Abstract
Osteoporosis represents a weakening of bone tissue due to an imbalance in the dynamic processes of bone formation and bone resorption that are continually ongoing within bone tissue. Most currently available osteoporosis therapies are antiresorptive agents. Over the past decade, bisphosphonates, notably alendronate and risedronate, have become the dominant agents with newer bisphosphonates such as ibandronate and zoledronic acid following a trend of less frequent dosing regimens. Synthetic estrogen receptor modulators (SERMs) continue to be developed as drugs that maintain the bone-protective effects of estrogen while avoiding its associated adverse side effects. Currently available agents of this class include raloxifene, the only SERM available in the United States (US), and lasofoxifene and bazedoxifene, available in Europe. Calcitonin, usually administered as a nasal spray, completes the list of currently approved antiresorptive agents, while parathyroid hormone analogs represent the only anabolic agents currently approved in both the US and Europe. Strontium ranelate is an additional agent available in Europe but not the US that has both anabolic and antiresorptive activity. New agents expected to further expand therapeutic options include denosumab, a monoclonal antibody inhibitor of the resorptive enzyme cathepsin K, which is in the final stages of Food and Drug Administration approval. Other agents in preclinical development include those targeting specific molecules of the Wnt/β-catenin pathway involved in stimulating bone formation by osteoblast cells. This review discusses the use of currently available agents as well as highlighting emerging agents expected to bring significant changes to the approach to osteoporosis therapy in the near future.
Introduction
Bone is a dynamic tissue, undergoing a continual remodeling process involving a cycle of formation of new bone tissue and breakdown (resorption) of older bone tissue. In osteoporosis, the balance of these processes is tipped toward resorption, leading to weakening of bone tissue and increased risk of fracture. Pharmacotherapy for the prevention and treatment of osteoporosis has predominantly been based on agents that prevent resorption of bone. Most available agents are effective at increasing bone mineral density or preventing fractures of the vertebra. The majority also have effects on nonvertebral sites, including the hip.
Over the past decade, bisphosphonates have become the most commonly prescribed osteoporosis medication following the decline of the use of estrogen-based hormone therapy as a result of the United States (US) Women’s Health Initiative trial. Focus in hormone therapy has shifted to synthetic estrogen receptor modulators (SERMs) designed to retain the positive effects of estrogen on bone while minimizing the negative effects of increasing risk of cardiovascular disease and cancer. Calcitonin hormone (another antiresorptive agent), parathyroid hormone (PTH) analogs (to date the only anabolic agent for osteoporosis treatment available in the US), and strontium ranelate (an agent with both anabolic and antiresorptive activity used widely in Europe, but not the US) complete the list of currently available treatment options.
New treatments in clinical trials include both new generations of currently available therapies and agents with novel mechanisms of action. New therapeutic strategies are also emerging from recent discoveries regarding the role of biologic pathways such as the Wnt/β-catenin pathway in regulating bone cell function. These strategies include more agents targeted to promote bone growth with the potential to be more effective in preventing fractures than current approaches.
Disease prevalence and treatment guidelines
Osteoporosis represents a condition of compromised bone strength predisposing a person to an increased risk of fracture. Bone strength depends on both bone quality and bone density. While bone density is relatively easily measured, by dual x-ray absorptiometry (DXA) and other modalities, there are few good measures of bone quality. Bone mineral density (BMD) has thus become the most common clinical measure of osteoporosis, although its relationship to risk of fracture is not strictly proportional.Citation1,Citation2
The World Health Organization (WHO) has defined osteoporosis as a BMD measurement of 2.5 standard deviations or more below the population mean BMD of sex-matched young adults, ie, a T-score of ≤ −2.5.Citation3 BMD is typically measured at the lumbar spine, femoral neck, and hip. A T-score of < −2.5 at any of those sites is diagnostic for osteoporosis. Osteopenia, or low bone mass, is defined as 1.5 to 2.5 standard deviations below the population mean. The occurrence of a nontraumatic fracture, regardless of BMD, is also considered by definition to be osteoporosis.
