 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
Black cumin (Nigella sativa) is an ancient herbal medicine recommended by the World Health Organization. The antioxidant and antihyperglycemic effects of black cumin are well established. Amelioration of renal dysfunction in nephrotoxic rats with black cumin treatment has also been noted. However, the effect of black cumin treatment on renal dysfunction in diabetes mellitus has not been clarified. In this study, the effect of black cumin oil (BC) on changes in renal dysfunction and renal hemodynamics in streptozotocin-induced diabetic rats was evaluated.
Methods
The experiments were performed in male Sprague Dawley rats, divided into four groups (seven in each group): (1) normal rats given tap water (CON); (2) normal rats administered with BC (CON-BC); (3) diabetic rats given tap water only (STZ); and (4) diabetic rats administered with BC (STZ-BC). Diabetes mellitus was induced in the rats by an injection of streptozotocin. BC was given orally at the dose of 1000 mg/kg body weight to the rat in either CON-BC or STZ-BC every day for 8 weeks. Renal hemodynamics and functions in each rat were studied.
Results
Renal hemodynamic changes in STZ-BC rats appeared to increase in terms of glomerular filtration rate, effective renal plasma flow, and effective renal blood flow, while renal vascular resistance and filtration fraction were decreased in comparison with diabetic rats given tap water only (STZ). An improvement of renal tubular dysfunction in STZ-BC rats was indicated by the decreases in fractional excretion of water and Mg++.
Conclusion
An administration of BC can restore changes in renal hemodynamics and renal dysfunction in streptozotocin-induced diabetic rats.
Introduction
Black cumin or black seed (Nigella sativa) is the ancient traditional herbal medicine that has been used continuously in the Middle East and is well-known throughout the rest of the world.Citation1–Citation4 The World Health Organization recommends black cumin as a herbal medicineCitation5 with anxiolytic effectCitation6 and it is used as an essential ingredient in Eastern medicine, including in Thai traditional medicine and Indian ayurvedic medicine. The active constituents of black cumin have been identified as thymoquinone, dithymoquinone, thymohydroquinone, and thymol.Citation7 Several studies have shown the various therapeutic actions of black cumin. It has activity against diabetes,Citation8,Citation9 radical scavenging activity,Citation10,Citation11 prevents lipid peroxidation,Citation12 and increases the antioxidant defense system.Citation12
Renal dysfunction is a common complication in diabetes mellitus that is involved in oxidative stress changes.Citation13–Citation15 The amelioration of renal hemodynamic and function changes in diabetics has been elucidated by supplementation with antioxidants.Citation16–Citation18 Black cumin was believed to be responsible for restoration in renal dysfunction in nephrotoxic rats through the antioxidant effect.Citation19,Citation20 However, knowledge of the effect of black cumin administration on changes in renal functions is still limited, especially in diabetes mellitus. Therefore, in the present study, the effect of black cumin oil (BC) on changes in renal dysfunction and renal hemodynamics was evaluated when administered in streptozotocin-induced diabetic rats.
Material and methods
Animals, experimental design, and treatments
All animals were cared for in accordance with recommendations given by the Ethics Committee of the Chulalongkorn University Animal Care and Use Committee. These guidelines were formulated to comply with international standards and are in accordance with the principles and guidelines for animal care of the National Council of Thailand (1999).
Twenty-eight male Sprague Dawley rats weighing 180–200 g were used in this study. The rats were divided into four groups of seven rats each: (1) control rats given tap water (CON); (2) control rats administered with black cumin oil (CON-BC); (3) diabetic rats given tap water only (STZ); and (4) diabetic rats administered with BC (STZ-BC). Diabetes mellitus was induced in the rats by an intravenous injection of streptozotocin (Sigma Chemical Co, St Louis, MO) at a dose of 55 mg/kg via the tail vein while the control rat was injected with an equivalent volume of citrate buffer as vehicle.Citation21 Two days after the injections, the blood samples of all rats which had fasted for 9 hours were obtained from the tail vein to verify the hyperglycemic state (blood glucose concentration >200 mg/dL). Streptozotocin-treated rats that did not exhibit hyperglycemia within 48 hours were excluded from the study. BC derived from the Nigella sativa plant by cold-pressed extraction (Sungsomboon Co, Ltd, Lopburi, Thailand) was given orally at a dose of 1000 mg/kg body weight to rats in the CON-BC or STZ-BC groups every day for 8 weeks. All animals were fed with standard rat chow and given tap water ad libitum. At the end of the experimental period, blood samples were taken from the tail vein of rats that had fasted for 9 hours and were tested for blood glucose concentration.
