Abstract
Avatrombopag is an orally-administered small molecule thrombopoietin receptor agonist. It was the third thrombopoietin receptor agonist approved for the treatment of immune thrombocytopenia and the first approved to treat periprocedural thrombocytopenia in patients with chronic liver disease (thereby providing an alternative to blood transfusions for these patients). Unlike eltrombopag, avatrombopag does not require a 4 hr food-restricted window around its use and it has not been associated with hepatotoxicity in ITP patients or portal vein thrombosis in patients with chronic liver disease. In ITP patients it can often be dosed less frequently than once daily. It is overall well-tolerated with a side-effect profile similar to placebo in randomized clinical trials. This article will review the clinical development, efficacy, safety, and pharmacology of avatrombopag for use in patients with ITP and thrombocytopenia of chronic liver disease.
Introduction
Thrombopoietin (TPO) is a glycoprotein hormone synthesized and secreted by the liver and acts as one of the main regulators of platelet productionCitation1 and activation.Citation2,Citation3 First the recombinant thrombopoietins and now the thrombopoietin receptor agonists (TPO-RAs) have been developed for clinical use to mimic endogenous TPO function and increase the platelet count in patients with thrombocytopenia.Citation1
TPO-RAs have been shown to be effective in the treatment of several conditions including immune thrombocytopenia (ITP),Citation4,Citation5 aplastic anemia,Citation6,Citation7 thrombocytopenia associated with chronic hepatitis C infection,Citation8 and as a preprocedural measure for patients with thrombocytopenia requiring surgery.Citation9–Citation12 Studies also suggest these drugs are effective in the treatment of chemotherapy-induced thrombocytopeniaCitation13,Citation14 and thrombocytopenia associated with myelodysplastic syndrome.Citation15–Citation17 There are currently four TPO-RAs on the market: romiplostim, eltrombopag, avatrombopag, and lusutrombopag ().
Table 1 Comparison of the commercially-available thrombopoietin receptor agonists.Citation20,Citation42,Citation43
Most patients with mild to moderate thrombocytopenia do not require treatment, and most patients with chronic liver disease (CLD) fall into this category. For these patients, treatment is generally only necessary in the case of active bleeding, profoundly low platelet counts, impending myelosuppression, and in the perioperative setting. Data demonstrates that patients with thrombocytopenia have an increased risk of various operative complications, including bleeding, sepsis, adverse pulmonary outcomes, renal complications, blood transfusion requirements, and 30-day mortality.Citation18 Platelet transfusion remains the mainstay of treatment for perioperative thrombocytopenia, but may be ineffective in certain populations, carry all of the risks of blood product transfusion, and are a scarce resource.Citation19 With effective TPO-RA treatment, patients with known thrombocytopenia undergoing elective procedures could undergo pharmacologic platelet count optimization prior to surgery, which would preserve platelet transfusion for acute surgical indications. TPO-RA treatment would also offer an option for patients who refuse platelet transfusion and those with immune barriers to response (such as immune thrombocytopenia or alloimmunization).
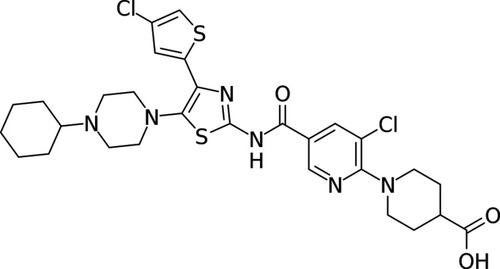
Avatrombopag (Doptelet) () is a TPO-RA that obtained its first approval in May 2018 for the treatment of periprocedural thrombocytopenia in patients with CLD based on the results of two large phase III clinical trials.Citation20 Phase II and phase III trials demonstrating efficacy in patients with ITP have also been published.Citation21 Avatrombopag was recently approved by the US FDA under a supplemental new drug application for treatment of chronic ITP. Here we will review the development, clinical trials, pharmacology, and safety of avatrombopag in patients with ITP and thrombocytopenia of CLD.