According to statistics compiled by the International Osteoporosis Foundation, more than 75 million people in the United States, Europe, and Japan have osteoporosis with an additional 70 million persons likely affected in China.Citation4 The US National Osteoporosis Foundation (NOF) has estimated that 10 million people have osteoporosis in the US alone with another 34 million having osteopenia.Citation5 As a result, lifetime risk of fracture for whites over the age of 50 years in the US is estimated to be 53% for females and 21% for males.Citation5 Fractures are costly to the individual in terms of morbidity – leading to chronic pain, disability, and loss of independence – and increased mortality. Costs to society are also high; according to NOF, two million osteoporotic fractures occur in the US per year, costing $19 billion/year in treatment costs.Citation5 By the year 2015, these numbers are expected to increase to three million fractures at a cost of more than $25 billion/year. Nine million osteoporotic fractures are estimated to occur annually worldwide.Citation4
An international consensus regarding who to screen and treat does not currently exist.Citation6 In the US, BMD screening is recommended by most organizations for all women aged 65 years and older, all men aged 70 years and older, and women and men aged 50 to 70 at high risk for the disease.Citation7 Risk calculators, such as WHO’s online FRAX® calculators (World Health Organization Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, UK) can determine an individual’s specific risk of fracture over the next 10 years based on country of residence and by inputting femoral neck BMD along with age, sex, height, weight, history of personal or parental fracture, smoking and drinking status, history of rheumatoid arthritis, use of glucocorticoids, or secondary osteoporosis.Citation8
Guidelines from NOF and other organizations in the US call for initiation of treatment in the following patients:Citation9
Patients with hip or vertebral fractures
Patients with BMD T-scores ≤ −2.5 at the femoral neck, total hip, or spine by DXA
Postmenopausal women or men ≥50 years old with low bone mass (T-score between −1 and −2.5) at the femoral neck, total hip, or spine AND:
10 year hip fracture probability ≥3% OR
10 year all major osteoporosis-related fracture probability of ≥20% based on the US-adapted WHO absolute fracture risk model
Osteoporosis is largely under-treated. In one study in the US, it was shown that only 26% of white women at high risk for fracture were receiving osteoporosis therapy, with the rate being less than 3% among men and black women with the same risk.Citation1 Low rates of adherence to osteoporosis medications contribute to under-treatment of the disease, with most studies estimating that 50% or less of patients with a prescription for osteoporosis medication actually take the medication as prescribed, regardless of the type of medication or frequency of dosing.Citation10 Improved adherence thus continues to be a goal in osteoporosis therapy.
Bone biology
Pharmacologic therapies for osteoporosis have been targeted to a number of different molecular processes involved in the bone remodeling cycle. Bone tissue is specialized connective tissue composed of cells, organic bone matrix, and inorganic calcified crystals. In addition to its mechanical function, bone plays a role in metabolic functions, such as serving as the primary storage site for calcium, phosphate, and other minerals. Thus, bone remodeling is not only altered by mechanical stresses, but also responds to a number of systemic hormones that regulate calcium homeostasis.
There are three primary cell types in bone, two of which, osteoblasts and osteoclasts, are located at the surface of the bone matrix. Osteocytes, which are derived from osteoblasts, are embedded in the bone matrix (). During the continual bone remodeling cycle, osteoclasts demineralize and resorb old bone, and osteoblasts deposit new bone to maintain a bone mass that adequately responds to the stresses placed on the skeleton.
Figure 1 RANK/RANKL/Osteoprotegerin signaling system in bone. Osteoblasts express the membrane-bound signaling protein receptor activator of NF kappa B ligand (RANKL) that binds to its receptor (RANK) on osteoclast precursor cells to stimulate their differentiation into activated multinucleated osteoclasts. Osteoprotegerin (OPG) secreted by local cells including osteoblasts also binds RANK and inhibits this activation. Activated osteoclasts secrete proteinases, including the collagenase cathepsin K that degrades collagen 1 fibers, the major organic component of bone matrix. The osteoclasts also secrete hydrochloric acid that dissolves the calcium phosphate hydroxyappatite crystals of the matrix.
