5% (n = 352) of the patients, with no statistical difference in control level with respect to mean age, gender, asthma duration, educational, or employment status. The uncontrolled asthma group had a significantly higher number of active smokers (23.2%) versus 15.1% in the controlled asthma group (P = 0.015) ().
The presence of asthma-related comorbidities had significantly negative effects on asthma control (). Half (51.4%) of the patients with controlled asthma had asthma-related comorbidities, while this percentage rose to 63.6% (140/220) in the uncontrolled asthma group (P = 0.004). The most common asthma-related comorbidity was rhinitis, and this was significantly more frequent among uncontrolled asthma group (P = 0.009).
Asthma control status throughout the study visits
Overall, the ratio of patients with controlled asthma was significantly higher (61.5% at visit 1, 82.0% at visit 2, 84.8% at visit 3 and 87.3% at visit 4; P < 0.001 for each) than that of uncontrolled asthma at each study visit and there was a significant progressive decrease in the ratio of uncontrolled patients at the follow-up visits compared to baseline (P < 0.001 for each) from 38.5% to 12.7% at the end of the study ().
Asthma control status from visit 1 to visit 4: asthma duration, BMI, smoking status and comorbid disorders
When asthma control status from visit 1 to visit 4 was evaluated in terms of time from asthma onset (0–15 versus more than 15 years), BMI (30 kg/m2 or higher versus less than 30 kg/m2), and smoking status (smoker versus non-smoker), a significant decrease in the ratio of patients with uncontrolled asthma was found in each case, regardless of the grouping (). Significantly higher rates of asthma control at visit 4 compared to visit 1 were detected even in patients with time from asthma onset more than 15 years (). On the other hand, the asthma control rate was significantly higher at all visits, both among nonsmokers compared to active smokers (64% versus 51%, P = 0.010 and 89% versus 78%; P = 0.030, respectively); and among patients with BMI lower than 30 kg/m2 compared to those with BMI 30 kg/m2 or higher at visit 4 (88.5% versus 81.8%, P = 0.009) ().
Table 2 Change in asthma control status from Visit 1–Visit 4 in terms of asthma duration, BMI, smoking status, and comorbid disorders
Patients with one (P < 0.001), two (P = 0.004) and three (P = 0.021) comorbidities had significantly higher ACT scores at visit 4 compared to visit 1, while baseline ACT scores of patients with three comorbidities were significantly lower than baseline scores of patients with a single comorbidity (P = 0.007) ().
Asthma control status from visit 1 to visit 4: inhaler treatment
Significant improvement in asthma control status during follow-up was observed in patients using fixed dose ICS/LABA combination inhalers (). There was a significant decrease in the ratio of patients with uncontrolled asthma from visit 1 to visit 4 for patients who received: ‘fluticasone propionate/salmeterol discus’ (38.2% versus 11.4%, P < 0.001); ‘extra fine beclomethasone/formoterol solution spray’ (32.7% versus 10.0%, P < 0.001); and ‘budesonide/formoterol turbuhaler’ (41.7% to 14.9%, P < 0.001). There were no significant changes in the ratio of uncontrolled asthma observed in patients receiving ‘budesonide and formoterol aerolizer’ (42.9% to 23.5%, P = 0.131) (). Overall, the ratio of patients with uncontrolled asthma was decreased by 45.2%–70.2%, depending on the inhaler type ().
Figure 2 Change in percentage of uncontrolled asthma patients (n = 220) with fixed dose and seperate combination inhaler treatments from visit 1 to visit 4.
