Abstract
Chronic sphenoid rhinosinusitis is a spectrum of inflammatory diseases in isolated sphenoid sinus which may persist over a period of 12 weeks. It is a different entity from other types of rhinosinusitis because clinical presentations include headache, visual loss or diplopia, and patients may or may not have nasal obstruction or nasal discharge. Nasal endoscopic examination is useful, and computed tomography is mandatory. The disease requires comprehensive knowledge and appropriate imaging technique for diagnosis. To treat patients with chronic sphenoid rhinosinusitis, surgical treatment with endoscopic transnasal sphenoidotomy is often required. As there are no recent updated reviews of chronic sphenoid rhinosinusitis, in this article, we review the anatomy of the sphenoid sinus and its clinical relationship with the clinical signs and symptoms of the disease, the imaging findings of each diagnosis and the comprehensive surgical techniques.
Introduction
Rhinosinusitis is defined as inflammation of the nose and the paranasal sinuses characterized by clinical symptoms of either nasal obstruction or nasal discharge at times accompanied by facial pain or loss of smell. Endoscopic findings may reveal nasal polyposis or mucopurulent discharge or mucosal obstruction of the meatus. Mucosal changes within sinuses may also be observed by computed tomography (CT) scan.Citation1 Chronic rhinosinusitis is defined as clinical symptoms that last for at least 12 weeks without complete resolution.Citation1 Because there is no clear definition for chronic sphenoid rhinosinusitis, in this article, we define chronic sphenoid rhinosinusitis as a spectrum of either infective or inflammatory diseases occurring exclusively in sphenoid sinus, either in one or both sides, persisting for more than 12 weeks. This may include bacterial rhinosinusitis, fungal rhinosinusitis and mucocele.
Isolated sphenoid lesion is an uncommon condition with an increasing incidence.Citation2 Patients may present with nonspecific symptoms such as headache, facial pain and fullness. Nasal symptoms are frequently absent. Among the isolated sphenoid diseases, inflammatory lesions are the most common with an incidence of over 50%.Citation3–Citation5 They are now more frequently diagnosed due to better recognition of the disease by the primary clinician as well as improved availability of diagnostic tools such as endoscopy and imaging techniques including CT and magnetic resonance imaging (MRI). Early diagnosis with appropriate radiological evaluation and timely management are important factors to decrease the likelihood of permanent neuro-ophthalmological sequelae.Citation3 As there are no recent updated reviews of chronic sphenoid rhinosinusitis, in this article, we review the anatomy of the sphenoid sinus and its clinical relationship with the clinical signs and symptoms of the disease, the imaging findings of each diagnosis and the comprehensive surgical techniques.
Anatomy of sphenoid sinus
The sphenoid sinus develops after birth. The pneumatization progresses at the age of 6 years and is completed by the ninth to 12th year.Citation6 The youngest known patient who was diagnosed and reported as having sphenoiditis was 10 years old.Citation3 The sphenoid sinus lies posteriorly in the apex of the nasal cavity. The walls of this sinus adhere to the optic canal, dura mater, pituitary gland and cavernous sinus, which contain the internal carotid arteries, and the third, fourth, fifth and sixth cranial nerves. Infection of the cavity may directly spread to these structures due to the close proximity to the sinus cavity itself, often resulting in serious consequences.