Drug development and mechanism of action
Initial strategies to discover small molecule thrombopoietin receptor agonists involved high-throughput screening for molecules capable of stimulating reporter genes (eg, STAT) in TPO-dependent cell lines, leading to the discovery of both eltrombopag and avatrombopag. In vitro experiments on human CB CD34+ cells found that Avatrombopag led to the maturation of megakaryocytes with similar morphological features to those stimulated by recombinant human TPO (rhTPO), suggesting a similar effect to TPO in vitro. STAT5 activity assays with platelets from twelve species, including humans, showed that avatrombopag led to phosphorylation of STAT5 in human and chimpanzee platelets, without binding to other homologs.Citation22 By contrast, rhTPO is able to activate human and chimpanzee platelets, as well as those from several other primates and mammals.Citation23
Further experiments in NOD/SCID mice looked to evaluate the action of avatrombopag in vivo. Human fetal liver CD34+ cells were transplanted into NOD/SCID mice, with human platelets appearing four weeks after transplant. Administration of avatrombopag led to an increase in the production of human platelets without having an effect on murine counts.Citation23 These results have been validated in humans with CLD associated thrombocytopenia, with avatrombopag administration leading to increased platelet counts as compared to placebo. However, patients on avatrombopag were not found to have increased levels of activated circulating platelets, as measured with flow cytometry. Furthermore, platelets extracted from patients on avatrombopag did not respond with an increased sensitivity to platelet activators in vitro. Avatrombopag does not therefore, fully mimic the effects of endogenous TPO, as its action is on platelet count and not reactivity.Citation24
However, while not mimicking endogenous TPO, avatrombopag does work synergistically with TPO, as opposed to other agonists, such as romiplostim, which may block TPO binding.Citation25 Avatrombopag in combination with rhTPO elevated platelet counts up to 200% more than TPO alone, as well as increasing the size of the hematopoietic progenitor and megakaryocytic progenitor pool to a greater degree than TPO alone.Citation25
Clinical trials
Treatment of periprocedural thrombocytopenia in CLD patients
In a Phase II multicenter, randomized, placebo-controlled, double-blind study, 130 adults with cirrhosis and platelet counts in the range of 10–58×109/L were randomized to receive either avatrombopag at a variety of doses or placebo for one week before surgery.Citation26 The primary end point of the study was an increase in platelet count ≥20×109/L and at least one platelet count >50×109/L during days 4–8 of the eight-day protocol. Analysis found that among two separate cohorts and five different dosing patterns, all but one showed significantly more patients reaching the endpoint in the avatrombopag group as compared to placebo, with 47.0% of patients reaching primary endpoint in Cohort A, as compared to 6.3% in the placebo group, and 47.6% of patients reaching primary endpoint in Cohort B as compared to 9.5% in the placebo group. A dose-response relationship was observed in both cohorts. The drug was well tolerated by most patients, with the overall incidence of adverse events similar between the avatrombopag and placebo groups.
Two similarly-designed phase III randomized, double-blind, placebo-controlled trials followed: ADAPT-1 took place at 75 sites across 20 countries and ADAPT-2 took place at 74 sites across 16 countries, which examined the use of avatrombopag in adults with thrombocytopenia (platelets ≤50×109/L) and CLD [MELD (Model for End-Stage Liver Disease) ≤24]. All participants were scheduled for a procedure with an associated risk of bleeding, with the primary endpoint of the study being the proportion of patients not requiring a rescue procedure or hemostatic medication for bleeding or a platelet transfusion up to 7 days after the scheduled procedure. Patients were excluded for a variety of conditions, including a history of thrombosis, hematologic disorders, cardiovascular disease, the use of blood thinners, or prior avatrombopag use.Citation9
Patients enrolled in the study assigned to a low baseline platelet count (<40×109/L) or high baseline platelet count cohort (40 to <50 x 109/L), and then randomized 2:1 to receive avatrombopag or placebo. Patients in the low baseline platelet count cohort received 5 doses of 60 mg each, while patients in the high baseline platelet count cohort received 5 doses of 40 mg each. Data from both studies concluded that patients on avatrombopag had a decreased need for rescue procedures, such as platelet transfusion, as compared to patients on placebo (). In ADAPT-1, 66% of patients in the low baseline platelet count group and 88% in the high baseline platelet count group achieved the primary endpoint as opposed to 23% and 38% on placebo, respectively. Similar results were seen in ADAPT-2, with 69% of patients in the low baseline platelet count group and 88% in the high baseline platelet count group achieved primary endpoint as opposed to 35% and 33% on placebo, respectively. This data was consistent regardless of age, sex, race, region, MELD score, Child-Turcotte-Pugh class, or disease etiology.Citation9 Furthermore, the mean change in platelet count from baseline, and the percentage of patients achieving a platelet count >50 x 109/L was significantly higher in patients receiving avatrombopag in both studies.