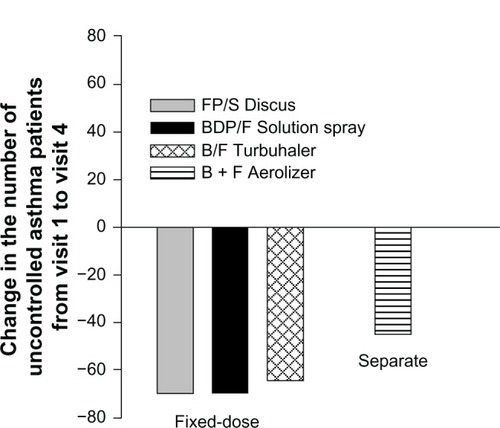
Table 3 Asthma control level according to inhaler device as assessed by the physicians
Logistic regression analysis for predictors of asthma control
Using asthma control (categorical) as the dependent variable, logistic regression analysis showed that the presence of asthma-related comorbidity (odds ratio [OR], 0.602; 95% CI, 0.419;0.863, P = 0.006) and active smoking (OR, 0.522; 95% CI, 0.330; 0.825, P = 0.005) were significant predictors of asthma control ().
Table 4 Logistic regression analysis for predictors of asthma control
Discussion
The principal findings of this real-life prospective ASIT study showed that the asthma control rate increased during follow up in adult outpatients with persistent asthma, moving from 61.5% to 87.0% after 6 months, regardless of patient demographics, smoking, educational, or employment status. Notably, the incidence of comorbid diseases was associated with poor asthma control, while fixed dose combinations proved highly effective in asthma control.
Failure in asthma control has been reported in several studies, despite variations in selected populations and methodology,Citation19 while objectives for good control proposed by international reference guidelines are still far from being met.Citation7,Citation24–Citation26 National and international asthma management guidelines recommend continuous, preventive rather than symptom-driven and crisis-oriented care.Citation27,Citation28 In this regard, justifying emphasis on asthma control versus asthma severity in the guidelines, our finding of asthma control (ACT score of ≥20) in 87.3% of patients promisingly highlights the role of patient monitoring via close follow up in the achievement of better asthma control.
The Asthma Insights and Reality in Europe (AIRE) Study, a multinational, population-based telephone survey, showed that 94.7% of all patients fail to achieve proper control of their disease.Citation24 The ASES Study, an office-based study conducted in Spain, confirmed that the percentage of patients at primary care and pneumologist office visits who reported suffering symptoms more than once a week was 24% and 32%, respectively.Citation29 In a population-based screening conducted in eleven European countries within the scope of European Respiratory Health Survey (ERCHS) II, overall asthma control rate was reported to be 32%, while the proportion of uncontrolled asthma in ICS users greatly varied by country, ranging from 20% (Iceland) to 67% (Italy).Citation19 Recently, a survey conducted in five European countries indicated that 50.4% of asthmatics had low levels of control;Citation30 this percentage increased to 56.6% in a more recent survey conducted in the same countries.Citation31
A cross-sectional study of 1188 patients with asthma from 28 centers in Turkey indicated controlled asthma in 51.5% of the patients (ACT ≥ 20),Citation9 while the Asthma Insights and Reality in Turkey (AIRET) study,Citation8 consistent with other international AIR surveys, demonstrated achievement of guideline-based asthma control in only 1.3% of participants, despite the availability of effective therapies.