Clinical manifestation
Patients with isolated chronic sphenoid rhinosinusitis may present with nonspecific symptoms and signs. Headache is the most common presentation, presenting in over 80% of cases.Citation4,Citation7,Citation8 Patients may have intermittent headaches for several years. The pain is described as either dull or sharp. It may commonly interfere with sleep and may not be relieved by analgesics.Citation2 The typical location of headache is retro-orbital or vertex.Citation7 Frontotemporal, fronto-orbital and hemicranial pain have been described as well.Citation9 The mechanism of headache is believed to be the irritation of the first and second branches of the trigeminal nerve, via the nasociliary and sphenopalatine nerves, which innervate sphenoid sinus.Citation9
Although cranial nerve involvements can be more commonly observed in sphenoid neoplasm, these presentations are not uncommon in sphenoiditis. Visual loss and other cranial nerve involvements were reported at an incidence of 12% in sphenoid rhinosinusitis presenting symptoms.Citation10 Visual deterioration may be caused by either inflammation involving the optic nerve in the case of bacterial rhinosinusitis or mass effect in the case of fungal ball or allergic fungal rhinosinusitis.Citation11,Citation12
Diplopia is the result of palsy of the third, fourth or sixth nerves due to the nearby location of the sphenoid and cavernous sinuses. The abducens nerve is the most commonly affected cranial nerve in isolated sphenoid sinusitis, and this effect may occur in isolation or in combination with other cranial palsies.Citation7,Citation12,Citation13
Physical examination
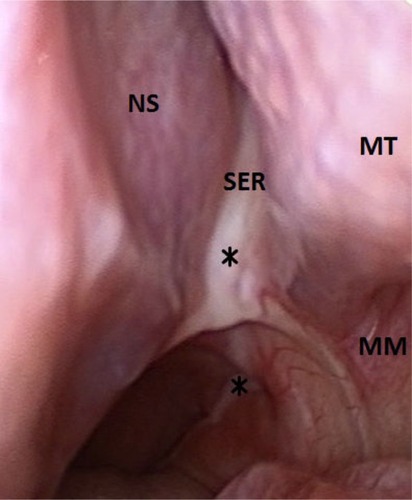
A rigid nasal endoscopy should be performed in every patient suspected of chronic sphenoiditis (). Although some patients may not report nasal symptoms, endoscopic examination may reveal various signs of inflammatory sphenoid disease such as mucopurulent discharge, edema or polyps in the sphenoethmoidal recess.Citation7 However, nasal endoscopy does not replace the necessity for imaging.Citation12 It is known that a normal-looking sphenoethmoidal recess on nasal endoscopy does not exclude sphenoid pathology.Citation7 On the other hand, the presence of mucopurulent discharge draining from the sphenoethmoidal recess should not be considered solely as bacterial infection. Advanced imaging study is still required to identify potential surgical cases.
Imaging studies
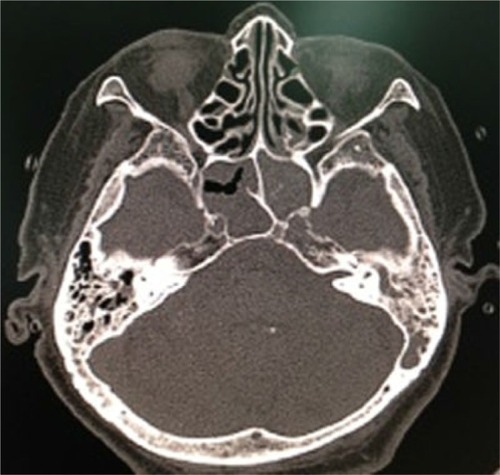
CT scan of the paranasal sinus is mandatory. It should always be performed to diagnose and provide a roadmap for sinus surgery.Citation12 A CT scan may differentiate inflammatory disease from neoplasm and bacterial from fungal infections with the different characteristics of mucosal and bone appearance of each disease. MRI is not always necessary; it is only required when intracranial or orbital extension is suspected to delineate the interface with neighboring structures and to rule out any associated intracranial pathology.Citation3 It may be useful in differentiating among mucoceles, benign tumors, encephaloceles and internal carotid artery aneurysm.Citation10
Surgical management
Only a few cases of chronic sphenoid rhinosinusitis were reported in the literature as medically responsive,Citation3 and the remaining required surgical intervention. Sphenoid sinus surgery is indicated when the diagnosis of bacterial sinusitis has been made with no clinical response to appropriate medical treatment during a certain period of 6–8 weeks and when the diagnosis of either fungal rhinosinusitis or mucocele has been made. Cases with cranial nerve involvements may require more urgent surgical treatment in order to timely restore or optimize all neural functions.
Endoscopic transnasal sphenoidotomy is acknowledged as the gold standard for surgical treatment of chronic sphe-noid rhinosinusitis.Citation3,Citation14 In comparison to external approaches, endoscopic surgery provides better visualization and thus allows for faster healing, better esthetic outcome, lower morbidity and higher success rate.Citation14 Sphenoid sinus can be opened with several techniques. The ostia can be directly approached. The sphenoid rostrum is approached between the middle and superior turbinate laterally and the septum medially. Unlike tumor surgery, resecting the inferior portion of the middle turbinate is usually not necessary. The sphenoid ostium is then widely opened and enlarged so that the infective or inflammatory content inside the sphenoid sinus cavity can be completely removed. Full inspection of the sphenoid sinus cavity is then performed to assure complete removal.