Renal hemodynamics and glomerular function study
On the specified day at the end of the experiment, an animal in each group was anesthetized with pentobarbitone sodium (Nembutal; CEVA Santé Animal, Libourne, France) (60 mg/kg body weight intraperitoneally). A tracheostomy was performed to facilitate respiration. The right common carotid artery was catheterized for collecting blood samples and monitoring blood pressure and heart rate (McLab System; ADInstruments, Sydney, Australia). The femoral vein was also catheterized for infusion of mixture solution of inulin and para-aminohippuric acid (PAH).
The urinary bladder was exposed by an incision at linea alba to canulate for urine collection. The animal was sustained with an infusion of normal saline solution at the rate of 10 mL/kg/h during the operation. After the operation, the mixture solution of inulin and PAH was infused instead of normal saline solution alone throughout the experiment. Two consecutive urine samples and blood samples at the midpoint of each urine collection were collected to study the glomerular filtration rate (GFR) and effective renal plasma flow (ERPF) by renal clearances of inulin (Cin) and PAH (CPAH) using standard techniques.Citation22 The blood volume was sustained by 6% bovine serum albumin in normal saline solution. Blood pressure and heart rate were recorded throughout the period of study. Hematocrit values of the blood samples were determined using a microhematocrit centrifuge (Z230H; BHG HERMLE GmbH and Co, Gosheim, Germany) and a microcapillary reader (IEC CAT No. 2201, Damon/IEC Division, Houston, TX). At the end of the experiment, both kidneys were immediately excised, the adhering fat removed, and weighed. The parameters of renal hemodynamics and glomerular function were calculated using the equations as follows:
(1)
(2)
(3)
(4)
(5) where, GFR = glomerular filtration rate (mL/min/g kidney weight), Cin = clearance of inulin (mL/min), Uin = urinary inulin concentration (mg/mL), V = urine flow rate (mL/min), Pin = plasma inulin concentration (mg/mL), ERPF = effective renal plasma flow (mL/min/g kidney weight), CPAH = clearance of PAH (mL/min), UPAH = urinary PAH concentration (mg/mL), PPAH = plasma PAH concentration (mg/mL), ERBF = effective renal blood flow (mL/min/g kidney weight), Hct = hematocrit value (%), FF = filtration fraction (%), RVR = renal vascular resistance (mmHg/mL/min/g kidney weight), and MAP = mean arterial pressure (mmHg).
Renal tubular function study
Fractional excretions (FE) of sodium (FENa), potassium (FEK), chloride (FECl), and magnesium (FEMg) ions,Citation23,Citation24 and of water () were performed to study the renal tubular function using the equations as follows:
(6)
(7) where,
, GFR = glomerular filtration rate (mL/min/g kidney weight), V = urine flow rate (mL/min), FEE = fractional excretion of the electrolytes (%), UE = concentration of urinary electrolytes (mEq/L), and PE = concentration of plasma electrolytes (mEq/L).
Chemical analyses
The urine and plasma samples were analyzed for inulin concentration by color developing using the diphenylamine methodCitation25 and PAH using the Smith method.Citation22 Plasma and urinary sodium-, potassium-, and chloride-ion concentration were determined using ion-selective electrode potentiometry (Cobas Integra 400 Plus; Roche Diagnostics Ltd, Rotkreuz, Switzerland). Magnesium concentrations in plasma and urine were measured using an atomic absorption spectrophotometer (1100B; PerkinElmer, Inc, Waltham, MA). The blood glucose concentration was determined using a glucometer (Advance Glucometer; Boehringer Ingelheim Pharma GmbH and Co, KG, Mannheim, Germany).
Statistical analyses
The data were statistically analyzed by analysis of variance (ANOVA) using Duncan’s test as the post hoc test. The significant comparisons were considered at P-values <0.05. The results are presented as means ± standard deviation.