The inconsistency of data on asthma control has been associated with the varied implementations of the asthma treatment guidelines in different countries, different treatment regimens, and geographic variation in asthma severity.Citation19 Moreover, comparison of data from different studies is difficult due to different asthma control measures and data collection methods adopted. For example, the higher proportion of controlled patients in our study compared to the ECRHS II surveyCitation19 may be linked to the fact that in the latter, asthma control was evaluated with the GINA guidelines composite measure, including lung function, whereas the former used ACT, which excludes lung function; therefore a higher rate of asthma control is to be expected.Citation15
The combined effects of failure to comply with recommendations and poor patient adherence to treatment, along with low usage of preventive medicine and low expectations of treatment, can be considered as the leading causes of poor disease control.Citation32 Given the positive influence of close patient monitoring on asthma control rates in our study, we consider better implementation of asthma management guidelines and patient education to raise awareness and expectations as crucial to improving asthma outcomes in Turkey.Citation8
The majority (79.5%) of patients with persistent asthma in our study were receiving fixed combination therapy. SABA was used in 32.5%, ICS in 20.3%, and LABA in 13.6% of patients, while spray (31.5%), turbuhaler (29.9%) and discus (26.6%) were the most frequently used inhaler types, with a high level (>94%) of overall satisfaction from inhaler therapy. Likewise, data from a past study concerning determinants of asthma control at tertiary healthcare level in Turkey indicated use of ICS and LABA combination in 57% of the 900 patients surveyed.Citation9
The use of fixed combination therapy in the majority of our patients is consistent with the remarkable alteration in practice patterns of asthma management in the last decade. There has been an increase in the prescription rate of controller medications, including multiple controllers for ICS + LABA, after Asthma Insights and Reality (AIR) surveys in the US, Europe, Asia-Pacific, Japan and Latin America populations reported low levels of asthma control.Citation24,Citation33–Citation36
Our findings found asthma control to be negatively associated with the incidence of comorbidities such as rhinitis, sinusitis and GERD, while it was positively associated with the use of fixed dose combination treatments. Significantly higher rates of asthma control were achieved by visit 4 compared to visit 1, even in patients with ≥15 years of asthma duration, and irrespective of age, gender, asthma duration, smoking status or BMI. However the presence of asthma-related comorbidity and active smoking were found to be significant predictors of worse asthma control.
ICS/LABA fixed combinations are reportedly the most commonly used anti-asthmatic medicationsCitation15 and the most effective treatment choice.Citation15,Citation32 Our findings confirmed this, with 61.5% of patients using fixed dose combination treatment achieving asthma control.
Indeed, the use of fixed dose combination therapy (ICS/LABA) was among the factors associated with optimal control of asthma in a study from France,Citation37 along with normal BMI, non-smoker status, age <50 and good compliance. On the other hand, exacerbation, use of reliever medication, switch of therapy and smoking have been listed as the factors for poor control in a Swiss study.Citation38 In another study from France, lack of asthma control in 41.1% of 4362 patients with persistent asthma was associated with patient-related factors including smoking, poor compliance and critical errors in device manipulation.Citation39
Our study is also in line with the international population-based ECRHS II Survey conducted in 11 countries,Citation19 which reported no differences based on gender or age in categories of asthma control.
Asthma-related comorbidities were identified in 56.1% of patients overall in our study population, with rhinitis in 38.3%, GERD in 18.5% and sinusitis in 18.4%. This is in accordance with the most common comorbidities reported in asthma, including rhinitis, sinusitis, GERD, obstructive sleep apnea, hormonal disorders and psychiatric disorders.Citation40 Our findings that higher scores of ACT and higher likelihood of asthma control were linked with a lesser number of comorbidities, support the evidence that various comorbid conditions such as rhino-sinusitis, GERD, psychological disturbances, and respiratory infections, are often observed in asthmatic patientsCitation40 and will place greater burden on healthcare systems unless taken into consideration in asthma treatment.Citation41
In accordance with the dataCitation31 that indicate smoking is a critical factor in the risk of poor asthma controlCitation42,Citation43 and impaired corticosteroid response,Citation44 there was a significantly lower percentage of smokers classified under the controlled asthma category at visit 1 (51.0% versus 64.0% non-smokers, P = 0.010) and visit 4 (78.0% versus 89% non-smokers, P = 0.030) in our study population.
Our study’s greatest value is in being the first large-scale, detailed survey conducted across Turkey using a patient evaluation questionnaire. The limitations are the lack of data on asthma severity and also the high drop-out rate (46.0%) from visit 1 to visit 4.