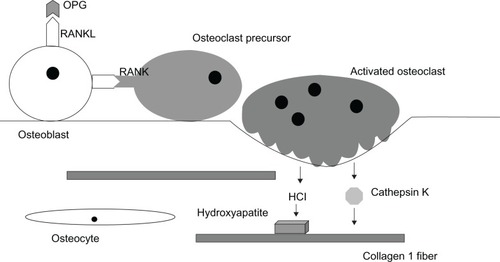
Osteoblasts actively produce osteoid, the organic component of the bone matrix, composed mainly of Type I collagen fibers along with a mixture of proteoglycans, phosphoproteins, phospholipids, hyaluronic acid, and glycoproteins ().Citation11,Citation12 Two of these glycoproteins, osteocalcin and sialoprotein, are bone-specific and have a high affinity for calcium. The inorganic component of the bone matrix is made up of calcium and phosphorus deposited along the osteoid scaffolding primarily in the form of hydroxyapatite crystals. Osteoclasts resorb the matrix by secreting hydrochloric acid, which dissolves calcium phosphate, and enzymes such as collagenases and other proteases. The most important of the proteases is cathepsin K, which degrades the organic matrix including Type I collagen.Citation11
Normally the processes of bone formation and bone resorption are tightly balanced. Disturbance of this balance can compromise bone density, strength, and microarchitecture. Most often this occurs due to increased osteoclast activity, leading to increased bone resorption and diminished bone density. In post-menopausal women, increased osteoclast activity results from the loss of estrogen; with the largest decrease in BMD occurring within five years of the beginning of menopause.Citation13
Systemic calcium homeostasis is under the control of three hormones with direct effects on bone tissue: vitamin D, calcitonin, and PTH. Activated vitamin D3 stimulates intestinal absorption of calcium. In bone, vitamin D3 binds to receptors on osteoblasts to increase release of osteocalcin and another glycoprotein, osteopontin, to facilitate mineralization.Citation14 PTH is released from the parathyroid glands in response to low calcium. Continuous high PTH levels act to mobilize calcium and phosphorus by stimulating resorption by osteoclasts.Citation15 High serum calcium feeds back to inhibit PTH release. Calcitonin is released from the thyroid gland in response to high serum calcium levels. It binds to receptors on osteoclasts and directly inhibits their activity, leading to reduced resorption and lower calcium levels.Citation15
Estrogen is another systemic hormone with direct effects on bone and playing an important role in osteoporosis. Recently it has been shown that estrogen acts through the estrogen receptor α (ERα) on osteoclasts to facilitate the expression of the FasL gene and induce apoptosis of osteoclasts, thereby controlling their lifespan.Citation16,Citation17
Within bone tissue, resorption is controlled by a system of three key proteins: RANK (receptor activator of nuclear factor kappa beta), its ligand RANKL (receptor-activator of nuclear factor kappa beta ligand), and a decoy receptor OPG (osteoprotegerin) ().Citation18 Binding of RANKL, a membrane-bound protein produced by osteoblasts, to RANK, the receptor on osteoclasts, leads to increased osteoclast differentiation, activation, and survival, resulting in increased bone resorption. OPG acts as a decoy receptor by binding with high affinity to RANKL therefore preventing the interaction with RANK. OPG thus acts as an effective inhibitor of bone resorption.
Many of the products of these processes can be measured as biochemical markers of bone turnover. Markers in current clinical use include, but are not limited to, degradation products of collagen I breakdown: telopeptides of the N-terminal (urinary NTx) and C-terminal (serum CTx) of collagen type 1; early markers of bone formation: N-terminal, propeptide of type 1 collagen and bone-specific alkaline phosphatase; and osteocalcin, a late marker of bone formation that appears only in the mineralization phase.Citation19 Cathepsin K is also considered a marker of bone turnover.