Results
Blood glucose concentration, blood pressure, and heart rate
The data in show that blood glucose levels significantly increased about 5–6 fold in the diabetic rats (STZ) and diabetic rats treated with BC (STZ-BC) in comparison with those in rats in the CON and CON-BC groups (P < 0.001). The blood glucose concentration of STZ-BC rats slightly decreased (4%) as compared with STZ rats. The heart rates significantly decreased (15%) in untreated diabetic rats, while the blood pressures showed nonsignificant decrease as compared with those of CON rats. The systemic circulatory parameters were maintained at the control levels in STZ-BC rats and systolic pressure and heart rate were significantly increased in comparison with those in STZ rats (P < 0.05).
Table 1 Alterations of blood glucose concentration and systemic circulation of control rats and diabetic rats after black cumin (Nigella sativa) oil administration (n = 7 in each group)
Renal hemodynamics and glomerular function
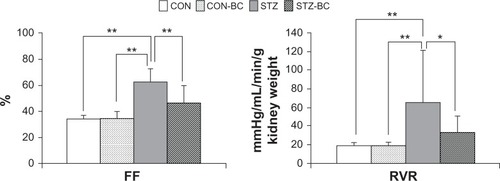
shows significant decreases (P < 0.01) in GFR (37%), ERPF (66%), and ERBF (65%) in diabetic rats as compared with those of rats in CON and CON-BC. After administration of BC for 8 weeks to diabetic rats, there were significant increases (P < 0.01) in GFR (51%), ERPF (92%), and ERBF (98%) as compared with the results obtained in untreated STZ rats; these values did not differ from those recorded in the CON rats. Increases in RVR (P < 0.05) of nearly 2.5 fold and FF of 83% (P < 0.01) were apparent in STZ rats as compared with those of both CON and CON-BC rats (). Administration of BC to diabetic rats could decrease RVR 50% (P < 0.05) and FF 25% (P < 0.01) compared with the results obtained in untreated diabetic rats, while they were not significantly different from the CON and CON-BC rats.
Figure 1 Effects of black cumin (Nigella sativa) oil administration on glomerular filtration rate (GFR), effective renal plasma flow (ERPF), and effective renal blood flow (ERBF).
Abbreviations: CON, control rats; CON-BC, control rats administered with black cumin oil; STZ, diabetic rats not administered with black cumin oil; STZ-BC, diabetic rats administered with black cumin oil.
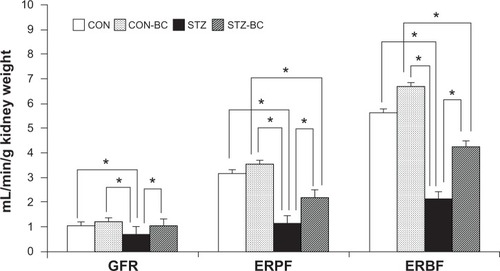
Figure 2 Effects of black cumin (Nigella sativa) oil administration on filtration fraction (FF) and renal vascular resistance (RVR).
Abbreviations: CON, control rats; CON-BC, control rats administered with black cumin oil; STZ, diabetic rats not administered with black cumin oil; STZ-BC, diabetic rats administered with black cumin oil.
Renal tubular function
Fractional excretion of water () and fractional excretion of Mg++ (FEMg) of untreated diabetic rats significantly increased (P < 0.05) to approximately 120% and 106%, respectively, compared with those of CON rats and CON-BC rats (). After BC administration in STZ-BC rats, the values of
and FEMg were significantly reversed (P < 0.05) to near the control levels, which were lower than those of STZ rats at approximately 47% and 32% (P < 0.05), respectively. FENa and FECl seemed to be decreased but not significant in both untreated diabetic rats and treated rats in comparison with those of rats in both CON and CON-BC. The FEK values in STZ and STZ-BC rats significantly decreased (P < 0.05) in comparison with those of CON and CON-BC rats. There was no significant difference for values of FENa, FECl, and FEK between STZ and STZ-BC rats.