Conclusion
In conclusion, our findings in this real-life prospective ASIT study revealed an asthma control rate of 61.5% in adult outpatients with persistent asthma in Turkey, which increased upon each follow-up, regardless of the smoking, educational and employment status of the patients. Fixed dose combinations proved superior in the achievement of asthma control. However, poor asthma control was associated with the incidence of comorbid diseases. Our findings have provided valuable data on the positive role of regular monitoring in disease control. We therefore advocate regular patient monitoring and patient education to raise awareness and therapeutic expectations, in order to better implement asthma management guidelines and achieve better control of the disease.
Acknowledgments
This study is funded by Chiesi İlac Tic. A.S. Turkiye. We would like to thank KAPPA Consultancy Training Research Ltd, Istanbul, for providing editorial support; Monitor CRO, Istanbul, for providing support in statistical analysis; and Aysegul Kahraman from Chiesi Tic. A.S. Turkiye for her great efforts and contributions at all stages of the study publication. The author wrote this paper on behalf of the ASIT Study Group. The other members, (by the physician’s name in descending order of number of patients enrolled) are:
Yıldız F, Study Coordinator (Department of Pulmonary Diseases, Kocaeli University School of Medicine, Kocaeli)
Erbagci A (Zonguldak Uzun Mehmet Chest Diseases Hospital, Zonguldak)
Demirel YS (Department of Chest Diseases, Ankara University, School of Medicine, Ankara)
Akcalı SD (Chest Diseases Clinic, Ankara Dıskapı Yıldırım Beyazıt Hospital, Ankara)
Ekici A (Department of Chest Diseases, Kirikkale University, School of Medicine, Kirikkale)
Dursunoglu N (Department of Chest Diseases,Pamukkale University School of Medicine,Denizli)
Ediger D (Department of Chest Diseases, Uludag University, School of Medicine, Bursa)
Erdinc M (Department of Chest Diseases, Ege University, School of Medicine, Izmir)
Cemri SC (Chest Diseases Clinic, Mersin State Hospital, Mersin)
Kalyoncu AF (Department of Chest Diseases, Hacettepe University, School of Medicine, Ankara)
Guclu SZ (Dr. Suat Seren Chest Diseases Hospital, Izmir)
Aktogu S (Dr. Suat Seren Chest Diseases Hospital, Izmir)
Bayramgurler B (Chest Diseases Clinic, Derince Research and Training Hospital, Kocaeli)
Bayram M (Chest Diseases Clinic, Sivas Numune Research and Training Hospital, Sivas)
Akgun M (Department of Chest Diseases, Erzurum Atatürk University, School of Medicine, Erzurum)
Mirici A (Department of Chest Diseases, Canakkale 18 March University, School of Medicine, Canakkale)
Akyildiz L (Chest Diseases Clinic, Private Park Hospital, Mardin)
Celik P (Department of Chest Diseases, Celal Bayar University, School of Medicine, Manisa)
Guven AO (Nihat Kitapci Chest Diseases Hospital, Erzurum)
Camsari G (Yedikule Chest Diseases Hospital, Istanbul)
Ozseker F (Sureyyapasa Chest Diseases Hospital, Istanbul)
Cimen F (Atatürk Chest Diseases Hospital, Ankara)
Kurutepe M (Sureyyapasa Chest Diseases Hospital, Istanbul)
Senyigit A (Department of Chest Diseases, Dicle University, School of Medicine, Diyarbakir)
Bektas Y (Trabzon Chest Diseases Hospital, Trabzon)
Ozbudak O (Department of Chest Diseases, Akdeniz University, School of Medicine, Antalya)
Saylan B, Baslilar S (Chest Diseases Clinic, Umraniye Research and Training Hospital, Istanbul)
Polatli M (Department of Chest Diseases, Adnan Menderes University, School of Medicine, Aydin)
Cagatay T (Department of Chest Diseases, Istanbul University, Istanbul School of Medicine, Istanbul)
Kalkan S (Chest Diseases Clinic, Private Batman Hospital, Batman)
Ozer A (Chest Disease Clinic, Cukurova State Hospital, Adana).
