Abstract
Purpose
Acute promyelocytic leukemia (APL) constitutes 5–10% of all cases of newly diagnosed acute myeloid leukemia. However, data on the epidemiology and risk factors for acute kidney injury (AKI) in patients with newly diagnosed APL are lacking. This study determined the incidence rate of AKI during induction chemotherapy for patients with newly diagnosed APL and the risk factors for AKI.
Patients and Methods
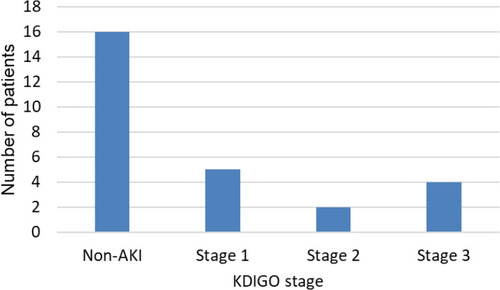
We conducted a retrospective observational study of patients with newly diagnosed APL in the Shonan Kamakura General Hospital between April 2004 and April 2020. Data of 27 patients with newly diagnosed APL were analyzed. The patients were classified as no AKI and AKI stages 1, 2 or 3.
Results
The incidence rate of AKI during induction chemotherapy was 40% (11/27). Among patients who developed AKI, four patients experienced AKI stage 3, and two patients required renal replacement therapy. No significant differences were found in the white blood cell count and baseline renal function between the groups; however, D-dimer and C-reactive protein levels upon admission were significantly higher in patients with AKI than in patients without AKI. Among patients who developed AKI, in hospital mortality at 90 days was 36% (4/11), which was significantly higher than among patients without AKI (p = 0.02). Patients who developed AKI were administered vancomycin more frequently, while almost all blood culture results were negative.
Conclusion
Incidence of AKI development in patients with newly diagnosed APL during induction chemotherapy was approximately 40%. Moreover, patients who developed AKI tended to be administered vancomycin more frequently. Unnecessary use of vancomycin should be avoided in patients with newly diagnosed APL, and using alternative non-nephrotoxic drugs should be considered for patients at risk of AKI.
Introduction
Acute promyelocytic leukemia (APL) accounts for approximately 5–10% of all cases of newly diagnosed acute myeloid leukemia (AML) and frequently presents in combination with coagulation disorders, including a high risk of life-threatening intracerebral hemorrhages.Citation1 Treatment for APL has dramatically changed the management and outcome of the disease over the two decades after the introduction of highly active drugs, including all-trans retinoic acid (ATRA) and arsenic trioxide (ATO).Citation2
However, differentiation syndrome is a potentially fatal complication of the treatment for APL and epidemiology studies have revealed that the incidence of early death in patients with APL remains high.Citation3,Citation4 Differentiation syndrome is characterized by unexplained fever, acute respiratory distress with interstitial pulmonary infiltrates, and/or acute kidney injury (AKI) due to capillary leakage.Citation5 The pathogenesis of the syndrome is considered as microvascular damage, since similar histologic findings are found in a variety of diseases (including trauma, sepsis, and adult respiratory distress syndrome).Citation6
In addition, a number of situations, such as tumor lysis syndrome, sepsis, decreased cardiac output, or drug toxicity, may lead to AKI. Even small changes in the serum creatinine levels are associated with increased mortality; thus, early identification of patients at risk and application of preventive strategies and treatment are fundamental for reducing its incidence.Citation7
Patients with hematological malignancies, more often experience AKI associated with sepsis, hypovolemia, and nephrotoxic drugs, given their differential characteristics. A previous study has revealed that AKI occurred in 36% of patients with AML and high-risk myelodysplastic syndrome undergoing induction chemotherapy.Citation8 Moreover, AKI is common in patients with newly diagnosed high-grade malignancies and is associated with lower complete remission and higher mortality rates.Citation8,Citation9
However, there are limited epidemiological data, and risk factors for AKI in patients with newly diagnosed APL is lacking. Prevention is the best method for avoiding AKI, with early identification of patients at risk and controlling the potentially modifiable risk factors, including the non-prescription or discontinuation of nephrotoxic drugs.Citation10 This study aimed to investigate the incidence of AKI during induction chemotherapy for patients with newly diagnosed APL and determine the risk factors for AKI.
