Abstract
Introduction
Thrombocytopenia is a common hematologic abnormality during pregnancy. Pregnant women with thrombocytopenia have a higher risk of bleeding excessively during or after childbirth, particularly if they need to have a cesarean section or other surgical intervention during pregnancy, labor or in the puerperium. The main aim of this study was to determine the prevalence of thrombocytopenia among pregnant women attending antenatal care service at Gondar University Hospital, northwest Ethiopia.
Materials and methods
A cross-sectional study was used to assess the prevalence of thrombocytopenia among pregnant women attending antenatal care service at Gondar University Hospital from January to April 2015. A total of 217 pregnant women were included in the study and a structured pretested questionnaire was used to obtain sociodemographic information, nutritional factors, obstetrics and gynecological factors, history and clinical condition. Blood samples were collected for platelet count and other platelet parameters, which were determined by using SysmexKX 21 automation. The data were entered to Epi info version 6 software and analyzed using SPSS version 20 software. Bivariable and multivariable statistical analyses were used to evaluate the effect of independent variable over the dependent variable. A p-value of <0.05 was considered as statistically significant.
Result
A total of 217 women receiving antenatal care service at Gondar University Hospital participated in the study. Thrombocytopenia among 19 pregnant women showed a prevalence of 8.8%. The mean ± standard deviation platelet count was 238.85×109/L (±74.57). Thrombocytopenia was significantly associated with patients who lived rurally (crude odds ratio =4.3, 95% confidence interval 1.48–12.76).
Conclusion
The prevalence of thrombocytopenia was 8.8% predominantly with mild type of thrombocytopenia. Thrombocytopenia was higher among pregnant women who lived rurally. Therefore, health care providers should screen routinely for thrombocytopenia to avoid excessive bleeding during pregnancy, especially in women who live rurally.
Introduction
Platelets are nonnucleated blood cells formed by cellular fragments of megakaryocytes, and they have a critical role in maintaining hemostasis.Citation1 Thrombocytopenia is suspected when a patient’s platelet count is <150,000×103/mm3. The normal reference range for platelet count in a nonpregnant woman is 150,000–400,000× 103/mm3. Due to hemodilution secondary to expansion of plasma volume, platelet count in normal pregnancies may be decreased by ~10%; most of the decrease in platelet count occurs during the third trimester of pregnancy,Citation2–Citation5 although the absolute platelet count remains within normal reference range in most patients.Citation3,Citation6 Thrombocytopenia can be classified as mild (platelet count of 100,000–150,000× 103/mm3), moderate (platelet count of 50,000–100,000× 103/mm3) or severe (platelet count <50,000×103/mm3).Citation1
During pregnancy, most cases of low platelet count are due to gestational thrombocytopenia (GT), idiopathic thrombocytopenic purpura (ITP) or preeclampsia.Citation7 Other causes include infection, such as malaria or folate deficiency, and diseases, such as leukemia and aplastic anemia.Citation4 GT is characterized by incidental detection of mild-to-moderate reduction in platelet count during pregnancy in otherwise healthy women with no previous history of ITP or conditions known to be associated with thrombocytopenia. It is not an early manifestation of autoimmune disease, there is no significant fetal or maternal morbidity, and normalization of platelet counts occur in the vast majority of patients postpartum.Citation7–Citation10 GT is responsible for ~75% of thrombocytopenia in pregnant women.Citation7 GT is usually mild and is not usually associated with fetal thrombocytopenia.11 Platelet count in patients with GT is usually >110,000×103/mm3, whereas counts as low as 70,000×103/mm3 have been reported. In patients with platelet count <70,000×103/mm3, an alternative explanation is frequently present. Although the pathogenesis of GT is not well understood, it may involve factors such as hemodilution and/or accelerated platelet clearance.Citation12,Citation13 It is known that pregnant women with thrombocytopenia have a higher risk of bleeding excessively during or after childbirth, particularly if they need to have a cesarean section or other surgical intervention during pregnancy or labor. Such bleeding complications are more likely when the platelet count is <50×103/mm3.Citation1
Thrombocytopenia during pregnancy has become a cause for unnecessary, often invasive, additional testing and cesarean deliveries. The evaluation and treatment of this condition can be expensive and distressing to the patient and can result in an adverse outcome. Obstetricians in our locality have no comprehensible guide for managing pregnant women with thrombocytopenia due to a lack of data about the frequency, severity and causes of this condition. Moreover, no relevant data are available from other parts of Ethiopia. Therefore, this study was aimed at determining the prevalence of thrombocytopenia among pregnant women attending antenatal care service at Gondar University Hospital, and estimating the proportions of the underlying causes that can give valuable information for the management of thrombocytopenia-related complications in pregnant women.