Some surgeons may prefer to approach the sphenoid sinus from the posterior ethmoid sinus.Citation15 Transethmoidal approach should be performed when patients have pathology in ethmoid sinus or extensive tumor. For cases in which the ostium cannot be identified, the use of a reliable landmark is essential. Orbital walls are fixed anatomical landmarks used when the sphenoid sinus ostium is not clearly seen.Citation16 The level of orbital floor is always below the sphenoid roof, and this indicates the level of sphenoid ostium.Citation16 The medial orbital wall indicates the lateral wall of the sphenoid sinus including the location of the optic nerve and the internal carotid artery. Traditionally, sphenoid sinus widening in an inferomedial fashion is widely suggested because it is safer when sphenoid face is resected away from vital structures. This may not be followed if the level of the sphenoid roof, optic nerve and internal carotid artery are clearly indicated by the inferior and medial orbital walls. Maximal opening of the sphenoid sinus can be achieved when it is widened superiorly and laterally.
Diseases of chronic sphenoid rhinosinusitis
Bacterial rhinosinusitis
Bacterial rhinosinusitis is the most common pathology in isolated inflammatory sphenoid lesion. Most studies reported in the literature do not clearly define their patient as having acute or chronic infection. It may be difficult to delineate the exact duration of the presenting symptom because the most common sphenoiditis presenting symptom of headache is nonspecific and may not be exactly recognizable. However, patients with chronic bacterial rhinosinusitis may look less severely ill than those with acute infection.Citation2 The presenting symptoms, as well as physical and endoscopic findings, may be indistinguishable from fungal rhinosinusitis or mucocele (). CT imaging may be the key to proper diagnosis. CT scan in chronic bacterial sphenoiditis may demonstrate abnormal findings of mucosal thickening, changes in air–fluid level and partial or complete opacification ().
Figure 2 Endoscopic finding of bacterial sphenoiditis.

Figure 3 CT finding of bacterial sphenoiditis.
Abbreviation: CT, computed tomography.
Once diagnosed, treatment with antibiotics for culture-based organisms is recommended.Citation2 Staphylococci have been reported as the most common cultured pathogen. Other pathogens that have been reported include Streptococcus pneumoniae, aerobic Gram-negative bacilli (Pseudomonas aeruginosa, Klebsiella pneumoniae, Haemophilus influenzae, Escherichia coli) and anaerobes (Peptostreptococcus, Fusobacterium, Prevotella and Porphyromonas).Citation2,Citation4,Citation7,Citation17,Citation18
Medical failure after comprehensive pharmacologic treatment with culture-based antibiotics, intranasal corticosteroids and topical decongestants within 6–8 weeks mandates surgery. However, surgical intervention may be required earlier in cases presenting with complications of cranial nerve involvements because early drainage of the sphenoid sinus may prevent persistent sequelae. Intraoperative findings of chronic bacterial sphenoiditis may include purulent discharge filled in the sinus cavity or mucosal thickening or polyps.
Fungal rhinosinusitis
Fungal rhinosinusitis can be broadly classified as invasive and noninvasive fungal rhinosinusitis. The invasive fungal rhinosinusitis can be distinguished from noninvasive disease by the presence of fungal invasion in sinus tissue from the histopathological study. Fungal rhinosinusitis is thought to comprise at least five subtypes;Citation19 however, only three subtypes might be diagnosed as chronic sphenoiditis which include chronic invasive fungal rhinosinusitis, allergic fungal rhinosinusitis and aspergilloma. The management of each subtype, as well as its prognosis, is different.
Aspergilloma
Aspergilloma or fungal ball is a noninvasive type of fungal rhinosinusitis. It is diagnosed when there is a dense conglomeration of hyphae and cheesy or clay-like material within the sinus cavity and when histopathology reveals chronic inflammatory mucosal response without eosinophil predominance, granulomatous response and evidence of tissue or vascular invasion.Citation12,Citation20 Although literature has previously reported fungal ball of sphenoid sinus as a rare entity,Citation7,Citation13,Citation21 it is now more commonly diagnosed with an incidence of 10–20% in more recent case series.Citation4,Citation8 The sphenoid sinus is acknowledged as the second most commonly involved sinus by fungal ball.Citation14 Patients usually have normal immunologic status. In published reports, it was more commonly diagnosed in elderly patients (over 50 years old), and female preponderance was observed.Citation22 Nasal endoscopic examinations should be performed; however, the examinations may not give any clue to the diagnosis as negative findings were reported for all 12 patients in the series by Lee et al.Citation22
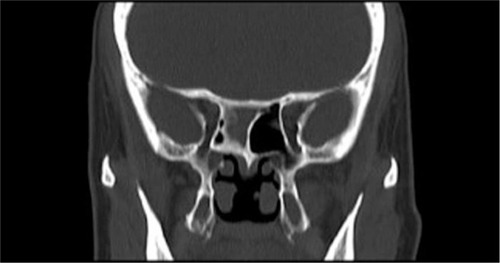
CT scan is an excellent tool for diagnosing sphenoid fungus ball. Typically, fungal ball appears as hyperattenuating in noncontrast CT due to dense-matted hyphae. The inflamed mucosal lining of the sinus is, however, hypoattenuating. Intrasinus metallic calcifications have been reported in 50% of cases.Citation14 The bone wall of the sinus may be sclerotic and thickened or expanded and thinned with focal areas of erosion from pressure necrosis (). Bone erosion has been reported in 63% of fungal ball cases and is not a sign of invasive fungal rhinosinusitis.Citation23 MRI findings show the fungal ball as hypointense on T1-weighted and T2-weighted images. Calcifications also generate areas of signal void on T2-weighted images.Citation24
Figure 4 CT finding of fungal ball sphenoiditis.
