Abstract
Purpose
To study risk factors for uncontrolled asthma and insufficient quality of life (QoL) in patients with mild asthma, ie those without preventer treatment.
Patients and Methods
Patients aged 18–75 years with a doctor’s diagnosis of asthma randomly selected from primary and secondary care in Sweden. Mild asthma was defined as self-reported current asthma and no preventer treatment. Data were collected from self-completed questionnaires in 2012 and 2015. Well-controlled asthma was defined as Asthma Control Test (ACT) ≥20 points and no exacerbation and uncontrolled asthma as ACT<20 points and/or at least one exacerbation in the previous six months. QoL was measured by the Mini Asthma Quality of Life Questionnaire (Mini-AQLQ), where a total mean score of ≥ 6 indicated sufficient and < 6 insufficient QoL. Multivariate logistic regression analyses were performed using asthma control and Mini-AQLQ as dependent variables. Asthma control was dichotomized as controlled and uncontrolled asthma and the Mini-AQLQ as sufficient QoL (mean score ≥6) and insufficient QoL (mean score <6).
Results
Among 298 patients, 26% had uncontrolled asthma, 40% insufficient QoL and 20% both uncontrolled asthma and insufficient QoL. Age ≥60 years, obesity, daily smoking, rhinitis and inadequate knowledge of asthma self-management were independently associated with poor asthma control. Factors independently associated with insufficient QoL were age ≥60 years, overweight, obesity, rhinitis, sinusitis and inadequate knowledge of asthma self-management. Age ≥60 years, obesity, rhinitis and inadequate knowledge of asthma self-management were independently associated with both uncontrolled asthma and insufficient QoL.
Conclusion
Among asthma patients without preventer medication, 26% had uncontrolled asthma and 40% had insufficient asthma-related QoL. Older age, obesity, and rhinitis were risk factors for both poor asthma control and a reduced QoL, but having good knowledge of asthma self-management reduced this risk. Our findings suggest that this group of patients requires further attention and follow-up.
Plain Language Summary
Many patients with little symptoms of asthma do not take asthma-preventer medication as their asthma is recognized as mild. Still, it is well-known that in this group there are patients with frequent and severe symptoms and acute attacks of asthma, defined as uncontrolled asthma. Quality of life (QoL) is less studied in these patients. Our aim was to study patient characteristics and factors with a higher risk for uncontrolled asthma and insufficient QoL in patients with mild asthma.
We studied patients with asthma diagnosis 18–75 of age in Sweden who reported asthma and no asthma preventer medication. They answered questionnaires about characteristics, knowledge of asthma, asthma symptoms, acute asthma attacks and QoL. A test for asthma symptom control, the Asthma Control Test (ACT), was answered, where 20 points or more meant good asthma symptom control. Patients were regarded as having uncontrolled asthma if they had less than 20 points and/or at least one acute asthma attack the last six months. QoL was measured by the Mini Asthma Quality of Life Questionnaire. A mean score of 6 or more meant sufficient and less than 6 insufficient QoL.
Of the 298 patients, 26% had uncontrolled asthma, 40% had insufficient QoL and 20% had both. Patients with risk for both uncontrolled asthma and insufficient QoL were 60 years and over, with obesity, rhinitis and those who reported insufficient knowledge of how to handle asthma. Our results suggest that patients with mild asthma need more attention, better management and follow-ups.