Table 2 Primary and secondary efficacy endpoints in phase III trials of avatrombopag for the management of periprocedural thrombocytopenia in CLD
Treatment of immune thrombocytopenia
Avatrombopag was recently FDA approved under a supplemental new drug application for the treatment of chronic ITP in adult patients who have failed other therapies. The use of avatrombopag to treat ITP has been examined in two major clinical trials. A Phase II trial randomized 64 subjects with ITP for at least 3 months to a variety of doses of avatrombopag or placebo, and found that avatrombopag led to increased platelet count with few adverse effects.Citation21 A Phase III multicenter, double-blind trial followed, randomizing 49 patients with chronic ITP and platelet counts <30 x 109/L to receive either 20 mg/day of avatrombopag or placebo. Before randomization, patients were stratified by splenectomy status, baseline platelet count, and use of other ITP medications. The study found superiority of the avatrombopag arm in the number of cumulative weeks without rescue therapy (12.4 vs 0.0 weeks), and demonstrated an increased platelet response rate (65.63% vs 0.0%) and decreased concomitant ITP medication use.Citation27
Dosing
Following the design of the ADAPT-1 and ADAPT-2 trials, avatrombopag dosing recommendations for periprocedural management of thrombocytopenia in patients with CLD are 60 mg per day for 5 days if the baseline platelet count is <40×109/L or 40 mg per day for 5 days if the count is 40–50×109/L for any procedure taking place 5–8 days after the last dose.Citation28 Of note, the FDA label does not restrict use to the sort of minor procedures included in the ADAPT-1 and ADAPT-2 trials. For ITP, the label advises use of the lowest dose of avatrombopag needed to achieve and maintain a platelet count ≥50×109/L, starting with 20 mg daily with food. Platelet counts are to be assessed weekly and dose titrated to maintain a platelet count between 50–200×109/L. There are six dose levels, from a maximum dose of 40 mg daily to a minimum dose of 20 mg once weekly.Citation28
Ongoing clinical trials
There is one Phase III trial of avatrombopag currently enrolling patients, evaluating the efficacy and safety of avatrombopag use in patient with chemotherapy-induced thrombocytopenia who are receiving chemotherapy for the treatment of ovarian, lung, or bladder cancer (ClinicalTrials.gov Identifier NCT03471078). This trial is currently recruiting participants and is estimated to be complete in November 2025.
Safety
So far, the general safety of avatrombopag has been tested in healthy subjects,Citation29 thrombocytopenic CLD patients,Citation9 and patients with ITP.Citation21,Citation27 An overview of the findings can be seen in (). Of note, the only population that has received the medication for a more prolonged amount of time (months to years) are patients with ITP.
Table 3 Prevalence of adverse events in avatrombopag trials
Avatrombopag has been generally well tolerated across trials, with few serious adverse effects, and no deaths reported. It is of particular interest that thrombotic events were reported in two studies. In ADAPT trials, there was one portal vein thrombosis in a patient on avatrombopag (who had a peak platelet count below 100×109/L); by comparison, there was one patient on the placebo arm who developed pulmonary embolism and another that had an acute myocardial infarction.Citation9 In one of the ITP studies, patients on avatrombopag reported stroke, MI, renal artery occlusion, deep vein thrombosis, and superficial thrombophlebitis. Concerns for portal vein thrombosis are of particular concern in the treatment of CLD patients with TPO-RAs as a prior randomized, controlled trial of eltrombopag for periprocedural thrombocytopenia in these patients found an increased incidence of portal vein thrombosis in the eltrombopag arm, leading to the trial being stopped prematurely.Citation30 The ADAPT-1 and ADAPT-2 studies did not find an increased risk of thrombotic events in patients taking avatrombopag, but these trials were not powered to assess thrombotic risk.Citation9
Pharmacology
Avatrombopag has poor aqueous solubility, leading to slow gut absorption and a peak plasma concentration (Cmax) that is reached 5–9 hrs after administration. However, the solubility of avatrombopag does not affect its absorption in the tested range (20–60 mg), as Cmax and AUC (area under the curve) both increase proportionally with dose.Citation29,Citation31 The terminal half-life is approximately 16–19 hrs.Citation29,Citation32 Volume of distribution does increase with body weight (measured in the range of 39–175 kg); this change was statistically significant but not clinically significant.Citation31 The pharmacokinetics of avatrombopag are significantly impacted varied by age, sex, hepatic disease, or renal dysfunction.Citation28 The pharmacologic properties of avatrombopag are summarized in .