Table 2 Alterations in renal tubular function of control rats and diabetic rats after black cumin (Nigella sativa) oil administration (n = 7 in each group)
Discussion
The results obtained in the present study for the effect of BC administration on renal function and renal hemodynamics in diabetic rats showed that BC can ameliorate renal dysfunction in kidney disease in a similar way to that observed in the administration of BC to nephrotoxic rats.Citation19,Citation20 Profound glomerular dysfunction was apparent in the diabetic rats with a significant reduction of GFR and a marked increase in RVR, which agreed with the authors’ previous studies.Citation17,Citation21 During progression of diabetes, a gradual increase in angiotensin-converting enzyme (ACE) was believed to be responsible for an increase in RVR.Citation26 An elevation of ACE level contributes to an increase in angiotensin II resulting in vasoconstriction, which preferentially constricts renal efferent arterioles rather than afferent arterioles.Citation27 The continuous vasoconstriction of renal arterioles leads to decreased GFR in diabetes. Inhibition of the renin-angiotensin system by ACE inhibitors has been reported to improve kidney function and these are commonly used in diabetics.Citation28–Citation32 The present results showed that BC administration in diabetic rats could decrease renal vascular resistance resulting in increases in effective renal plasma flow and renal blood flow near to values recorded in control rats, with consequent restoration of GFR level (, ). In addition, BC administration in STZ-BC rats could lower the filtration fraction to near the control level. The high filtration fraction, which indicates an improper ratio of GFR to ERPF, was apparent in the untreated diabetic rats.Citation33 The extent of ERPF reduction was more than that of GFR in STZ rats. In treated diabetic rats, the degree of increase in ERPF was more than that of GFR. Given these findings, it is probable that the dilatation of efferent arterioles would be more than that of the afferent arterioles during BC administration in diabetic rats. The present findings for the action of BC seem consistent with the action of ACE inhibitors,Citation33 although neither the plasma angiotensin level, the dilatation, nor the constriction of efferent and afferent arterioles were measured directly in the present study. The ACE inhibitor-like effect of BC may occur not only in diabetic rats but also in control rats. Physiologically, local production of angiotensin II is not high. Additionally, the kidney can regulate both GFR and renal blood flow via process of autoregulation. Therefore, in the present study, the remarkable changes of both GFR and ERPF were less pronounced in CON-BC rats in comparison with the untreated control rats. The responsive effect of BC administration on kidney function via inhibition of the renin-angiotensin system needs to be investigated further.
The present study shows that STZ rats in the absence of BC administration had a lower heart rate in comparison with the normal control level (). After BC administration every day for 8 weeks in diabetic rats, significant elevation of both heart rate and blood pressure was observed. The relationship between general circulation and renal hemodynamics is recognized. An increase in systemic blood pressure would contribute to an increase in ERPF, which would partly account for the increase in filtration pressure and GFR in STZ-BC rats. However, small alteration of the heart rate with significant increase in systolic blood pressure is, at least in part, affected by the role of BC in CON-BC rats. These results are in agreement with the previous study of cardiac inotropic and chronotropic adrenergic responsiveness of N. sativa–supplemented rats,Citation34 but in contrast to other previous studies of the antihypertensive effect of BC.Citation35–Citation37 The discrepancy in results for BC administration in hypertension between those studies and the present study could reflect the differences in species studied, including the model used in the studies. The explanation for this interesting finding deserves further investigation.
It is known that in general physiological condition FENa is usually <1% during the reduction of renal hemodynamics. This was true in the diabetic rats in this study, in which RVR increased and GFR and RBF decreased. FENa and FECl seemed to decrease but not significantly in both untreated and treated diabetic rats in comparison with those of rats in both CON and CON-BC groups. These results indicate no tubular defect in Na+ reabsorption. However, hemodynamic changes and no alteration of FENa in comparable tubular dysfunction in diabetes seem unlikely. An increase in fractional excretion of Mg++ has been demonstrated to be an indicator for impairment of renal tubular reabsorption.Citation23,Citation24 FEMg in the diabetic rats was higher (106%) than that of CON rats. After BC administration, FEMg of STZ-BC markedly decreased toward the control level (). The constriction of efferent arterioles with an increase in RVR in diabetic rats would account for the decrease in peritubular blood flow, leading to decreased tubular Mg++ reabsorption. Alternatively, the dilatation of efferent arterioles during administration of BC in diabetic rats would increase peritubular blood flow and Mg++ reabsorption resulting in a decrease in FEMg. Furthermore, increase in renal tubular reabsorption of water was apparent in STZ-BC rats. Diuresis usually occurs in diabetics in the absence of BC as a result of glycosuria and impairment of renal tubular function. It is probable that BC administration may ameliorate the impairment of renal tubular reabsorption, decrease glycosuria, or both. In the present study, BC administration did not decrease blood glucose concentration in STZ-BC rats as would be expected. This observation did not support other experimental studies of antihyperglycemic activities of BC administration.Citation38,Citation39 However, the slight decrease in blood glucose concentration in STZ-BC rats may contribute to the decrease in diuresis. In addition, the antioxidative stress activity of BC in the amelioration of renal dysfunction should not be ignored in the present experiment.Citation10–Citation12
In conclusion, BC administration in streptozotocin-induced diabetic rats achieved a better restoration of changes in renal hemodynamics and renal dysfunction including the enhancement of vascular function. These findings deserve further investigation in terms of the role of BC in the inhibition of the renin-angiotensin system.