Introduction
Asthma is a common chronic respiratory disease affecting approximately 300 million individuals worldwide.Citation1 The asthma prevalence in adults in Sweden is estimated to be about 10%.Citation2 Depending on the definition and population, between 50% and 75% of asthma patients are believed to have mild asthma.Citation3 The International Global Initiative for Asthma (GINA) guidelines define mild asthma as asthma that is well controlled at pharmacological treatment step 1 or step 2.Citation1,Citation4 However, mild asthma can be defined in several ways, for example by symptom control and lung function, or by current therapy regardless of asthma control.Citation4 The term mild asthma is disputed as it may imply that patients with infrequent and mild symptoms are at low risk of deterioration of asthma.Citation1 There is an ongoing discussion on how to define mild asthma.Citation5
The overall goal of asthma treatment and management is to accomplish asthma control, including symptom control and reducing the risk of future adverse outcomes such as acute exacerbations.Citation1 However, it is well known that a sizable portion of patients with asthma have uncontrolled asthma.Citation6–8 Patients who appear to have mild asthma are also often suffering from a lack of asthma control. A cross-sectional study of patients with mild asthma from eight countries found that 25% of the patients had uncontrolled asthma.Citation9 According to a systematic review, the average number of exacerbations per patient per year was 2.9 in patients with mild asthma, and up to 42% of individuals had unscheduled physician visits related to asthma.Citation4 Several studies have shown that patients who are only treated with short-acting beta2-agonist (SABA) as needed, have a significant risk of having uncontrolled asthma.Citation9–12 The use of only as needed SABA is associated with an elevated risk of exacerbations compared to the use of inhaled corticosteroid-formoterol (ICS-formoterol) as needed.Citation13 An excessive use of SABA is linked to increased risks of exacerbations and mortality.Citation14
It is essential to assess patients´ experiences and perceptions of how asthma affects their quality of life (QoL). Although more objective clinical parameters are important, measuring health-related quality of life (HRQL) should also be included when evaluating the disease, as it measures a person’s own perception of how the disease affects daily life ie activities, emotions and functions.Citation15,Citation16 Studies have shown that severe and/or uncontrolled asthma is associated with poor HRQL.Citation17–19 Patients with mild asthma may also have impaired HRQL, and asthma control seems to impact HRQL, even when severity measures are taken into account.Citation17,Citation18 This emphasizes the need to identify patients at risk of both poor asthma control and impaired HRQL.
The main objective of this study was to identify risk factors for both uncontrolled asthma and insufficient QoL in Swedish primary and secondary care patients with mild asthma, ie without preventer treatment.
Materials and Methods
Study Design, Setting and Participants
The PRAXIS study, an observational study involving adult asthma patients randomly selected from primary and secondary care in central Sweden, provided the data. The first cohort started in 2005 with a follow-up in 2012 and a second cohort started in 2015.
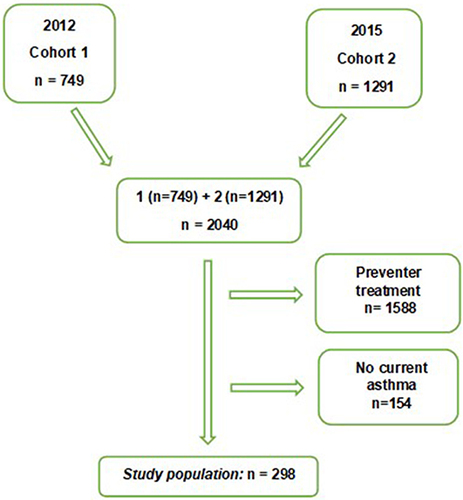
In 2005, a questionnaire was sent to the first cohort of 1725 patients with a doctor’s diagnosis of asthma (ICD-10 J45), aged 18–75 years. The response rate in 2005 was 71%, and 61% of those responded to the follow-up in 2012, resulting in 749 participating patients. In 2015 members of the second cohort of 2804 asthma patients were randomly selected from the same centers, and after approving participation were sent the same extended questionnaire as in 2012. With a 46% response rate, 1291 patients were included. The present study includes 2040 patients from two cross-sectional studies, the follow-up in 2012, and the second cohort in 2015.
In this study, mild asthma was defined as having a doctor’s diagnosis of asthma, self-reported current asthma and no preventer treatment (inhaled corticosteroid or montelukast). There were 298 study participants, 78% from primary care and 22% from secondary care, (see flow chart ).
Variables
The self-completion questionnaire provided information on patient characteristics and symptoms including night awakenings due to asthma, use of short-acting beta2-agonists, educational level, comorbidities, self-assessed severity of disease, and exacerbations. The Swedish versions of the Asthma Control Test (ACT) and Mini-Asthma Quality of Life Questionnaire (Mini-AQLQ) were included in the questionnaire.
Age was categorized into three groups < 40, 40–59, ≥60 years, body mass index (BMI) kg/m2 into underweight/normal weight (< 24.9), overweight (25–29.9), obesity (≥ 30) and smoking as daily or no smoking. Educational level was divided into high educational level defined as at least three years beyond the Swedish compulsory schooling of 9 years and low educational level below.