Table 4 Summary of key pharmacokinetic parameters of avatrombopag
In stark contrast to eltrombopag, avatrombopag absorption is not reduced by dietary fat or divalent cations (such as calcium).Citation28,Citation33,Citation34 Taking avatrombopag in the fed state actually reduces inter-subject variability in pharmacokinetic parameters, though it does not affect the rate or extent of absorption within a subject. In phase III trials, avatrombopag was given under fed conditions. The dietary restrictions required in patients taking eltrombopag (a four-hour restricted window around the dose) can affect compliance or quality of life, and indeed dosing regimens involving administration less frequently than once daily have been developed to address this.Citation35 While such a protocol not necessary in patients receiving avatrombopag for dietary reasons, the ITP dose titration protocol described in the prescribing information utilizes this exact dosing strategy and is successful given the relatively long terminal half-life of avatrombopag and the underlying kinetics of thrombopoiesis.
Model development showed that a pharmacokinetic/pharmacodynamic model with a linear dose effect was superior to other models in tracking the effect of dose adjustments and co-administered drug interactions.Citation31 The final model showed production rate increasing 1.17% per 1 ng/mL increase in plasma avatrombopag concentration. Pharmacokinetic/pharmacodynamic modeling of avatrombopag shows an overall linear relationship between platelet response and plasma avatrombopag concentration. There were statistically significant effects of race (East Asian), TPO level, and albumin on the slope parameter, with each of these factors decreasing the dose effect. These are not currently believed to be of clinical relevance in CLD patients,Citation31 as opposed to eltrombopag which does show clinically significant differences in the platelet response between East Asian and white patients.The impact of baseline endogenous TPO level and platelet response to avatrombopag has not been well-studied in ITP patients, but evidence suggests a clinically-significant inverse relation between endogenous TPO level and platelet response to both eltrombopag and romiplostim in patients with ITP.Citation36–Citation38
Relative potency of the TPO-RAs is often questioned. In healthy volunteers assessed in different studies, romiplostim was approximately 8 times more potent than eltrombopag at increasing the platelet count and avatrombopag was approximately 3 times more potent than eltrombopag at increasing the platelet count.Citation29,Citation39 This may be true in patients with various thrombocytopenias, such as ITP, but requires confirmation.Citation40
Drug metabolism
Avatrombopag is metabolized in equal proportions by two cytochrome P450 (CYP) enzymes, CYP2C9 and CYP3A.Citation31 The avatrombopag and its metabolites are mainly excreted in feces (88%); 34% of the drug is excreted in the feces unmetabolized.Citation29 CYP2C9 polymorphisms which are known to decrease enzyme activity have been studied and showed that these “intermediate metabolizers” have a higher exposure to avatrombopag, possibly due to decreased clearance and therefore increased circulating plasma avatrombopag levels. These polymorphisms are more common in whites as compared to the Asian population (18% vs 3%).Citation29 Trials have not suggested these polymorphisms lead to a clinically significant difference in response to avatrombopag.