Patients and Methods
We conducted a retrospective observational study of all patients with newly diagnosed APL in the Shonan Kamakura General Hospital between April 2004 and April 2020; APL diagnosis was confirmed according to clinical presentations, morphological criteria of the French-American-British classification, cytogenetic assay for t (15; 17) (q22; q21), and reverse transcription polymerase chain reaction assay for promyelocytic leukemia-retinoic acid receptor α transcripts. The study institution is a 629-bed tertiary care hospital that provides advanced medical care (including stem cell transplant) and admits more than 200 patients with hematological malignancies annually.
Clinical data for patients with APL who underwent induction chemotherapy were retrospectively collected and reviewed. Among these patients, we examined the incidence of AKI within 28 days of admission; AKI was confirmed according to the Kidney Disease Improving Global Outcomes Clinical Practice Guideline (KDIGO) criteria. The patients were classified as no AKI (KDIGO 0) and AKI stages 1, 2 or 3, according to the changes in serum creatinine (sCr) levels;Citation11 severity of AKI was categorized as stage 1 (increase in sCr levels 1.5–1.9 times the baseline value or ≥0.3 mg/dL); stage 2 (increase in sCr levels 2.0–2.9 times the baseline value); or stage 3 (increase in sCr levels ≥3.0 times the baseline value, or ≥4.0 mg/dL, or initiation of renal replacement therapy).
The following information was also collected: demographic data; laboratory data; sequential organ failure assessment score on admission;Citation12 induction regimen; presence of differentiation syndrome (presence of any of the following signs and symptoms: unexplained fever, weight gain, peripheral edema, dyspnea with interstitial pulmonary infiltrates, pleural and pericardial effusions, hypotension, and acute renal failure);Citation13 use of antibiotics, including cefepime, vancomycin (VCM), meropenem, piperacillin-tazobactam, amikacin, and amphotericin B, within 28 days of admission; blood culture results; intensive care unit (ICU) admission; renal replacement therapy for renal indications; use of mechanical ventilation; and mortality within 90 days following induction chemotherapy. The following criteria were used to exclude patients from this analysis: age under 18 years, patients undergoing chronic dialysis, lack of accurate medical records, and patients who underwent induction chemotherapy in other hospitals.
The study was conducted in agreement with the tenets of the Declaration of Helsinki. This retrospective observational study was approved by the Ethics committee from the institutional review board of the Shonan Kamakura General Hospital in Japan. Because this was a retrospective study using patients’ data obtained from the electronic health records, the institutional review board and medical ethics committee waived the need for written informed consent from the participants.
Statistical Analyses
Data are presented as median (25th–75th percentile) for continuous variables, and frequency (percentage) for qualitative variables. Nonparametric data were analyzed using the Mann–Whitney U (two independent samples) or the Kruskal–Wallis tests (more than two groups) with Dunn’s post hoc test. Categorical data were analyzed using the Fisher’s exact test for two variables. All tests were two-tailed, with results considered significant if p <0.05. All statistical analyses were performed using SPSS statistics, version 23.0 (IBM Japan, Ltd., Tokyo, Japan).
Results
The search strategy initially identified 29 patients; however, two patients were excluded, based on the exclusion criteria. Finally, data of 27 patients with newly diagnosed APL were analyzed in this study. Baseline characteristics of the patients are summarized in . Patients’ median age at initiation of induction chemotherapy was 61 (35–73) years; 63% (17/27) were men. Baseline renal function parameters were sCr level of 0.81 (0.70–0.99) mg/dl and estimated glomerular filtration rate level of 68.6 (59.7–87.5) mL/min/1.73 m2. Of the 27 patients, all were administered ATRA, and 16 patients were administered a combination of ATRA and idarubicin and/or cytarabine; 59% (16/27) of patients developed differentiation syndrome, and 15% (4/27) underwent mechanical ventilation.