Self-reported comorbid diagnoses present during the last 12 months included allergic rhino-conjunctivitis due to pet and/or pollen allergy, rhinitis, anxiety and/or depression and sleep apnoea. Additionally, sinusitis reported over the previous six months and gastroesophageal reflux disease (GERD) defined as night symptoms of heartburn and/or acid reflux at least once a week were included as comorbidities. Self-assessed severity of asthma was categorized into very mild, mild, moderate and severe and knowledge of asthma self-management as adequate (yes, yes partly) and inadequate (yes little, no) knowledge.
Outcome Measures – Asthma Control and Quality of Life
Asthma symptom control was assessed using the ACT and exacerbation history. The ACT comprises five questions about asthma symptom control in the previous four weeks with a score ranging from 5 to 25 points. A score ≥20 points indicates well-controlled, and <20 points indicates poor asthma symptom control.Citation20
An asthma exacerbation was defined as an emergency visit to a hospital or primary care due to asthma worsening and/or a course of oral corticosteroids due to asthma worsening in the previous six months.
In this study, well-controlled asthma was defined as ACT ≥20 points and no exacerbation in the previous six months; and uncontrolled asthma ACT < 20 and/or at least one exacerbation during the last six months.
The disease-specific quality of life instrument, the Mini-AQLQ, was used to assess QoL.Citation21 The mini-AQLQ includes 15 questions about symptoms (5 items), activity limitations (4 items), emotional function (3 items) and environmental stimuli (3 items) during the previous two weeks. Each item is assessed on a seven-point scale, from severe (1) to no (7) impairment. A total mean score was calculated, where a mean score below six indicates an impact on the HRQL.Citation22
Statistical Analysis
The statistical analyses were performed using SPSS Statistics version 26.0. Cross-tabulation and Chi-2 tests assessed differences in proportions, and differences between groups for continuous data were assessed using the Student’s t-test. Multivariate logistic regression analyses were performed using asthma control and Mini-AQLQ as dependent variables. Asthma control was dichotomized as controlled and uncontrolled asthma and the Mini-AQLQ as sufficient QoL (mean score ≥6) and insufficient QoL (mean score <6). Independent variables that were statistically significantly associated with uncontrolled asthma and insufficient QoL in the univariate analyses, were included in the multivariate analyses. A p-value of <0.05 was considered to be statistically significant.
Ethics
This study is part of the PRAXIS-study, which was approved by the Regional Ethical Review Board of Uppsala (Dnr 2011/318). The participants were informed about the purpose of the study, in accordance with the Declaration of Helsinki. Written consent was obtained from all participants.
Results
Patient Characteristics
Of the study population with a doctor’s diagnosis of asthma (n=2040), 298 (16%) study participants had current asthma and no preventer treatment. The mean age was 49 (SD ±15.9) years, 58% were women, the mean BMI was 27 kg/m2 (SD ±5.21), 5% were daily smokers, 76% had pet-and/or pollen allergy, 66% had rhinitis and 45% had high-level education, see stratified by sex. Some 44% of study participants assessed their asthma as very mild, 38% mild, 16% moderate and 2% severe. In total, 52% reported sufficient knowledge of asthma self-management, and no statistically significant differences between the sexes were found (p=0.057).
Table 1 Patient Characteristics Stratified by Sex
Factors Associated with Asthma Control and Quality of Life
Ten percent of the study participants had experienced at least one exacerbation, 6% received treatment with a course of oral steroids due to exacerbation in the previous six months and 19% had an ACT score <20. Some 19% reported night awakenings due to asthma symptoms during the previous week and 17% had taken extra doses of SABA more than twice.
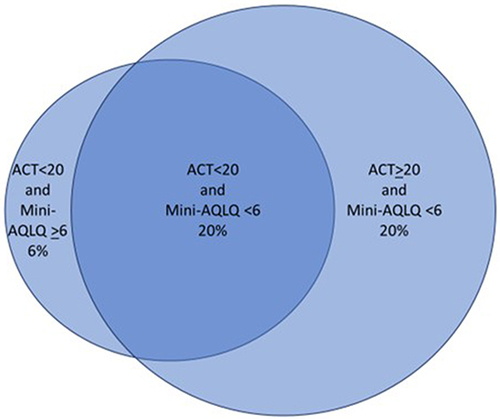
In total, 26% had uncontrolled asthma, 40% had a Mini-AQLQ total mean score <6 and 20% had both uncontrolled asthma and insufficient QoL (). shows patient characteristics stratified into asthma control/uncontrolled asthma and Mini-AQLQ ≥ 6 / Mini-AQLQ <6.