A study in 48 healthy volunteers examined the pharmacokinetic properties of avatrombopag when administered alone and in with with fluconazole (moderate inhibitor of CYP2C9 and CYP3A), itraconazole (strong CYP3A inhibitor), or rifampin (strong inducer of CYP3A and moderate inducer of CYP2C9). Data showed that administration of avatrombopag with fluconazole increased the AUC by 2.16-fold and extended the half-life by 20 hrs. Itraconazole increased the AUC by 1.37-fold, with the half-life extended by 8.4 hrs. Rifampin, the inducer of CYP3A and CYP2C9, decreased the AUC by 0.568-fold, decreasing the half-life by 10 hrs. The substantial impact of fluconazole on pharmacokinetic parameters suggests that CYP2C9 plays a more dominant role in avatrombopag metabolism than CYP3A.Citation41 However, for the dosing regimens currently used, the effects of CYP inducers and inhibitors were found to be clinically insignificant, as well as lacking any safety concerns, and so dose adjustments are not currently required.Citation31
Conclusion
Avatrombopag is a TPO receptor agonist currently approved for periprocedural use in patients with thrombocytopenia secondary to chronic liver disease as well as immune thrombocytopenia. The drug is effective at increasing platelet counts and is generally well-tolerated. Unlike eltrombopag, avatrombopag can be taken without dietary restrictions and does not show significant differences in platelet response based on race. Avatrombopag-drug interactions appear to be generally clinically insignificant. Additional study is ongoing to assess the use of avatrombopag to treat chemotherapy-induced thrombocytopenia.
Author contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Acknowledgment
HA is the recipient of the National Hemophilia Foundation-Shire Clinical Fellowship Award, which provides partial salary support.
Disclosure
Dr Hanny Al-Samkari report personal fees and research funding from Agios and Dova, and personal fees from Moderna, outside the submitted work. The authors report no other conflicts of interest in this work.
References
- Kuter DJ. The biology of thrombopoietin and thrombopoietin receptor agonists. Int J Hematol. 2013;98(1):10–23. doi:10.1007/s12185-013-1382-023821332
- Rodriguez-Linares B, Watson SP. Thrombopoietin potentiates activation of human platelets in association with JAK2 and TYK2 phosphorylation. Biochem J. 1996;316(Pt 1):93–98. doi:10.1042/bj31600938645238
- Pasquet JM, Gross BS, Gratacap MP, et al. Thrombopoietin potentiates collagen receptor signaling in platelets through a phosphatidylinositol 3-kinase-dependent pathway. Blood. 2000;95(11):3429–3434.10828025
- Kuter DJ, Rummel M, Boccia R, et al. Romiplostim or standard of care in patients with immune thrombocytopenia. N Engl J Med. 2010;363(20):1889–1899. doi:10.1056/NEJMoa100262521067381
- Cheng G, Saleh MN, Marcher C, et al. Eltrombopag for management of chronic immune thrombocytopenia (RAISE): a 6-month, randomised, phase 3 study. Lancet. 2011;377(9763):393–402. doi:10.1016/S0140-6736(10)60959-220739054
- Desmond R, Townsley DM, Dumitriu B, et al. Eltrombopag restores trilineage hematopoiesis in refractory severe aplastic anemia that can be sustained on discontinuation of drug. Blood. 2014;123(12):1818–1825. doi:10.1182/blood-2013-10-53474324345753
- Townsley DM, Scheinberg P, Winkler T, et al. Eltrombopag added to standard immunosuppression for aplastic anemia. N Engl J Med. 2017;376(16):1540–1550. doi:10.1056/NEJMoa161387828423296
- Afdhal NH, Dusheiko GM, Giannini EG, et al. Eltrombopag increases platelet numbers in thrombocytopenic patients with HCV infection and cirrhosis, allowing for effective antiviral therapy. Gastroenterology. 2014;146(2):442–452 e441. doi:10.1053/j.gastro.2013.10.01224126097
- Terrault N, Chen YC, Izumi N, et al. Avatrombopag before procedures reduces need for platelet transfusion in patients with chronic liver disease and thrombocytopenia. Gastroenterology. 2018;155:705–718. doi:10.1053/j.gastro.2018.05.02529778606
- Tateishi R, Seike M, Kudo M, et al. A randomized controlled trial of lusutrombopag in Japanese patients with chronic liver disease undergoing radiofrequency ablation. J Gastroenterol. 2019;54(2):171-181.
- Afdhal N, Duggal A, Ochiai T, et al. Platelet response to lusutrombopag, a thrombopoietin receptor agonist, in patients with chronic liver disease and thrombocytopenia undergoing non-emergency invasive procedures: results form a Phase 3 randomized, double-blind, placebo-controlled study. Blood. 2017;130:291(Abstract).