Table 1 Patient Characteristics in All Patients
According to the KDIGO classification, AKI was observed in 11 (40.7%) patients. Neither age at diagnosis, white blood cell (WBC) count, platelet count, and fibrinogen level, nor baseline renal function parameters significantly differed between patients with and without AKI. However, D-dimer and C-reactive protein levels were significantly higher in patients with AKI at admission than in patients without AKI. A total of four (15%) patients died during induction chemotherapy. Among patients with AKI, 45% (5/11) required ICU admission, and 36% (4/11) required mechanical ventilation. Moreover, 82% (9/11) had previous exposure to vancomycin, a percentage that was significantly higher than that among patients without AKI (p = 0.01). Among patients who developed AKI, in hospital mortality at 90 days was 36% (4/11), which was significantly higher than patients without AKI (p = 0.02).
Of all patients, 19% (5/27) had AKI stage 1, 7% (2/27) had AKI stage 2, and 15% (4/27) had AKI stage 3 (two patients required renal replacement therapy). () The median time from the initiation of induction chemotherapy to the peak in sCr level for AKI was 10 (5–15) days (); summarizes the demographic data and clinical characteristics of the patients who developed stage 3 AKI. All four patients were administered vancomycin during induction chemotherapy; however, all blood culture results were negative despite multiple separate blood cultures from one patient. Of the four patients who developed stage 3 AKI, three patients had the highest through >20 mg/L. Mortality curves of the outcomes after induction chemotherapy are shown in . The overall mortality rate was 15% (4/27) at 90 days.
Figure 2 Number of patients who developed AKI and time from the initiation of induction chemotherapy to peak creatinine level in AKI.
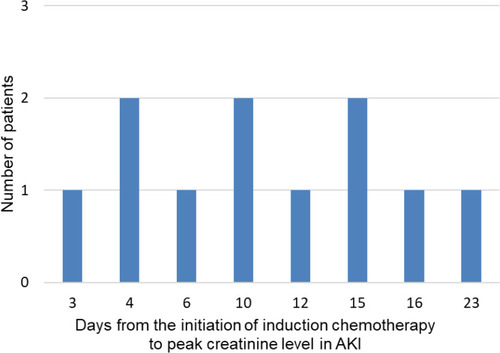
Figure 3 Kaplan–Meier survival curves of 90-day survival for AKI compared with non-AKI in newly diagnosed APL patients. Survival at 90 days was significantly lower in patients with an AKI (p=0.01).
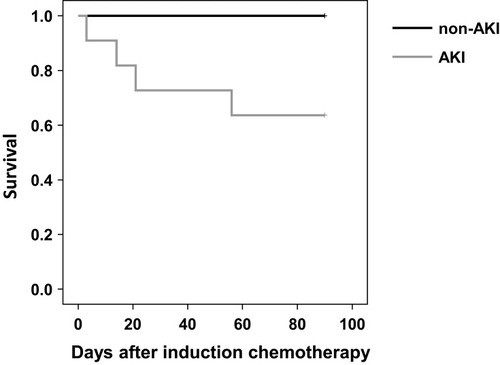
Table 2 Characteristics of Patients Who Developed Stage 3 AKI
Discussion
The incidence rate of AKI during induction chemotherapy for patients with newly diagnosed APL was 40.7% in this study. Among patients who developed AKI, four patients experienced AKI stage 3, and two patients required renal replacement therapy. No significant differences were found between the groups, with respect to WBC count and baseline renal function; however, D-dimer and C-reactive protein levels at admission in patients with AKI were significantly higher than those in patients without AKI because patients with AKI were administered vancomycin significantly more frequently.
Our findings support previous research regarding the risk of AKI among patients with newly diagnosed high-grade hematological malignancies.Citation8,Citation9,Citation14 Reported independent risk factors for AKI among patients with hematologic malignancies include age ≥55 years, mechanical ventilation, use of vancomycin, diuretics, amphotericin B lipid formulations, vasopressors, leukopenia, hypoalbuminemia, and non‐fludarabine-based chemotherapy.Citation8 Although differentiation syndrome is the main life-threatening complication of differentiating agents in patients with APL, epidemiology of AKI in newly diagnosed patients with APL is still lacking.Citation15 Therefore, we provide evidence from demographic data regarding the prevalence and risk factors of AKI among patients with newly diagnosed APL. Because the etiology of AKI is significantly associated with the 6-month complete response rate and 28-day mortality,Citation9,Citation16 Identifying patients who are at risk of developing AKI during induction chemotherapy is essential.