Table 2 Patient Characteristics Stratified by Level of Asthma Control and Quality of Life
Figure 2 Proportions of patients with either uncontrolled asthma/insufficient Mini-AQLQ (20%), controlled asthma/insufficient Mini-AQLQ (20%) or uncontrolled asthma/sufficient Mini-AQLQ (6%).
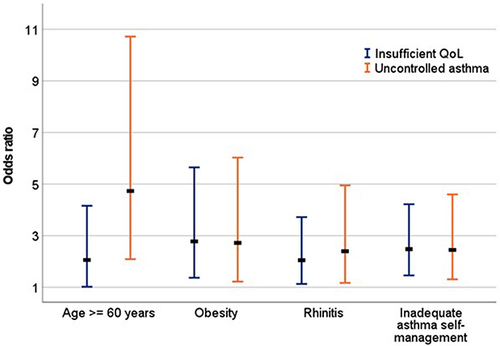
Age ≥60, obesity, daily smoking, rhinitis and inadequate knowledge of asthma self-management were independently associated with not achieving asthma control (). Factors independently associated with insufficient QoL were age ≥60, overweight, obesity, rhinitis, sinusitis and inadequate knowledge of asthma self-management ().
Table 3 Factors Associated with Uncontrolled Asthma
Table 4 Factors Associated with Insufficient Quality of Life
Factors associated with both uncontrolled asthma and insufficient QoL, were age ≥ 60 years OR 4.73 (95% CI 2.09–10.72) and OR 2.06 (95% CI 1.02–4.16); obesity OR 2.72 (95% CI 1.22–6.03) and OR 2.78 (95% CI 1.37–5.65); rhinitis OR 2.40 (95% CI 1.17–4.95) and OR 2.05 (95% CI 1.13–3.72) and inadequate knowledge of asthma self-management OR 2.45 (95% CI 1.31–4.60) and OR 2.48 (1.46–4.22) ().
Discussion
The main findings in this real-world study of Swedish asthma patients with no preventer medication were that 26% had uncontrolled asthma, 40% had insufficient asthma-related QoL and 20% had both uncontrolled asthma and insufficient QoL. Age ≥ 60 years, obesity and rhinitis were risk factors for both uncontrolled asthma and impaired quality of life; however, the risk was decreased by self-reported adequate knowledge of asthma self-management.
Our results are consistent with other studies where a significant portion of patients with asthma that appeared mild did not have asthma control, as determined by ACT measurements of asthma symptoms and exacerbation frequency.Citation9,Citation12,Citation23 In our study of patients without preventer medication, 10% of the patients reported at least one exacerbation during the previous six months and 6% had taken a course of oral steroids due to exacerbation. In a global prospective study with a three-year follow-up time, 23% of the patients with physician-assessed mild asthma had at least one exacerbation in the last 12 months, with 15% experiencing severe exacerbations.Citation23 Additionally, in a survey of patients who described their asthma as mild, more than 50% reported at least one exacerbation during the previous year.Citation24
In our study, 19% of the participants had nocturnal awakenings, and 17% had used rescue medication more than twice in the previous week. In a real-world survey of mild asthma patients from eight nations, 41% of the respondents reported having symptoms at night and 34% had used a rescue inhaler in the previous four weeks.Citation9 However, in this study, mild asthma was defined by treatment with SABA as needed or low-dose ICS which may be a sign of more severe disease than in our study. Frequent use of rescue medication, older age and comorbidity have all been demonstrated to be risk factors for worsening asthma severity in patients with mild asthma.Citation25
Previous research has demonstrated that asthma control is a strong predictor of HRQL even if differences in severity are taken into account.Citation19 A longitudinal real-world study in adult asthmatics showed that asthma control and BMI were key predictors of asthma-related QoL.Citation26 In our study 79% of those with uncontrolled asthma had insufficient asthma-related QoL (data not shown). Our findings that older age, obesity, daily smoking and rhinitis are associated with poorer asthma control have previously been noted in individuals with asthma.Citation27–30 However, to the best of our knowledge, these associations have not previously been found in patients with mild asthma without preventer treatment. Factors associated with insufficient asthma-related QoL in mild asthma have been less studied. Louis et al showed that being female, higher BMI and smoking were associated with a lower asthma-related QoL in a group of asthma patients recruited from secondary care.Citation31 The association between higher BMI and lower QoL has also been demonstrated in other studies but not in mild asthma patients.Citation32,Citation33 In a Swedish multicentre study of individuals with asthma of different severity levels, rhinosinusitis, obesity and high age were associated with lower quality of life as in our study.Citation34 However, we have shown that in patients with mild asthma without preventer treatment, common comorbidities such as rhinitis and obesity, as well as older age are associated with both uncontrolled asthma and insufficient quality of life. This highlights the need to also identify and prioritize patients without preventer treatment with these risk factors so that they can have follow-ups and reviews to be better managed.