- Al-Samkari H, Marshall AL, Goodarzi K, Kuter DJ. Romiplostim for the management of perioperative thrombocytopenia. Br J Haematol. 2018;182(1):106–113. doi:10.1111/bjh.1528029767837
- Al-Samkari H, Marshall AL, Goodarzi K, Kuter DJ. The use of romiplostim in treating chemotherapy-induced thrombocytopenia in patients with solid tumors. Haematologica. 2018;103(4):e169–e172. doi:10.3324/haematol.2017.18016629242295
- Soff GA, Miao Y, Devlin SM, et al. Romiplostim for Chemotherapy-Induced Thrombocytopenia (CIT). Results of a Phase 2 trial. Blood. 2017;130:289(Abstract).
- Wang ES, Lyons RM, Larson RA, et al. A randomized, double-blind, placebo-controlled phase 2 study evaluating the efficacy and safety of romiplostim treatment of patients with low or intermediate-1 risk myelodysplastic syndrome receiving lenalidomide. J Hematol Oncol. 2012;5:71. doi:10.1186/1756-8722-5-7123190430
- Giagounidis A, Mufti GJ, Fenaux P, et al. Results of a randomized, double-blind study of romiplostim versus placebo in patients with low/intermediate-1-risk myelodysplastic syndrome and thrombocytopenia. Cancer. 2014;120(12):1838–1846. doi:10.1002/cncr.2866324706489
- Kantarjian HM, Giles FJ, Greenberg PL, et al. Phase 2 study of romiplostim in patients with low- or intermediate-risk myelodysplastic syndrome receiving azacitidine therapy. Blood. 2010;116(17):3163–3170. doi:10.1182/blood-2010-03-27475320631375
- Glance LG, Blumberg N, Eaton MP, et al. Preoperative thrombocytopenia and postoperative outcomes after noncardiac surgery. Anesthesiology. 2014;120(1):62–75. doi:10.1097/ALN.0b013e3182a4441f23903021
- Nagrebetsky A, Al-Samkari H, Davis NM, Kuter DJ, Wiener-Kronish JP. Perioperative thrombocytopenia: evidence, evaluation, and emerging therapies. Br J Anaesth. 2019;122(1):19–31. doi:10.1016/j.bja.2018.09.01030579402
- Shirley M. Avatrombopag: first global approval. Drugs. 2018;78(11):1163-1168.
- Bussel JB, Kuter DJ, Aledort LM, et al. A randomized trial of avatrombopag, an investigational thrombopoietin-receptor agonist, in persistent and chronic immune thrombocytopenia. Blood. 2014;123(25):3887–3894. doi:10.1182/blood-2013-07-51439824802775
- Kuter DJ. New thrombopoietic growth factors. Blood. 2007;109(11):4607–4616. doi:10.1182/blood-2006-10-01931517289815
- Fukushima-Shintani M, Suzuki K, Iwatsuki Y, et al. AKR-501 (YM477) a novel orally-active thrombopoietin receptor agonist. Eur J Haematol. 2009;82(4):247–254. doi:10.1111/j.1600-0609.2008.01198.x19183407
- Michelson AD, Smolensky Koganov E, Forde EE, Carmichael SL, Frelinger AL 3rd. Avatrombopag increases platelet count but not platelet activation in patients with thrombocytopenia resulting from liver disease. J Thromb Haemost. 2018;16(12):2515–2519. doi:10.1111/jth.1429530264918
- Fukushima-Shintani M, Suzuki K, Iwatsuki Y, et al. AKR-501 (YM477) in combination with thrombopoietin enhances human megakaryocytopoiesis. Exp Hematol. 2008;36(10):1337–1342. doi:10.1016/j.exphem.2008.04.02018619724
- Terrault NA, Hassanein T, Howell CD, et al. Phase II study of avatrombopag in thrombocytopenic patients with cirrhosis undergoing an elective procedure. J Hepatol. 2014;61(6):1253–1259. doi:10.1016/j.jhep.2014.07.00725048952
- Jurczak W, Chojnowski K, Mayer J, et al. Phase 3 randomised study of avatrombopag, a novel thrombopoietin receptor agonist for the treatment of chronic immune thrombocytopenia. Br J Haematol. 2018;183:479–490. doi:10.1111/bjh.2018.183.issue-330191972
- Dova Pharmaceuticals. Doptelet (avatrombopag) tablets: US prescribing information; Published 2018 Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/210238s000lbl.pdf. Accessed 71, 2019.