Chamoun et al have revealed that that old age, high creatinine levels, low hemoglobin counts, hypoalbuminemia at the time of diagnosis, and an elevated total volume of blood product transfusions were significant predictors of early death in patients with APL who were treated with ATRA and ATO (with or without gemtuzumab ozogamicin).Citation17 Consistent with the study, we found that patients with AKI had higher hospital mortality at 90 days than patients without AKI. Although discussing the general prevention of AKI in patients with hematological malignancies is difficult, management of acute kidney injury involves fluid resuscitation, avoidance of nephrotoxic medications, and contrast media exposure. Diuretics do not have a proven role in reducing the incidence of tumor lysis syndrome and their routine use is not recommended, unless there are clinical signs or symptoms of volume overload.Citation18 Conversely, fluid overload was found to be the most significant clinical factor associated with ICU transfers and endotracheal intubation in patients with APL;Citation17 thus, early intervention with aggressive diuresis and early renal replacement therapy should be considered.
Additionally, we found that patients who developed AKI were more frequently administered vancomycin than patients without AKI. Vancomycin is a commonly used tricyclic glycopeptide antibiotic, which is considered the antibiotic-of-choice, primarily for infections involving methicillin-resistant Staphylococcus aureus.Citation19 Because vancomycin has been plagued with concerns about nephrotoxicity, there is a vancomycin-associated measurable risk of AKI.Citation19,Citation20 Lahoti et al have identified that use of vancomycin was the significant independent risk factor (odds ratio: 2.3) for AKI in patients with acute myelogenous leukemia or high-risk myelodysplastic syndrome.Citation8 In a previous study that has investigated the factors associated with VCM-induced AKI in 150 patients with hematologic malignancies, multivariate analysis revealed that the risk factors of VCM-induced AKI were an initial VCM trough concentration of >15 mg/L.Citation21 Our finding that three-fourths patients who developed stage 3 AKI had the highest through >20 mg/L is consistent with this result. A retrospective study has shown that the target through vancomycin concentration of approximately 11.5 μg/mL is favorable for febrile neutropenia in patients with hematological malignancies.Citation22 Therefore, we need to monitor more closely vancomycin serum levels to allow dose adjustment.
In this study, 82% patients with AKI were administered vancomycin within 28 days of admission; however, almost all blood culture results were negative despite multiple separate blood cultures. While patients with hematological malignancies are often neutropenic due to the disease or during chemotherapy for it, our result suggested that unnecessary use of vancomycin might lead to an increased risk of AKI. A study that evaluated the use of empirical vancomycin for patients with febrile neutropenia (with regard to adherence to treatment guidelines) has revealed that inappropriate use of empirical vancomycin was observed in >30% of patients.Citation23 Vancomycin is still widely used to treat febrile neutropenia in patients with hematological malignancies, by potentially increasing toxicity. A recent analysis of a large cohort of critically ill adults being administered empirical vancomycin found that gram-positive cocci were identified within 48 h, during almost all episodes of methicillin-resistant Staphylococcus aureus bacteremia.Citation24 These findings may inform the timing of discontinuation of empirical vancomycin among patients with hematological malignancies. Moreover, intravenous vancomycin treatment is associated with a higher risk for kidney injury; thus, using an alternative non-nephrotoxic drug (such as linezolid) should be considered for patients at risk of AKI.Citation25
Our study had some limitations. First, this is a retrospective study; multiple unmeasured variables may have affected the outcomes, and conclusions should be validated by certain prospective studies in the future. Secondly, this study was performed in a single center; hence, population size was comparatively small. Thus, we thought it would be impractical to conduct a multivariate analysis on such a small number of cases. Therefore, causal association between AKI and administration of vancomycin is not entirely clear. A larger study group could have revealed other risk factors for AKI. However, the findings of this study offer new, potentially useful information for this patient population; APL has become the most curable subtype of adult AML. However, early death rate in APL remains high.Citation26 Several studies have already shown that the risk of AKI among patients with newly diagnosed high-grade hematological malignancies and patients with AKI had significantly higher mortality rates than patients without AKI.Citation8,Citation9 Further studies, specifically designed to investigate the incidence rate of AKI during induction chemotherapy between APL and other subtypes of acute myeloid leukemia are needed.