Acknowledgments
This study was supported by the Thailand Research Fund. The authors are grateful to Dr Sirima Thongruay and Mr Theerasak Norapaksunthorn for their assistance.
Disclosure
The authors report no conflicts of interest in this work.
References
- ClearyPDChiropractic use: a test of several hypothesesAm J Public Health1982727277307091466
- CookCBaisdenDAncillary use of folk medicine by patients in primary care clinics in southwestern West VirginiaSouth Med J198679109811013749993
- McGuireMBRitual Healing in Suburban AmericaNew Brunswick, NJRutgers University Press1988
- HuntLMArarNHAkanaLLHerbs prayer, and insulin: use of medical and alternative treatments by a group of Mexican American diabetic patientsJ Fam Pract20004921622310735480
- World Health OrganizationNigella sativaIndex Medicus for the Eastern Mediterranean Region2009861Health Publications, Production & Dissemination, Library & Health Literature Services, WHO Region office for the Eastern Mediterranean Available from: http://www.emro.who.int/dsaf/dsa1032.pdfAccessed December 8, 2011
- PerveenTHaiderSKanwalSHaleemDJRepeated administration of Nigella sativa decreases 5-HT turnover and produces anxiolytic effects in ratsPak J Pharm Sci20092213914419339222
- GhoshehOAHoudiAACrooksPAHigh performance liquid chromatographic analysis of the pharmacologically active quinones and related compounds in the oil of the black seed (Nigella sativa L.)J Pharm Biomed Anal19991975776210698539
- El-DakhakhnyMMadyNLembertNAmmonHPThe hypoglycemic effect of Nigella sativa oil is mediated by extrapancreatic actionsPlanta Med20026846546612058330
- KanterMCoskunOKorkmazAOterSEffects of Nigella sativa on oxidative stress and beta-cell damage in streptozotocin-induced diabetic ratsAnat Rec A Discov Mol Cell Evol Biol200427968569115224410
- BuritsMBucarFAntioxidant activity of Nigella sativa essential oilPhytother Res20001432332810925395
- RamadanMFKrohLWMörselJTRadical scavenging activity of black seed (Nigella sativa L.), coriander (Coriandrum sativum L.), and niger (Guizotia abyssinica Cass.) crude seed oils and oil fractionsJ Agric Food Chem2003516961696914611155
- MeralIYenerZKahramanTMertNEffect of Nigella sativa on glucose concentration, lipid peroxidation, anti-oxidant defence system and liver damage in experimentally-induced diabetic rabbitsJ Vet Med A Physiol Pathol Clin Med20014859359911848252
- BaynesJWRole of oxidative stress in development of complications in diabetesDiabetes1991404054122010041
- HeidlandASebekovaKSchinzelRAdvanced glycation end products and the progressive course of renal diseaseAm J Kidney Dis200138S100S10611576932
- LeeHBYuMRYangYJiangZHaHReactive oxygen species-regulated signaling pathways in diabetic nephropathyJ Am Soc Nephrol2003148 Suppl 3S241S24512874439
- CravenPADe RubertisFRKaganVEMelhemMStuderRKEffects of supplementation with vitamin C or E on albuminuria, glomerular TGF-beta, and glomerular size in diabetesJ Am Soc Nephrol19978140514149294832
- YusuksawadMSChaiyabutrNChanges in renal hemodynamics in streptozotocin-induced diabetic rats with L-ascorbic acid supplementationClin Hemorheol Microcirc20063439139916614463
- KuhadASachdevaAKChopraKAttenuation of renoinflammatory cascade in experimental model of diabetic nephropathy by sesamolJ Agric Food Chem2009576123612819601660
- AliBHThe effect of Nigella sativa oil on gentamicin nephrotoxicity in ratsAm J Chin Med200432495515154284