Materials and methods
Study settings and study population
An institutional-based cross-sectional study design was used to assess the prevalence of thrombocytopenia among pregnant women attending the antenatal care service at Gondar University Hospital from January to April 2015. All women between the ages of 15–49 years who visited Gondar University Hospital for antenatal care during the study period were the source population.
Data collection
Women who visited the antenatal care unit at Gondar University Hospital during the study period participated in the study. Pregnant women on anti-inflammatory drugs, had a bleeding disorder, splenomegaly, or hypertension, or were on antiretro-viral treatment were excluded from the study. After obtaining written informed consent, sociodemographic nutritional factors, obstetrics and gynecological factors, history and clinical condition were collected from each study participant using a pretested structured questionnaire, those who had normal blood pressure, were free from malaria parasites and had no platelet aggregation on peripheral film examination were included in the study.
Two milliliters of venous blood was collected under aseptic conditions and transferred in to ethylene diamine tetra acetic acid (EDTA) anticoagulant tubes by mixing for 5 minutes. The specimens were labeled with identification number of each study participant. The EDTA anticoagulant specimens were kept at room temperature until analysis was done for a maximum of 4 hours after specimen collection. The complete blood cell counts were determined using SysmexKX 21 analyzer (Sysmex Corporation, Bellport, NY, USA) which applies electric impedance principle (Sysmex user manual, 2002) following the manufacturer’s instructions.
The reliability of the study findings was guaranteed by implementing quality control (QC) measures throughout the whole process of the laboratory work. All materials, equipment and procedures were adequately controlled. Sysmex were checked for linearity and validity by using lower, medium and high quality control reagents. Preanalytical, analytical and postanalytical stages of quality assurance that were incorporated in standard operating procedures were strictly followed. Appropriate volume of blood and anticoagulant was used to maintain the specimen’s quality. Every day before the samples were investigated, control reagents with low, medium and high concentration were simultaneously investigated by the Sysmex machines to maintain the reagents quality. In addition, thin blood films stained with Wright stain were prepared for all blood samples, to confirm thrombocytopenia and exclude the presence of platelet aggregation and malaria parasites.
Data processing
The data were entered, cleaned and analyzed using SPSS statistical computer software version 20 (IBM Corporation, Armonk, NY, USA). Summary statistics such as frequencies and percentages were calculated. Logistic regression was used to identify the associated factors with thrombocytopenia. A 95% confidence interval and a p-value <0.05 were considered as statistically significant.
Ethical approval
Ethical approval was obtained from the University of Gondar, School of Biomedical and Laboratory Sciences Ethical Clearance Committee, and a permission letter was obtained from Gondar University Hospital Chief Executive Officer before going ahead with the study. Each study participant were asked to participate voluntarily and provided written informed consent to participate in the study. Parental consent was obtained for participants <16 years of age. Confidentiality was kept throughout the collection and processing of specimens. Each study participant were informed about the objective of the study. Voluntary participation and the right to withdraw at any time were emphasized. In addition to this, any study subject with an abnormal test result were referred to their physicians for further investigation and management.
Results
Sociodemographic characteristics of study participants
In this study, a total of 217 woman from the antenatal care at Gondar University Hospital were included in this study. One hundred and sixty-nine (77.8%) of the study subjects were aged <30 years. The mean (± standard deviation [SD]) age of the study participants were 25.67 (±4.69) years. Most of the study subjects (192 [88.3%]) lived in an urban residence. Among the study subjects, 215 (99.1%) were married and 137 (63.1%) were housewives by occupation. Among the study subjects, 35 (16.1%) were unable to read and write (illiterate; ).
Table 1 Sociodemographic characteristics of pregnant women attending antenatal care service at Gondar University Hospital in 2014, northwest Ethiopia
Reproductive characteristics of pregnant women attending antenatal care at Gondar University Hospital in 2014, northwest Ethiopia
Among the study subjects, 38.2%, 36.9% and 24.9% were in the third, second and first trimester, respectively. The mean number of children that the women had were 2, with 2.3% having only one child and 47% having three and more children ().