In contrast to imaging techniques, biochemical markers of bone turnover obtained in serum samples show changes in a markedly larger range. Typically a decrease of 50%–80% or an increase of 100%–200% occurs in days or weeks of initiating treatment with antiresorptive or anabolic drugs compared with usual increases in BMD of 6%–7% with bisphosphonates and 2%–3% with SERMs after two years of therapy.Citation19
Current pharmacologic treatments
Pharmacologic therapies for osteoporosis are all recommended in the context of standard nonpharmacologic therapy including adequate calcium, vitamin D, and weight-bearing exercise. Calcium supplements are recommended for adults at doses of 1,000 mg daily until age 50 and 1,200 mg/day for adults over age 50 years.Citation20 Concurrent vitamin D supplementation to ensure adequate calcium absorption is also recommended at doses of 800–1,000 international units (IU)/day for adults ages 50 and older, with the goal of achieving serum levels of at least 30 ng/mL. Assessment of vitamin D status is important, given that an estimated 77% of adults in the US are considered to have inadequate levels of vitamin D, ie, below 30 ng/mL.Citation21 Sunlight exposure is important in maintaining adequate levels of vitamin D, causing production of the vitamin D3 prohormone through ultraviolet B irradiation of its 7-dehydrocholesterol precursor in the skin.Citation22 However, even in latitudes where the sunlight intensity can facilitate this reaction year-round, insufficient levels of vitamin D are common in the population.Citation23 Although no formal recommendations for amounts of sun exposure exist, research referenced by the US National Institutes of Health has suggested that 5–30 minutes of exposure between 10 am and 3 pm at least two times a week without sunscreen may be adequate to maintain vitamin D levels.Citation24 For patients who are vitamin D-deficient, replacement levels of oral vitamin D of 50,000 IU/week should be taken for 8–12 weeks and then at least 1,000 IU/day.Citation25
Exercise, including weight-bearing activities such as running, jumping, and resistance training, can also contribute to osteoporosis prevention. Specific recommendations for maintenance of bone health from organizations such as the US NOF and the American College of Sports Medicine include performance of weight-bearing exercise for a total of 30 minutes on most days and resistance training of 8–12 repetitions or 8–10 exercises at least two days a week.Citation26,Citation27 Common-sense fall prevention strategies also contribute to fracture prevention.
An osteoporosis medication may have an indication for prevention of osteoporosis in patients with low bone mass, treatment of patients with already established osteoporosis, or both (). To be approved for prevention of osteoporosis in patients in the US, agents must be shown in clinical trials to significantly increase BMD in patients with low bone mass. Therapies approved for treatment of already established osteoporosis must demonstrate a significant reduction in fractures.
Table 1 Osteoporosis therapies currently approved in the US
Most currently approved drugs for osteoporosis prevention or treatment are antiresorptive (). The bisphosphonates, alendronate and risedronate, are often the first drugs recommended for treating postmenopausal osteoporosis. Bisphosphonates are approved for both prevention and treatment. Indications for estrogen are limited to prevention, whereas the calcitonin and PTH analogs are reserved for treatment. PTH is the single anabolic agent currently available in the US. Its use is limited to treatment of osteoporosis for two-year periods.
The focus of the therapies presented here is the treatment and prevention of primary osteoporosis associated with menopause and aging. However, it should be noted that a number of other diseases, as well as drugs and nutritional deficiencies, can cause secondary osteoporosis, the most frequent being glucocorticoid excess. Other conditions associated with secondary osteoporosis include endocrine disorders such as Cushing’s syndrome, hypogonadism, and Type 1 diabetes mellitus; gastrointestinal disease including celiac disease and other malabsorption syndromes, and liver disorders; bone marrow-related conditions such as thalassemia and other anemias; and other miscellaneous causes including chronic obstructive pulmonary disease, multiple sclerosis, and rheumatoid arthritis. Among the numerous medications associated with osteoporosis are heparin, anticonvulsants such as phenytoin and phenobarbitol, lithium, cancer chemotherapeutic agents, and excessive thyroid hormone.Citation28 Although patients with secondary osteoporosis can benefit from therapies used for primary osteoporosis, it is important to identify secondary osteoporosis because there are often effective specific interventions that can be added to the more general approach.