- Nomoto M, Pastino G, Rege B, Aluri J, Ferry J, Han D. Pharmacokinetics, pharmacodynamics, pharmacogenomics, safety, and tolerability of avatrombopag in healthy Japanese and white subjects. Clin Pharm Drug Dev. 2018;7(2):188–195. doi:10.1002/cpdd.349
- Afdhal NH, Giannini EG, Tayyab G, et al. Eltrombopag before procedures in patients with cirrhosis and thrombocytopenia. N Engl J Med. 2012;367(8):716–724. doi:10.1056/NEJMoa111070922913681
- Nomoto M, Ferry J, Hussein Z. Population pharmacokinetic/pharmacodynamic analyses of avatrombopag in patients with chronic liver disease and optimal dose adjustment guide with concomitantly administered CYP3A and CYP2C9 inhibitors. J Clin Pharmacol. 2018;58:1629–1638. doi:10.1002/jcph.v58.1229905956
- Desjardins RE, Tempel DL, Lucek R, Kuter DJ. Single and multiple doses of AKR-501 (YM477) increase the platelet count in healthy volunteers. Blood. 2006;108(11):477. doi:10.1182/blood-2006-03-013334
- Williams DD, Peng B, Bailey CK, et al. Effects of food and antacids on the pharmacokinetics of eltrombopag in healthy adult subjects: two single-dose, open-label, randomized-sequence, crossover studies. Clin Ther. 2009;31(4):764–776. doi:10.1016/j.clinthera.2009.04.01019446149
- Wire MB, Bruce J, Gauvin J, et al. A randomized, open-label, 5-period, balanced crossover study to evaluate the relative bioavailability of eltrombopag powder for oral suspension (PfOS) and tablet formulations and the effect of a high-calcium meal on eltrombopag pharmacokinetics when administered with or 2 hrs before or after PfOS. Clin Ther. 2012;34(3):699–709. doi:10.1016/j.clinthera.2012.01.01122336488
- Al-Samkari H, Kuter DJ. An alternative intermittent eltrombopag dosing protocol for the treatment of chronic immune thrombocytopenia. Br J Clin Pharmacol. 2018;84(11):2673–2677. doi:10.1111/bcp.1371730032487
- Makar RS, Zhukov OS, Sahud MA, Kuter DJ. Thrombopoietin levels in patients with disorders of platelet production: diagnostic potential and utility in predicting response to TPO receptor agonists. Am J Hematol. 2013;88(12):1041–1044. doi:10.1002/ajh.2356223913253
- Kuter DJ, Meibohm A, Lopez A. TPO concentrations and response to romiplostim. Am J Hematol. 2014;89(12):1155–1156. doi:10.1002/ajh.2381825132329
- Al-Samkari H, Kuter DJ. Thrombopoietin level predicts response to treatment with eltrombopag and romiplostim in immune thrombocytopenia. Am J Hematol. 2018;93(12):1501–1508. doi:10.1002/ajh.2527530187942
- Jenkins JM, Williams D, Deng Y, et al. Phase 1 clinical study of eltrombopag, an oral, nonpeptide thrombopoietin receptor agonist. Blood. 2007;109(11):4739–4741. doi:10.1182/blood-2006-11-05796817327409
- Al-Samkari H, Kuter DJ. Relative potency of the thrombopoietin receptor agonists eltrombopag, avatrombopag and romiplostim in a patient with chronic immune thrombocytopenia. Br J Haematol. 2018;183(2):168. doi:10.1111/bjh.2018.183.issue-229978577
- Nomoto M, Zamora CA, Schuck E, et al. Pharmacokinetic/pharmacodynamic drug-drug interactions of avatrombopag when coadministered with dual or selective CYP2C9 and CYP3A interacting drugs. Br J Clin Pharmacol. 2018;84(5):952–960. doi:10.1111/bcp.1351729341245
- Kim ES. Lusutrombopag: first global approval. Drugs. 2016;76(1):155–158. doi:10.1007/s40265-015-0525-426666417
- Kuter DJ. Romiplostim. Cancer Treat Res. 2011;157:267–288. doi:10.1007/978-1-4419-7073-2_1621052962
- Al-Samkari H. Avatrombopag maleate for the treatment of periprocedural thrombocytopenia in patients with chronic liver disease. Drugs Today. 2018;54(11):647–655. doi:10.1358/dot.2018.54.11.289944130539164