- UzEBayrakOKayaANigella sativa oil for prevention of chronic cyclosporine nephrotoxicity: an experimental modelAm J Nephrol20082851752218223305
- YusuksawadMThongruaySLe GrandSMChaiyabutrNLong-term effects of vitamin C supplementation on glomerular changes in streptozotocin-induced diabetic ratsAsian Biomed20071279287
- SmithHWPrinciple of Renal PhysiologyNew York, NYOxford University Press1962196217
- FutrakulNButthepPVongthavarawatVEarly detection of endothelial injury and dysfunction in conjunction with correction of hemodynamic maladjustment can effectively restore renal function in type 2 diabetic nephropathyClin Hemorheol Microcirc20063437338116614461
- FutrakulNFutrakulPRenal microvascular disease in an aging population: a reversible process?Ren Fail20083035335618569906
- LittleJMA modified diphenylamine procedure for the determination of inulinJ Biol Chem194918074775418135809
- LeeheyDJSinghAKAlaviNSinghRRole of angiotensin II in diabetic nephropathyKidney Int200058Suppl 77S93S98
- ArimaSItoSThe mechanisms underlying altered vascular resistance of glomerular afferent and efferent arterioles in diabetic nephropathyNephrol Dial Transplant2003181966196913679465
- ErmanAVekslerSGafterUBonerGWittenbergCvan DijkDJRenin-angiotensin system blockade prevents the increase in plasma transforming growth factor β1, and reduces proteinuria and kidney hypertrophy in the streptozotocin-diabetic ratJ Renin Angiotensin Aldosterone Syst2004514615115526251
- AndersenSTarnowLRossingPHansenBVParvingHHRenoprotective effects of angiotensin II receptor blockade in type 1 diabetic patients with diabetic nephropathyKidney Int20005760160610652037
- HitePFDeBellisHFDiabetic kidney disease: a renin-angiotensin-aldosterone system focused reviewJ Pharm Pract200922560570
- HeerspinkLNinomiyaTNinomiyaTEffects of a fixed combination of perindopril and indapamide in patients with type 2 diabetes and chronic kidney diseaseEur Heart J2010312888289620501479
- ZojaCCornaDGagliardiniEAdding a statin to a combination of ACE inhibitor and ARB normalizes proteinuria in experimental diabetes, which translates into full renoprotectionAm J Physiol Renal Physiol2010299F1203F121120719975
- MillerJAImpact of hyperglycemia on the renin angiotensin system in early human type 1 diabetes mellitusJ Am Soc Nephrol1999101778178510446946
- Al-HaririMTYarTBamosaAOEl-BahaiMNEffects of two-months Nigella sativa supplementation on cardiac hemodynamics and adrenergic responsivenessJ Pak Med Assoc20095936336819534369
- BoskabadyMHShafeiMNParsaeeHEffects of aqueous and macerated extracts from Nigella sativa on guinea pig isolated heart activityPharmazie20056094394816398273
- KhattabMMNagiMNThymoquinone supplementation attenuates hypertension and renal damage in nitric oxide deficient hypertensive ratsPhytother Res20072141041417236176
- DehkordiFRKamkhahAFAntihypertensive effect of Nigella sativa seed extract in patients with mild hypertensionFund Clin Pharmacol200822447452
- RchidHChevassusHNmilaRNigella sativa seed extracts enhance glucose-induced insulin release from rat-isolated Langerhans isletsFundam Clin Pharmacol20041852552915482373
- FararhKMAtojiYShimizuYShiinaTNikamiHTakewakiTMechanisms of the hypoglycaemic and immunopotentiating effects of Nigella sativa L. oil in streptozotocin-induced diabetic hamstersRes Vet Sci20047712312915196902