Antiresorptive agents
Bisphosphonates
Bisphosphonates are the most commonly prescribed drugs used to treat osteoporosis in the US and many other countries. Etidronate was the first bisphosphonate to be used as therapy beginning in the 1960s. Although its approved indications in the US are limited to treatment of hypercalcemia and Paget’s disease, a disease of accelerated bone turnover, etidronate is commonly used in Europe and other countries for treatment of osteoporosis as cyclic oral therapy, given for two weeks every three months.Citation29 Alendronate, a once daily oral medication, was the first bisphosphonate to be approved for treatment of osteoporosis in the US in 1995. Since that time, newer bisphosphonates with less frequent dosing intervals have been introduced, partially in an attempt to improve compliance. In addition to alendronate, three other bisphosphonates have been approved in the US for both treatment and prevention of osteoporosis. Risedronate is an oral medication that can be administered daily, weekly, or monthly at varying doses (). Zoledronic acid is medication administered once yearly by intravenous transfusion. Ibandronate is available in both oral and intravenous forms at various dosing frequencies.
Other bisphosphonates not approved in the US, but available in other countries for treatment of osteoporosis, include clodronate and pamidronate. Both are usually taken as oral agents, but are also available for intravenous, and in the case of clodronate, intramuscular administration.Citation30
Bisphosphonates are structurally related to inorganic pyrophosphate, a naturally occurring compound composed of two phosphate groups.Citation31 Like pyrophosphate, bisphosphonates bind to hydroxyapatite crystals and thus have a very high affinity for bone. Upon exposure to acid and enzymes secreted by an active osteoclast, bisphosphonates are released from the bone matrix where they promote osteoclast apoptosis.Citation31,Citation32
Bisphosphonates differ in strength of binding to the bone mineral matrix, with the zoledronic acid having the highest affinity followed by pamidronate > alendronate > ibandronate > risedronate > etidronate > clodronate.Citation31,Citation33 Higher-affinity bisphosphonates bind avidly to the bone surface, but spread through bone slowly. Lower-affinity agents are distributed more widely through the bone, but have a shorter residence time when treatment is stopped. Suppression of bone resorption occurs within approximately three months of initiation of oral bisphosphonate therapy regardless of dosing frequency, but is more rapid after intravenous administration. Length of suppression is largely a function of affinity for mineral matrix binding; zoledronic acid, with the highest affinity, effectively suppresses markers of bone turnover for up to one year.
Bisphosphonates in general have been shown to increase BMD of the spine by 5%–8% and at the hip by 3%–6% after three years. All bisphosphonates have been shown to reduce vertebral fractures by 40%–70%.Citation32 Aldenronate, risedronate, and zoledronic acid also reduced nonvertebral fractures by 25%–40%, including hip fractures by 40%–60%, in women with osteoporosis.Citation32 Ibandronate has not been shown to reduce nonvertebral fractures.
Divalent cations from food or other ingested sources will completely block absorption of oral bisphosphonates. Therefore, these agents must be taken after a prolonged fast, followed by 30–60 minutes with nothing else by mouth. Even under these conditions, less than 1% of an orally administered dose is absorbed. Bisphosphonates do not undergo systemic metabolism and their plasma half-lives are short. Fifty percent of the absorbed dose binds to bone surfaces; the other 50% is excreted rapidly by the kidneys.Citation32
Because bisphosphonates accumulate in bone, they can be continued to be released from bone for months or years after treatment is stopped and may protect against fracture for 3–5 years after treatment is stopped.Citation32 On this basis, consideration of a “drug holiday” after 5–10 years of bisphosphonate treatment has been advocated, with longer treatment periods and shorter off-treatment periods recommended for those at greatest risk of fracture.