Another important finding was that self-reported adequate knowledge of asthma self-management was associated with a lower risk of uncontrolled asthma and insufficient QoL. The importance of self-management of asthma in achieving treatment goals is well known. It involves knowledge of how to handle the disease with non-pharmacological and pharmacological treatments through education about the disease, treatments, risk factors and skills training. The most effective way to disseminate this in clinical practice is to develop a good and continuous partnership with the patient and the health care providers.Citation1 According to a study by Mancuso et al good knowledge, a more positive attitude and more self-efficacy are all associated with higher QoL.Citation35 It is interesting to note that even though the patients in our study did not receive preventer treatment, the association was still statistically significant, stressing the value of education and self-management in this group.
Strengths and Limitations of the Study
Patients with asthma without preventer treatment are a prevalent group in clinical practice, but there are few studies that characterize them. Our results could therefore be regarded as relevant and important, because they provide information about disease control, quality of life and associated risk factors. As these patients were randomly selected from a large number of Swedish primary care centers and secondary care hospitals, the results can be generalized for Swedish asthma patients without preventer treatment.
A weakness of our study was that the study group was rather small. Only data from questionnaires were used and there were no data on lung function or from medical records that could have provided more information. The questionnaire did not include information about as needed treatment, but we can assume that a sizable portion of patients were treated with SABA as needed. There is very little possibility that the patients had treatment with ICS-formoterol as needed as our study was conducted before the release of the GINA guidelines in 2018.
Conclusion
In all, 26% of the patients who were not receiving preventer treatment had uncontrolled asthma, and 40% had poorer QoL related to their asthma. Older age, obesity, and rhinitis were risk factors for both poor asthma control and a reduced QoL, but having a good understanding of asthma self-management reduced the risk. The findings imply that a significant portion of asthma patients in this group may not be receiving sufficient care, and that there are opportunities for improvement in the treatment, information and education necessary to manage their asthma effectively.
Disclosure
Dr Sofia Eriksson reports non-financial support from Astra Zeneca, outside the submitted work. Dr Maaike Giezeman reports grants from ALF funding Region Örebro County; personal fees from Böhringer Ingelheim, Orion Pharma, and Astra Zeneca, outside the submitted work. Dr Hanna Sandelowsky reports personal fees from AstraZeneca, GSK, Chiesi, and OrionPharma, outside the submitted work. Dr Björn Ställberg reports personal fees from AstraZeneca, Novartis, Boehringer Ingelheim, and GlaxoSmithKleine, outside the submitted work. Dr Karin Lisspers reports personal fees from Novartis, Boehringer Ingelheim, AstraZeneca, and GlaxoSmithKline, outside the submitted work. The authors report no other conflicts of interest in this work.
Additional information
Funding
References
- Global Initiative for Asthma. Global strategy for asthma management and prevention; 2022. Available from: www.ginasthma.org/gina-reports/. Accessed June 26, 2024.