Table 2 Reproductive characteristics of pregnant women attending antenatal care service at Gondar University Hospital in 2014, northwest Ethiopia
Hematological profiles of the study subjects
The mean (± SD) hematologic profiles of the study subjects were platelet count 238.85+74.57×109/L, white blood cell (WBC) count 9.35+2.85×109/L and red blood cell (RBC) count 4.43+0.40×1012/L ().
Table 3 Hematologic profiles of pregnant women attending antenatal care service at Gondar University Hospital in 2014, northwest Ethiopia
Prevalence of thrombocytopenia
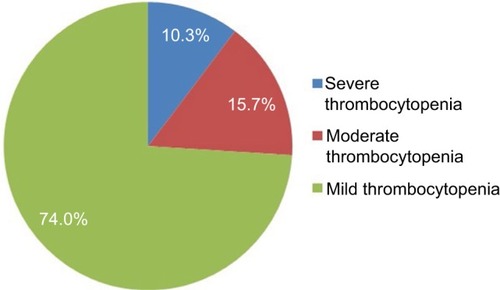
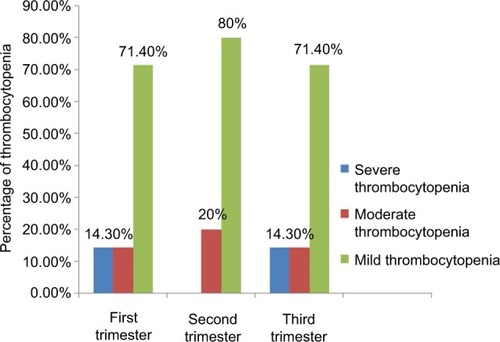
The prevalence of thrombocytopenia in this study was found in 19 women (8.8%), the remaining 198 (92.2%) women had a platelet count in the normal range. Among the thrombocytopenic pregnant women in this study, 74% had mild thrombocytopenia, 15.7% had moderate thrombocytopenia and 10.3% had severe thrombocytopenia ( and ).
Factors associated with thrombocytopenia
Factors associated with thrombocytopenia were assessed by logistic regression and showed that living in a rural residence showed women were approximately four times more likely to develop thrombocytopenia than women living in an urban area (crude odds ratio [COR]=4.35, 95% confidence interval 1.48–12.76) ().
Table 4 Factors associated with thrombocytopenia among pregnant women attending antenatal care service at Gondar University Hospital in 2014, northwest Ethiopia
Discussion
This study was conducted in order to determine the prevalence of thrombocytopenia among pregnant women attending the antenatal care at Gondar University Hospital. In this study, the prevalence of thrombocytopenia among pregnant women was 8.8%. In this study, the prevalence of thrombocytopenia among pregnant women was 8.8%, which was almost comparable to the results of studies conducted by Vyas et alCitation14 (7.67%), Nisha et alCitation15 (8.8%), DwivedilCitation16 (8.17%), Shamoon et alCitation17 (8%), MyersCitation18 literature review (8%–10%), Jeffrey et alCitation19 clinical review (8%), and Jodkowska et alCitation20 (7%–10%). However, the result of this study was lower than in studies conducted in Switzerland (11.6%),Citation21 Ethiopia (13.5%),Citation22 Ghana (15.3%),Citation23 Israel (21.8%),Citation24 and Nigeria (13.5%).Citation25 The difference may be due to sociodemographic differences of the study subjects and differences in the study design. Among the thrombocytopenic pregnant women in our study, 74% had mild thrombocytopenia, 15.7% had moderate thrombocytopenia and 10.3% had severe thrombocytopenia. These results are in line with studies conducted in Ethiopia, Ghana, India and Nigeria14,22,23,25,26 which showed a high frequency presence of mild type thrombocytopenia. This study showed that there was no association between the trimesters and thrombocytopenia (p>0.05). This result is similar with previous studies conducted in Ethiopia.Citation22
In summary, thrombocytopenia is a crucial problem among pregnant women with the prevalence of thrombocytopenia shown to be 8.8%, dominantly mild type thrombocytopenia. Thrombocytopenia was higher among pregnant women in the study area who were from a rural residence. For this reason, screening of pregnant women should include a platelet count, especially if they reside in a rural area.
Limitation of the study
The study was a cross-sectional study and it did not include control groups. Since this study is not a follow-up study, it may lack many independent factors of thrombocytopenia assessment.