Disclosure
The author declares no conflict of interests in this paper.
References
- European Community Respiratory Health SurveyVariations in the prevalence of respiratory symptoms, self-reported asthma attacks, and use of asthma medication in the European community respiratory health survey (ECRHS)Eur Respir J199696876968726932
- Van GanseEAntonicelliLZhangQAsthma-related resource use and cost by GINA classification of severity in three European countriesRespir Med200610014014716338597
- MasoliMFabianDHoltSBeasleyRThe global burden of asthma: executive summary of the GINA Dissemination Committee reportAllergy20045946947815080825
- Turkish Ministry of Health Chronic Airway Diseases (COPD-Asthma) Prevention and Control Program (2009–2013) Action PlanAnkara20093941
- global initiative for asthma (GINA)Global strategy for asthma management and prevention. NHLBI/WHO workshop report1995 updated 2007
- BatemanEDBousheyHABousquetJCan guideline-defined asthma control be achieved? The Gaining Optimal Asthma Control studyAm J Respir Crit Care Med200417083684415256389
- RabeKFAdachiMLaiCKWorldwide severity and control of asthma in children and adults: the global asthma insights and reality surveysJ Allergy Clin Immunol2004114404715241342
- SekerelBEGemiciogluBSorianoJBAsthma insights and reality in Turkey (AIRET) studyRespir Med20061001850185416564685
- TurktasHMunganDUysalMAOguzulgenKTurkish Asthma Control Survey Study GroupDeterminants of asthma control in tertiary level in Turkey: a cross-sectional multicenter surveyJ Asthma20104755756220560829
- Expert Panel Report 2 Guidelines for the diagnosis and management of asthma. Publication No 97–4051BethesdaNational Heart, Lung and Blood Institutes of Health1997
- LundbackBDahlRAssessment of asthma control and its impact on optimal treatment strategyAllergy20076261161917508964
- GINA (Global Initiative on Asthma), National Institutes of Health, National Heart Lung and Blood Institute, NHLBI/WHO Workshop ReportGlobal strategy for asthma management and prevention11995 updated 2008
- National Asthma Education and Prevention ProgramExpert Panel Report 3 (EPR-3): guidelines for the Diagnosis and Management of Asthma-Summary Report 2007J Allergy Clin Immunol200712094138 J Allergy Clin Immunol20081211330
- OhtaKYamaguchiMAkiyamaKJapanese guideline for adult asthmaAllergol Int20116011514521636963
- AllegraLCremonesiGGirbinoGPRISMA (PRospectIve Study on asthMA control) Study GroupReal-life prospective study on asthma control in Italy: cross-sectional phase resultsRespir Med201210620521422035853
- HorneRPriceDClelandJCan asthma control be improved by understanding the patient’s perspective?BMC Pulm Med20077817518999
- RankMWollanPLiJYawnBTrigger recognition and management in poorly controlled asthmaticsAllergy Asthma Proc2010319910520977834
- Global initiative for asthma (GINA)Global strategy for asthma management and prevention Updated 2011. Available from: http://www.ginasthma.org/uploads/users/files/GINA_Report2011_May4.pdfAccessed November 14, 2012
- CazzolettiLMarconAJansonCTherapy and Health Economics Group of the European Community Respiratory Health SurveyAsthma control in Europe: a real-world evaluation based on an international population-based studyJ Allergy Clin Immunol20071201360136717981317
- NathanRASorknessCAKosinskiMDevelopment of the asthma control test: a survey for assessing asthma controlJ Allergy Clin Immunol2004113596514713908
- SchatzMSorknessCALiJTAsthma Control Test: reliability, validity, and responsiveness in patients not previously followed by asthma specialistsJ Allergy Clin Immunol200611754955616522452