- Backman H, Raisanen P, Hedman L, et al. Increased prevalence of allergic asthma from 1996 to 2006 and further to 2016 - results from three population surveys. Clin Exp Allergy. 2017;47(11):1426–1435. doi:10.1111/cea.12963
- Dusser D, Montani D, Chanez P, et al. Mild asthma: an expert review on epidemiology, clinical characteristics and treatment recommendations. Allergy. 2007;62(6):591–604. doi:10.1111/j.1398-9995.2007.01394.x
- FitzGerald JM, Barnes PJ, Chipps BE, et al. The burden of exacerbations in mild asthma: a systematic review. ERJ Open Res. 2020;6(3):00359–2019. doi:10.1183/23120541.00359-2019
- Mohan A, Lugogo NL, Hanania NA, et al. Questions in mild asthma. An official American Thoracic Society Research Statement. Am J Respir Crit Care Med. 2023;207(11):e77–e96. doi:10.1164/rccm.202304-0642ST
- Cazzoletti L, Marcon A, Janson C, et al. Asthma control in Europe: a real-world evaluation based on an international population-based study. J Allergy Clin Immunol. 2007;120(6):1360–1367. doi:10.1016/j.jaci.2007.09.019
- Kämpe M, Lisspers K, Ställberg B, Sundh J, Montgomery S, Janson C. Determinants of uncontrolled asthma in a Swedish asthma population: cross-sectional observational study. Eur Clin Respir J. 2014;1(1):24109. doi:10.3402/ecrj.v1.24109
- Peters SP, Jones CA, Haselkorn T, Mink DR, Valacer DJ, Weiss ST. Real-world Evaluation of Asthma Control and Treatment (REACT): findings from a national Web-based survey. J Allergy Clin Immunol. 2007;119(6):1454–1461. doi:10.1016/j.jaci.2007.03.022
- Ding B, Small M. Disease burden of mild asthma: findings from a Cross-Sectional Real-World Survey. Adv Ther. 2017;34(5):1109–1127. doi:10.1007/s12325-017-0520-0
- Reddel HK, Ampon RD, Sawyer SM, Peters MJ. Risks associated with managing asthma without a preventer: urgent healthcare, poor asthma control and over-The-counter reliever use in a cross-sectional population survey. BMJ Open. 2017;7(9):e016688. doi:10.1136/bmjopen-2017-016688
- Price D, David-Wang A, Cho SH, et al. Time for a new language for asthma control: results from REALISE Asia. J Asthma Allergy. 2015;8:93–103. doi:10.2147/JAA.S82633
- Stridsman C, Axelsson M, Warm K, Backman H. Uncontrolled asthma occurs in all GINA treatment steps and is associated with worse physical health - a report from the OLIN adult asthma cohort. J Asthma. 2021;58(5):586–595. doi:10.1080/02770903.2020.1713150
- Reddel HK, Busse WW, Pedersen S, et al. Should recommendations about starting inhaled corticosteroid treatment for mild asthma be based on symptom frequency: a post-hoc efficacy analysis of the START study. Lancet. 2017;389(10065):157–166. doi:10.1016/S0140-6736(16)31399-X
- Nwaru BI, Ekström M, Hasvold P, Wiklund F, Telg G, Janson C. Overuse of short-acting β(2)-agonists in asthma is associated with increased risk of exacerbation and mortality: a nationwide cohort study of the global SABINA programme. Eur Respir J. 2020;55(4):1901872. doi:10.1183/13993003.01872-2019
- Wilson SR, Rand CS, Cabana MD, et al. Asthma outcomes: quality of life. J Allergy Clin Immunol. 2012;129(3 supp):S88–S123. doi:10.1016/j.jaci.2011.12.988
- Juniper EF, Wisniewski ME, Cox FM, Emmet AH, Nielsen KE, O’Byrne PM. Relationship between quality of life and clinical status in asthma: a factor analysis. Eur Respir J. 2004;23(2):287–291. doi:10.1183/09031936.04.00064204
- Chapman KR. Impact of ‘mild’ asthma on health outcomes: findings of a systematic search of the literature. Respir Med. 2005;99(11):1350–1362. doi:10.1016/j.rmed.2005.03.020
- Song HJ, Blake KV, Wilson DL, Winterstein AG, Park H. Health-related quality of life and health utilities of mild, moderate, and severe asthma: evidence from the Medical Expenditure Panel Survey. J Asthma Allergy. 2021;14:929–941. doi:10.2147/JAA.S316278