Author contributions
FA conceived and designed the study, was involved in the literature review and wrote and edited the final draft of the article.
BE and ZG collected the data, carried out the data and statistical analysis and were involved in literature review, writing and editing of the final draft. All authors approved the final version of the manuscript.
Acknowledgments
We would like to acknowledge the Department of Haematology, School of Biomedical and Laboratory Sciences, University of Gondar, for all the support to conduct this research work. We also would like to extend our deepest appreciation to the study participants for their willingness in providing the information set for the study.
Disclosure
The authors report no conflicts of interest in this work.
Reference
- KatkeRDGohilDPThrombocytopenia during pregnancy: an institutional based studyInt J Reprod Contracept Obstet Gynecol201434947951
- SainioSKekomakiRRiikononSTeramoKMaternal thrombocytopenia at term: a population-based studyActa Obstet Gynecol Scand200079974474910993097
- BoehlenFHohlfeldPExtermannPPernegerTVde MoerloosePPlatelet count at term pregnancy: a reappraisal of the thresholdObstet Gynecol2000951293310636497
- McCraeKRThrombocytopenia in pregnancy: differential diagnosis, pathogenesis, and managementBlood Rev200317171412490206
- BallemPJHematological problems of pregnancyCan Fam Physician1988342531253721253125
- BoehlenFThrombocytopenia during pregnancy: importance, diagnosis and managementHamostaseologie2006261727416444327
- BurrowsRFKeltonJGFetal thrombocytopenia and its relation to maternal thrombocytopeniaN Engl J Med199332920146314668413457
- RuggeriMSchiavottoCCastamanGTosettoARodeghieroFGestational thrombocytopenia: a prospective studyHaematologica19978233413429234586
- SamuelsPBusselJBBraitmanLEEstimation of the risk of thrombocytopenia in the offspring of pregnant women with presumed immune thrombocytopenic purpuraN Engl J Med199032342292352366833
- HowHYBergmannFKoshyFIdiopathic thrombocytopenic purpura: a practice guideline developed by explicit methods for the American Society of HaematologyBlood19968813408704187
- ShehataNBurrowsRKeltonJGGestational thrombocytopeniaClin Obstet Gynecol199942232733410370851
- KadirRAMcLintockCThrombocytopenia and disorders of platelet function in pregnancySemin Thromb Hemost201137664065222102267
- VyasRupaShahSComparative study of mild versus moderate to severe thrombocytopenia in third trimester of pregnancy in a tertiary care hospitalNHL J Med Sci201431811
- NishaSAmitaDUmaSTripathiAKPushplataSPrevalence of and characterization of thrombocytopenia in pregnancy in India womenIndian J Hematol Blood Transfus2012282778123730013
- DwivediPPuriMNigamAAgarwalKFetomaternal outcome in pregnancy with severe thrombocytopeniaEur Rev Med Pharmacol Sci201216111563156623111971
- ShamoonRPMuhammedNSJaffMSPrevalence and etiological classification of thrombocytopenia among a group of pregnant women in Erbil City, IraqTurk J Hematol20092623123128
- MyersBThrombocytopenia in pregnancyObstert Gynecol2009113177183
- JeffreyALevyCPTMCFSLanceDMurphyMDThrombocytopenia in pregnancyJ Am Board Fam Pract200215290712150462
- JodkowskaAMartynowiczHKaczmarek-WdowiakBMazurThrombocytopenia in pregnancy – pathogenesis and diagnostic approachPostepy Hig Med Dosw (Online)20156901215122126561848
- BoehlenFHohlfeldPExtermannPPernegerTVde MoerloosePPlatelet count at term pregnancy: a reappraisal of the thresholdObstet Gynecol2000951293310636497
- BelaynehFG/MariamASolomonFThe prevalence of thrombocytopenia, and associated factors among pregnant women attending antenatal care at Hawassa University Referral Teaching and HospitalJ Harmoniz Res Med Hlth Sci201524175182
- OlayemiEAkuffoFWGestational thrombocytopenia women among pregnant Ghanaian womenPan Afr Med J2012123422891092
- ParnasMSheinerEShoham-VardiIModerate to severe thrombocytopenia during pregnancyEur J Obstet Gynecol Reprod Biol20061281–216316816533554
- AjibolaSOAkinbamiAAdewumiAGestational thrombocytopenia women among pregnant women in Legos NigeriaNiger Med J201455213914324791048