Abbreviation: CT, computed tomography.
Medical treatment is not successful for aspergilloma. Surgical intervention is always indicated.Citation12 Intraoperative findings may reveal fungal concrement with or without mucopurulent discharge (). The mucosa of the sphenoid sinus should have normal color. Sinus mucosa should be sent for histopathology. Tissue or vascular invasion indicates invasive fungal rhinosinusitis.Citation12
Allergic fungal sinusitis
Allergic fungal sinusitis (AFS) is another form of noninvasive fungal rhinosinusitis. Major criteria for diagnosis as proposed by Bent and Kuhn include the presence of nasal polyposis, characteristic sinus CT findings of heterogeneous hyperdensities that are often unilateral and asymmetric, type 1 hypersensitivity, eosinophilic mucin and positive fungal stain or culture.Citation25 Patients are immunocompetent. AFS typically demonstrates low signal intensity of the sinus contents on T1-weighted images on MRI. The T2 signal void is also observed, due to a high concentration of various metals concentrated by the fungal organism, as well as a high protein and dry content of the allergic mucin.Citation24 Bone erosion with bone remodeling is one of the most common clinical features of AFS which was reported in up to 50% of patients.Citation26 Thus, AFS in sphenoid sinus can easily cause compressive symptoms of cranial neuropathies which surround the sphenoid sinus. It was reported that cranial neuropathies develop at 10% of the sphenoid AFS with bone erosion.Citation26 Hyperprolactinemia and gynecomastia secondary to AFS compression of the pituitary gland were also reported as presenting symptoms of sphenoid AFS.Citation27,Citation28 To meet the criteria of diagnosis, nasal polyposis should be visible either when performing nasal endoscopic examination or during surgical treatment.
Treatment of AFS is surgery. Endoscopic sphenoidotomy with total removal of the thick mucin and fungal debris is the treatment of choice. It is essential that all sinuses involved be widely opened. In case of isolated sphenoid AFS, the sphenoid sinus should be maximally widened to optimize postoperative care and topical steroid therapy.Citation29,Citation30 Traditional endoscopic transnasal sphenoidotomy and traditional endoscopic sinus surgery with small-hole concept may not achieve this aim. Postoperative systemic steroids can be tapered off early if aggressive topical steroid therapy is effectively given. Histopathology should be performed with both specimens of sinus mucosa and mucin to confirm diagnosis of AFS. Immunotherapy is recommended postoperatively.