Side effects of bisphosphonates include upper gastrointestinal symptoms and infrequent bone, joint, and/or muscle pain. Osteonecrosis of the jaw is another rare, but serious, side effect that was identified through post-marketing surveillance. According to a report of a task force of the American Society for Bone and Mineral Research, osteonecrosis of the jaw, formally defined as the presence of exposed bone in the maxillofacial region that does not heal within eight weeks of identification by a healthcare provider, was estimated to occur in between one in 10,000 to less than one in 100,000 patient years.Citation34 A recent re-evaluation of three large, randomized controlled trials of bisphosphonates has shown no increase in “atypical” femoral shaft fractures, which had previously been suggested to be linked to their use.Citation35
Estrogen
Estrogen has long been used in the prevention of osteoporosis, with widespread use beginning in the 1980s when it was cited by a US National Institutes of Health Consensus Conference as the most effective means for preventing bone loss.Citation36 Use of conjugated equine estrogen (CEE) in combination with progestins, to protect against adverse endometrial changes, continued to increase through the 1990s, so that by 2001 approximately 15 million women in the US aged 50–74 years were using estrogen therapy, with 42% of women of that age estimated to have had some exposure to hormone replacement therapy.Citation37
Following release of results of the Women’s Health Initiative (WHI) in 2002 showing increased adverse events associated with estrogen therapy, its use declined rapidly worldwide.38−42 Although confirming the association of estrogen with decreases in biochemical markers of osteoporosis of 50%–60%, a two-year increase in BMD of 4%–6% in the hip and spine, and decreased incidence of both vertebral and hip fractures of 34% after five years, the trial was stopped three years early due to significantly increased risks of coronary heart disease, stroke, pulmonary embolism, and breast cancer in estrogen/progestin users compared with the placebo group.Citation43 A year and a half later, the estrogen-only arm in post-menopausal women with hysterectomy was also stopped early due to increased incidence of stroke.Citation44
Estrogen therapy is now recommended for osteoporosis prevention only in patients with significant risk of osteoporosis and only after all nonestrogen medication has been carefully considered. The recommended starting dose is 0.3 mg CEE (plus 1.5 mg medroxyprogesterone acetate). Currently no estrogen (or progestin) product has a Food and Drug Administration (FDA) indication for treatment of osteoporosis.Citation45
SERMs
SERMs represent a growing number of compounds that act as either estrogen receptor agonists or antagonists in a tissue-specific manner. They are a chemically diverse group that lack the steroid structure of estrogen, but possess a tertiary structure that allows them to bind to estrogen receptors ER-alpha and/or ER-beta. The goal is to develop SERMs that dissociate the favorable estrogenic effects on bone and the cardiovascular system from unfavorable stimulatory effects associated with breast and endometrial cancer.
Currently there are two main chemical classes of SERMs approved for clinical use: triphenyl ethylene derivatives (tamoxifen and toremifene which are used to treat breast cancer) and benzothiopene derivatives (such as raloxifene, the only SERM currently indicated for the prevention and treatment of osteoporosis in the US). In 2007, raloxifene was also granted an indication for breast cancer prevention by the FDA.
Raloxifene is an oral medication given in a dose of 60 mg/day. Four major international trials have assessed the use of raloxifene in 37,000 postmenopausal women.Citation46 In two osteoporosis prevention trialsCitation47,Citation48 and two treatment trials of women with postmenopausal osteoporosis,Citation49,Citation50 raloxifene use has been associated with a 30% reduction in biochemical markers of osteoporosis, three-year increases in BMD of 2% and 3% at the hip and spine and decreased vertebral fractures by 30%–50% in women with pre-existing vertebral fractures or low bone density. It has not been shown to have a significant effect on nonvertebral or hip fractures. Raloxifene is associated with hormonally related side effects such as increased risk of blood clots and vasomotor symptoms, including hot flushes.