- Chen H, Gould MK, Blanc PD, et al. Asthma control, severity, and quality of life: quantifying the effect of uncontrolled disease. J Allergy Clin Immunol. 2007;120(2):396–402. doi:10.1016/j.jaci.2007.04.040
- Thomas M, Kay S, Pike J, et al. The Asthma Control Test (ACT) as a predictor of GINA guideline-defined asthma control: analysis of a multinational cross-sectional survey. Prim Care Respir J. 2009;18(1):41–49. doi:10.4104/pcrj.2009.00010
- Juniper EF, Guyatt GH, Cox FM, Ferrie PJ, King DR. Development and validation of the Mini Asthma Quality of Life Questionnaire. Eur Respir J. 1999;14(1):32–38. doi:10.1034/j.1399-3003.1999.14a08.x
- Bateman ED, Boushey HA, Bousquet J, et al. Can guideline-defined asthma control be achieved? The Gaining Optimal Asthma ControL study. Am J Respir Crit Care Med. 2004;170(8):836–844. doi:10.1164/rccm.200401-033OC
- Golam SM, Janson C, Beasley R, et al. The burden of mild asthma: clinical burden and healthcare resource utilisation in the NOVELTY study. Respir Med. 2022;200:106863. doi:10.1016/j.rmed.2022.106863
- Guarnieri G, Batani V, Senna G, Dama A, Vianello A, Caminati M. Is mild asthma truly mild? The patients’ real-life setting. Expert Rev Respir Med. 2022;16(11–12):1263–1272. doi:10.1080/17476348.2023.2167714
- Chen W, FitzGerald JM, Lynd LD, Sin DD, Sadatsafavi M. Long-term trajectories of mild asthma in adulthood and risk factors of progression. J Allergy Clin Immunol Pract. 2018;6(6):2024–32.e5. doi:10.1016/j.jaip.2018.04.027
- Louis G, Pétré B, Schleich F, et al. Predictors of change in asthma-related quality of life: a longitudinal real-life study in adult asthmatics. Qual Life Res. 2023;32(5):1507–1520. doi:10.1007/s11136-022-03339-0
- Racine G, Forget A, Moullec G, Jiao T, Blais L, Lemiere C. Predictors of asthma control and exacerbations: a real-world study. J Allergy Clin Immunol Pract. 2021;9(7):2802–2811. doi:10.1016/j.jaip.2021.04.049
- Camarinha C, Fernandes M, Alarcão V, Franco J. Determinants associated with uncontrolled asthma in Portugal: a national population-based study. Pulmonology. 2023;29(1):29–41. doi:10.1016/j.pulmoe.2020.02.014
- Zhong N, Lin J, Zheng J, et al. Uncontrolled asthma and its risk factors in adult Chinese asthma patients. Ther Adv Respir Dis. 2016;10(6):507–517. doi:10.1177/1753465816663978
- Phillips KM, Hoehle LP, Caradonna DS, Gray ST, Sedaghat AR. Association of severity of chronic rhinosinusitis with degree of comorbid asthma control. Ann Allergy Asthma Immunol. 2016;117(6):651–654. doi:10.1016/j.anai.2016.09.439
- Louis G, Pétré B, Schleich F, et al. Predictors of asthma-related quality of life in a large cohort of asthmatics: a cross-sectional study in a secondary care center. Clin Transl Allergy. 2021;11(7):e12054. doi:10.1002/clt2.12054
- Lavoie KL, Bacon SL, Labrecque M, Cartier A, Ditto B. Higher BMI is associated with worse asthma control and quality of life but not asthma severity. Respir Med. 2006;100(4):648–657. doi:10.1016/j.rmed.2005.08.001
- Grammer LC, Weiss KB, Pedicano JB, et al. Obesity and asthma morbidity in a community-based adult cohort in a large urban area: the Chicago Initiative to Raise Asthma Health Equity (CHIRAH). J Asthma. 2010;47(5):491–495. doi:10.3109/02770901003801980
- Ek A, Middelveld RJM, Bertilsson H, Bjerg A, Ekerljung L. Chronic rhinosinusitis in asthma is a negative predictor of quality of life: results from the Swedish GA2LEN survey. Allergy. 2013;68(10):1314–1321. doi:10.1111/all.12222
- Mancuso CA, Sayles W, Allegrante JP. Knowledge, attitude, and self-efficacy in asthma self-management and quality of life. J Asthma. 2010;47(8):883–888. doi:10.3109/02770903.2010.492540