Chronic invasive fungal rhinosinusitis
Invasive fungal sinusitis is defined as fungal sinusitis in which mycotic organisms infiltrate sinus mucosa. Chronic invasive fungal sinusitis of isolated sphenoid sinus is rare. In most cases, the immunological status of patients is normal or only mildly abnormal. Presenting symptoms are often unspecific. Diagnosis should be suspected when patients have disease invasion to adjacent structures such as cranial nerve palsies or pituitary involvement. The disease can be difficult to differentiate from fungal ball by CT or MRI if there is no bone involvement. Focal or diffuse bone destruction is commonly observed. On the other hand, sclerotic bone changes are commonly noted as well.Citation31
Diagnosis can be made from material obtained intraoperatively from the sphenoid sinus and histopathological confirmation of fungal invasion within sinus mucosa. Aspergillus sp. is reported as the most common causative agent. The gold standard for treatment is radical surgical debridement with long-term use of systemic antifungal agents. As the sphenoid sinus is adjacent to several vital structures, extensive sphenoidectomy with aggressive mucosa removal may not be easily performed. Wide sphenoidotomy with long-term use of antifungal agents is an acceptable surgical management with a satisfying result.Citation32 Amphotericin B and voriconazole are both commonly prescribed for the treatment of invasive fungal disease.Citation32 Intraoperative findings may not be distinguished from fungal ball; however, intraoperative mucosal necrosis may be observed as a clue for invasive nature.Citation31 The presence of fungus ball suggests the potential of a previous fungal ball transformation into invasive fungal sphenoiditis.Citation31 The prognosis of chronic invasive fungal rhinosinusitis is rather poor with a report of 25% mortality rate.Citation31
Mucocele
Mucoceles are benign, encapsulated lesions filled with mucus and lined by epithelium. They are expansile and locally destructive with the ability to resorb bone, causing erosions of the bony walls of the sinus. Sphenoid sinus mucocele is quite common. It represents up to 20% of all paranasal sinus mucoceles.Citation33 The pathophysiology of this lesion is still unknown but is believed to be caused by obstruction of the sinus ostium, cystic dilatation of glandular structures or cystic development from embryonic epithelial residues.Citation34 Radiation exposure at head and neck area has also been postulated.Citation33
Sphenoid sinus mucocele may be asymptomatic. It is commonly discovered accidentally after CT or MRI of the head and neck region.Citation35 Patients with sphenoid sinus mucocele may become symptomatic when the mucocele compresses or displaces structures around sphenoid sinus. Clinical symptoms may mimic neoplasm. Thus, visual loss is more common in sphenoid sinus mucocele than in other inflammatory sphenoid diseases.
CT imaging is required to diagnose and to define the exact boundaries of the mucocele. Mucoceles may show various imaging features, depending on their contents. They often have low attenuation on CT, a low signal on T1-weighted MRI and a high signal on T2-weighted MRI, due to their watery content. There is usually no enhancement, or at most marginal enhancement, on CT and T1-weighted MRI, whereas many of the lesions in the differential diagnosis show contrast enhancement. In mucoceles with high protein content, T1-weighted MRI shows a lesion which is homogeneously hyperintense centrally with a surrounding rim of hypointense mucosa.Citation33
Medical treatment is not a successful option for mucocele. Asymptomatic mucocele does not mandate surgical treatment and can be followed up. Mucocele requires surgical intervention when it is symptomatic, shows rapid growth or has extensive involvement of the orbit and brain.
Conclusion
The condition discussed, key diagnostic findings, recommended imaging and treatment are summarized in . Comprehensive history taking, physical examination, endoscopic examination and advanced imaging studies provide appropriate clinical diagnosis. Histopathology and microbiology are important for definite diagnosis. Endoscopic sphenoidotomy is the treatment of choice and should be performed in a timely manner to prevent permanent sequelae.
Table 1 Summary of chronic sphenoid rhinosinusitis
Disclosure
The authors report no conflicts of interest in this work.
References
- FokkensWJLundVJMullolJEuropean position paper on rhinosinusitis and nasal polyps 2012Rhinology201250111222469599
- LewDSouthwickFSMontgomeryWWWeberALBakerASSphenoid sinusitis. A review of 30 casesN Eng J Med19833091911491154