Conclusion
We found that the incidence of AKI development in patients with newly diagnosed APL during induction chemotherapy was approximately 40%. Patients who developed AKI tended to be administered vancomycin more frequently, while almost all blood culture results were negative. Therefore, unnecessary use of vancomycin should be avoided in patients with newly diagnosed APL, and using alternative non-nephrotoxic drugs should be considered for patients at risk of AKI. Preventing the development of AKI during APL induction chemotherapy is essential.
Abbreviations
AKI, acute kidney injury; AMK, Amikacin; APL, acute promyelocytic leukemia; AraC, cytarabine; ATO, arsenic trioxide; ATRA, all-trans retinoic acid; CFPM, Cefepime; CR, complete response; DNR, daunorubicin; eGFR, estimated glomerular filtration rate; IDR, idarubicin; KDIGO, Kidney Disease Improving Global Outcomes Clinical Practice Guideline; MEPM, Meropenem; PIPC/TAZ, Piperacillin-Tazobactam; RRT, renal replacement therapy; sCr, serum creatinine; SOFA, sequential organ failure assessment; VCM, Vancomycin.
Data Sharing Statement
The data used to support the findings of this study are available and may be released upon application to the corresponding author.
Acknowledgments
The authors thank all of the physicians and staff at the hospital for their help in this study.
Disclosure
The authors report that they have no conflict of interest.
References
- Sant M, Allemani C, Tereanu C, et al. Incidence of hematologic malignancies in Europe by morphologic subtype: results of the haemacare project. Blood. 2010;116(19):3724–3734. doi:10.1182/blood-2010-05-28263220664057
- Sanz MA, Lo-Coco F. Modern approaches to treating acute promyelocytic leukemia. Clin Infect Dis. 2011;29(5):495–503. doi:10.1200/JCO.2010.32.1067
- Montesinos P, Bergua JM, Vellenga E, et al. Differentiation syndrome in patients with acute promyelocytic leukemia treated with all-trans retinoic acid and anthracycline chemotherapy: characteristics, outcome, and prognostic factors. Blood. 2009;113(4):775–783. doi:10.1182/blood-2008-07-16861718945964
- Lehmann S, Ravn A, Carlsson L, et al. Continuing high early death rate in acute promyelocytic leukemia: a population-based report from the Swedish Adult Acute Leukemia Registry. Leukemia. 2011;25(7):1128–1134. doi:10.1038/leu.2011.7821502956
- Siddall E, Khatri M, Radhakrishnan J. Capillary leak syndrome: etiologies, pathophysiology, and management. Kidney Int. 2017;92(1):37–46. doi:10.1016/j.kint.2016.11.02928318633
- Tallman MS, Andersen JW, Schiffer CA, et al. Clinical description of 44 patients with acute promyelocytic leukemia who developed the retinoic acid syndrome. Blood. 2000;95:90–95.10607690
- Chertow GM, Burdick E, Honour M, Bonventre JV, Bates DW. Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol. 2005;16(11):3365–3370. doi:10.1681/ASN.200409074016177006
- Lahoti A, Kantarjian H, Salahudeen AK, et al. Predictors and outcome of acute kidney injury in patients with acute myelogenous leukemia or high-risk myelodysplastic syndrome. Cancer. 2010;116(17):4063–4068. doi:10.1002/cncr.2530620564156
- Canet E, Zafrani L, Lambert J, et al. Acute kidney injury in patients with newly diagnosed high-grade hematological malignancies: impact on remission and survival. PLoS One. 2013;8(2):e55870. doi:10.1371/journal.pone.005587023457485