- KoFWHuiDSLeungTFEvaluation of the asthma control test: a reliable determinant of disease stability and a predictor of future exacerbationsRespirology20121737037822107482
- MAPI Research Institute: Linguistic validation [Webpage on the internet]LyonMAPI Research Institute2004http://www.mapiresearch.fr/i02intr.htmAccessed February 11, 2010
- RabeKFVermeirePASorianoJBMaierWCClinical management of asthma in 1999: the Asthma Insights and Reality in Europe (AIRE) studyEur Respir J20001680280711153575
- VermeirePARabeKFSorianoJBMaierWCAsthma control and differences in management practices across seven European countriesRespir Med20029614214911905548
- SorianoJBRabeKFVermeirePAPredictors of poor asthma control in European adultsJ Asthma20034080381314626337
- ChapmanKRImpact of ‘mild’ asthma on health outcomes: findings of a systematic search of the literatureRespir Med2005991350136216210094
- HaselkornTFishJEZeigerRSTENOR Study GroupConsistently very poorly controlled asthma, as defined by the impairment domain of the Expert Panel Report 3 guidelines, increases risk for future severe asthma exacerbations in The Epidemiology and Natural History of Asthma: Outcomes and Treatment Regimens (TENOR) studyJ Allergy Clin Immunol200912489590219811812
- Lopez-VinaACimasJEDiaz SanchezCCoriaGVegazoOPicado VallesCA comparison of primary care physicians and pneumologists in the management of asthma in Spain: ASES studyRespir Med20039787288112924513
- DemolyPPaggiaroPPlazaVPrevalence of asthma control among adults in France, Germany, Italy, Spain and the UKEur Respir Rev20091810511220956130
- DemolyPGueronBAnnunziataKAdamekLWaltersRDUpdate on asthma control in five European countries: results of a 2008 surveyEur Respir Rev20101915015720956184
- FueyoARuizMAAncocheaJGuileraMBadiaXESCASE GroupAsthma control in Spain. Do season and treatment pattern matter? The ESCASE studyRespir Med200710191992417079125
- LaiCKDe GuiaTSKimYYAsthma Insights and Reality in Asia-Pacific Steering Committee. Asthma control in the Asia-Pacific region: the asthma insights and reality in Asia-Pacific studyJ Allergy Clin Immunol200311126326812589343
- AdamsRJFuhlbriggeAGuilbertTLazanoPMartinezFInadequate use of asthma medication in the United States: results of Asthma in America national population surveyJ Allergy Clin Immunol2002110586412110821
- AdachiMMorikawaAIshiharaKAsthma insights and reality in Japan (AIRJ)Arerugi20025141142012087759
- NeffenHFritscherCSchachtFCAIRLA Survey GroupThe Asthma insights and reality in Latin America surveyRev Panam Salud Publica20051719119715826399
- GodardPHuasDSohierBPribilCBoucotIAsthma control in general practice: a cross-sectional survey of 16,580 patientsPresse Med20053413511357 French [with English abstract]16292185
- MiedingerDNeukommEChhajedPNThe use of the Asthma Control Test in general practice and its correlation with asthma control according to the GINA guidelinesCurr Med Res Opin2011272301230821988667
- MolimardMLe GrosVImpact of patient-related factors on asthma controlJ Asthma20084510911318350401
- BouletLPBoulayMÈAsthma-related comorbiditiesExpert Rev Respir Med2011537739321702660
- GershonASWangCGuanJToTBurden of comorbidity in individuals with asthmaThorax20106561261820627918
- McLeishACZvolenskyMJAsthma and cigarette smoking: a review of the empirical literatureJ Asthma20104734536120528586
- HaughneyJPriceDKaplanAAchieving asthma control in practice: understanding the reasons for poor controlRespir Med20081021681169318815019
- ThomsonNCChaudhuriRAsthma in smokers: challenges and opportunitiesCurr Opin Pulm Med200915394519077704