- NourYAAl-MadaniAEl-DalyAGaafarAIsolated sphenoid sinus pathology: spectrum of diagnostic and treatment modalitiesAuris Nasus Larynx200835450050818242904
- FriedmanABatraPSFakhriSCitardiMJLanzaDCIsolated sphenoid sinus disease: etiology and managementOtolaryngol Head Neck Surg2005133454455016213927
- NgYHSethiDSIsolated sphenoid sinus disease: differential diagnosis and managementCurr Opin Otolaryngol Head Neck Surg2011191162021178620
- SomPMLawsonWFatterpekarGMZinreichSJEmbryology, anatomy, physiology, and imaging of the sinonasal cavitiesSomPMCurtinHDHead and Neck Imaging5th edSt LouisElsevier Health Sciences2011102165
- SethiDSIsolated sphenoid lesions: diagnosis and managementOtolaryngol Head Neck Surg1999120573073610229601
- MartinTJSmithTLSmithMMLoehrlTAEvaluation and surgical management of isolated sphenoid sinus diseaseArch Otolaryngol Head Neck Surg2002128121413141912479731
- LerouxEValadeDGuichardJPHermanPSphenoid fungus balls: clinical presentation and long-term follow-up in 24 patientsCephalalgia200929111218122319811505
- LawsonWReinoAJIsolated sphenoid sinus disease: an analysis of 132 casesLaryngoscope199710712 Pt 1159015959396670
- WangJKLinSYLaiPCJouJRCompressive optic neuropathy secondary to sphenoid sinus aspergillosisJ Neuroophthalmol20052927780
- CharakornNSnidvongsKIsolated oculomotor nerve palsy caused by fungal ball rhinosinusitis: a case report and literature reviewAsian Rhinol J2016315760
- WyllieJW3rdKernEBDjalilianMIsolated sphenoid sinus lesionsLaryngoscope1973838125212654758128
- PagellaFMattiEDe BernardiFParanasal sinus fungus ball: diagnosis and managementMycoses200750645145617944705
- StankiewiczJAThe endoscopic approach to the sphenoid sinusLaryngoscope19899922182212913432
- WuttiwongsanonCChaowanapanjaPHarveyRJThe orbital floor is a surgical landmark for the Asian anterior skull baseAm J Rhinol Allergy2015296e216e21926637573
- SocherJACassanoMFilheiroCACassanoPFelippuADiagnosis and treatment of isolated sphenoid sinus disease: a review of 109 casesActa Otolaryngol200812891004101019086308
- BrookIBacteriology of acute and chronic sphenoid sinusitisAnn Otol Rhinol Laryngol2002111111002100412450174
- deShazoRDChapinKSwainREFungal sinusitisN Engl J Med199733742542599227932
- deShazoRDO’BrienMChapinKCriteria for the diagnosis of sinus mycetomaJ Allergy Clin Immunol19979944754859111491
- RuoppiPSeppaJPukkilaMNuutinenJIsolated sphenoid sinus diseases: report of 39 casesArch Otolaryngol Head Neck Surg2000126677778110864116
- LeeTJHuangSFChangPHCharacteristics of isolated sphenoid sinus aspergilloma: report of twelve cases and literature reviewAnn Otol Rhinol Laryngol2009118321121719374153
- PandaNKBalajiPChakrabartiASharmaSCReddyCEParanasal sinus aspergillosis: its categorization to develop a treatment protocolMycoses200447727728315310329
- AribandiMMcCoyVABazanC3rdImaging features of invasive and noninvasive fungal sinusitis: a reviewRadiographics20072751283129617848691
- BentJP3rdKuhnFADiagnosis of allergic fungal sinusitisOtolaryngol Head Neck Surg199411155805887970796
- IllingEADunlapQWoodworthBAOutcomes of pressure-induced cranial neuropathies from allergic fungal rhinosinusitisOtolaryngol Head Neck Surg2015152354154525583853
- MenendezJYWoodworthBAJohnstonJMJrGynecomastia and hyperprolactinemia secondary to advanced allergic fungal rhinosinusitis in a pediatric patientTurk Neurosurg201626116616826768883
- ChapurinNWangCSteinbergDMJangDWHyperprolactinemia secondary to allergic fungal sinusitis compressing the pituitary glandCase Rep Otolaryngol20162016726070726998375
- SnidvongsKKalishLSacksRSivasubramaniamRCopeDHarveyRJSinus surgery and delivery method influence the effectiveness of topical corticosteroids for chronic rhinosinusitis: systematic review and meta-analysisAm J Rhinol Allergy201327322123323710959
- SnidvongsKPrattEChinDSacksREarlsPHarveyRJCorticosteroid nasal irrigations after endoscopic sinus surgery in the management of chronic rhinosinusitisInt Forum Allergy Rhinol20122541542122566474
- LeeDHYoonTMLeeJKJooYEParkKHLimSCInvasive fungal sinusitis of the sphenoid sinusClin Exp Otorhinolaryngol20147318118725177433
- BaumannAZimmerliSHauslerRCaversaccioMInvasive sphenoidal aspergillosis: successful treatment with sphenoidotomy and voriconazoleORL J Otorhinolaryngol Relat Spec200769212112617159376
- SoonSRLimCMSinghHSethiDSSphenoid sinus mucocele: 10 cases and literature reviewJ Laryngol Otol20101241444719825255
- KoslingSHintnerMBrandtSSchulzTBlochingMMucoceles of the sphenoid sinusEur J Radiol20045111515186877
- GiovannettiFFiliaciFRamieriVUngariCIsolated sphenoid sinus mucocele: etiology and managementJ Craniofac Surg20081951381138418812867