- Meersch M, Schmidt C, Hoffmeier A, et al. Prevention of cardiac surgery-associated AKI by implementing the KDIGO guidelines in high risk patients identified by biomarkers: the prevAKI randomized controlled trial. Intensive Care Med. 2017;43(11):1551–1561. doi:10.1007/s00134-016-4670-328110412
- Summary of recommendation statements. Kidney Int Suppl. 2012;2(1):8–12. doi:10.1038/kisup.2012.7
- Vincent JL, de Mendonça A, Cantraine F, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med. 1998;26(11):1793–1800. doi:10.1097/00003246-199811000-000169824069
- Sanz MA, Montesinos P. How we prevent and treat differentiation syndrome in patients with acute promyelocytic leukemia. Blood. 2014;123(18):2777–2782. doi:10.1182/blood-2013-10-51264024627526
- Luciano RL, Brewster UC. Kidney involvement in leukemia and lymphoma. Adv Chronic Kidney Dis. 2014;21(1):27–35. doi:10.1053/j.ackd.2013.07.00424359984
- Di Micco L, Mirenghi F, Morelli E, De Simone E. Acute kidney failure in differentiation syndrome: a possible complication during therapy with differentiating agents for acute promyelocytic leukemia. A case report. G Ital Nefrol. 2019;36(4).
- Seylanova N, Crichton S, Zhang J, Fisher R, Ostermann M. Acute kidney injury in critically ill cancer patients is associated with mortality: a retrospective analysis. PLoS One. 2020;15(5):e0232370. doi:10.1371/journal.pone.023237032437362
- Chamoun K, Kantarjian HM, Wang X, et al. Unrecognized fluid overload during induction therapy increases morbidity in patients with acute promyelocytic leukemia. Cancer. 2019;125(18):3219–3224. doi:10.1002/cncr.3219631150121
- Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guidelines by the infectious diseases society of america for the treatment of methicillin-resistant staphylococcus aureus infections in adults and children: executive summary. Clin Infect Dis. 2011;52(3):285–292. doi:10.1093/cid/cir03421217178
- Wilson FP, Berns JS. Tumor lysis syndrome: new challenges and recent advances. Adv Chronic Kidney Dis. 2014;21(1):18–26. doi:10.1053/j.ackd.2013.07.00124359983
- Filippone EJ, Kraft WK, Farber JL. The nephrotoxicity of vancomycin. Clin Pharmacol Ther. 2017;102(3):459–469. doi:10.1002/cpt.72628474732
- Okada N, Chuma M, Azuma M, et al. Effect of serum concentration and concomitant drugs on vancomycin-induced acute kidney injury in haematologic patients: a single-centre retrospective study. Eur J Clin Pharmacol. 2019;75(12):1695–1704. doi:10.1007/s00228-019-02756-431511938
- Suzuki Y, Tokimatsu I, Morinaga Y, et al. A retrospective analysis to estimate target trough concentration of vancomycin for febrile neutropenia in patients with hematological malignancy. Clin Chim Acta. 2015;440:183–187. doi:10.1016/j.cca.2014.11.02725476135
- Chastain DB, Wheeler S, Franco-Paredes C, Olubajo B, Hawkins WA. Evaluating guideline adherence regarding empirical vancomycin use in patients with neutropenic fever. Clin Infect Dis. 2018;69:88–93.
- Melling PA, Noto MJ, Rice TW, Semler MW, Stollings JL. Time to first culture positivity among critically ill adults with methicillin-resistant staphylococcus aureus growth in respiratory or blood cultures. Ann Pharmacother. 2020;54(2):131–137. doi:10.1177/106002801987793731544471
- Sinha Ray A, Haikal A, Hammoud KA, Yu AS. Vancomycin and the risk of AKI: a systematic review and meta-analysis. Clin J Am Soc Nephrol. 2016;11(12):2132–2140. doi:10.2215/CJN.0592061627895134
- Park JH, Qiao B, Panageas KS, et al. Early death rate in acute promyelocytic leukemia remains high despite all-trans retinoic acid. Blood. 2011;118(5):1248–1254. doi:10.1182/blood-2011-04-34643721653939