Two newer SERMs that have recently received approval in Europe, but are not yet approved in the US, are lasofoxifene and bazedoxifene (). Lasofoxifene is a third generation naphthalene derivative SERM that binds to both ERα and ERβ with high affinity. Its half-life is two times longer than that of raloxifene and it has better oral bioavailability.Citation51 Lasofoxifene has been tested in 17 Phase II/III trials involving more than 10,000 women for postmenopausal osteoporosis prevention or treatment, with key evidence coming from two large Phase III trials.Citation52 In the Osteoporosis Prevention and Lipid Lowering study involving 1,907 women, increases in lumbar BMD of 2.3% were observed among those receiving lasofoxifene 0.25 or 0.5 mg/day, compared with a 0.7% reduction in patients who received placebo.Citation53 The Postmenopausal Evaluation and Risk Reduction with Lasofoxifene (PEARL) trial demonstrated a reduction in vertebral fractures of 42% after three years and nonvertebral fractures, primarily forearm and wrist, of 24% among women with osteoporosis after five years of treatment.Citation54 Rates of venous thromboembolism were also significantly increased. Based on earlier data from the PEARL trial, an FDA application for lasofoxifene was submitted in September 2008. Approval is currently pending a response to a request for additional information. Lasofoxifene 0.5 mg/day was approved for treatment of osteoporosis by the European FDA counterpart, the European Medicines Agency, in 2009 and is available as a prescription drug there.
Table 2 Osteoporosis therapies not currently approved in the US
Bazedoxifene is another third generation SERM currently undergoing investigation in clinical trials. It is based on a raloxifene template with an indole ring substituting for the benzothioprine core.Citation55 In clinical trials of postmenopausal women with osteopenia, bazedoxifene 20 mg/day and 40 mg/day resulted in increases in BMD at the lumbar spine and other sites of approximately 1.5% and was associated with significant decreases in markers of bone turnover.Citation56 In Phase III trials, bazedoxifene in doses of 20 mg/day or 40 mg/day was associated with reduction of vertebral fractures of 39% and a nonsignificant reduction of all fractures of 16% over three years.Citation57 Among women at high risk of fracture in the next 10 years (22%) based on FRAX® score (WHO, University of Sheffield, UK), vertebral fractures were decreased by 50% and all fractures by 33%.Citation58 Bazedoxifene is in the later stages of the approval process at the US FDA for treatment of osteoporosis pending a request for additional safety information in 2008 from an FDA Advisory Committee. It was approved by the European Medicines Agency in April 2009.
Bazedoxifene is also being investigated for use in combination with conjugated estrogen as a “tissue selective estrogen complex (TSEC)” with the rationale that it will block estrogen stimulation of endometrial and breast tissue without the need for progestin therapy, while having an additive effect with estrogen on bone.Citation59 Results from a recent study of bazedoxifene-based TSECs showed the combination drug was associated with significantly greater increases in BMD at both spine and hip and significantly greater decreases in markers of bone turnover compared with raloxifene at most doses.Citation58
Problems with side effects and demonstrating efficacy in reducing fractures has prevented other SERMS, such as tibiloneCitation59 and arzoxifene,Citation60 from continuing toward approval. A number of other SERMs continue to be developed and await completion of testing in clinical trials.Citation61,Citation62
Calcitonin
Calcitonin is another antiresorptive agent approved for treatment of osteoporosis. Like the endogenous form of the hormone, it acts on the calcitonin receptor on osteoclasts to decrease their activity. Of the many synthetic or recombinant calcitonins from different species that have been used for medical purposes, including human calcitonin, porcine calcitonin, eel calcitonin-derivative, and salmon calcitonin, the salmon preparation (SCT) is the most widely used in clinical practice.Citation63
SCT is available as an injectable formulation for intravenous, intramuscular or subcutaneous use, and as a nasal spray. Injectable SCT was the first to be introduced and was approved in the US in 1984 and is available in 90 other countries for osteoporosis treatment.Citation63 SCT was approved as a nasal spray for treatment of postmenopausal osteoporosis in the US in 1995 and is currently the most commonly used calcitonin formulation, in part due to its convenience of administration.Citation63 Clinical trials of SCT nasal spray, taken at a dose of 200 IU/day, have demonstrated a 20% decrease in biomarkers of osteoporosis, a small effect on BMD in the spine (1%−2% increase),64−66 but a 36% reduced incidence of vertebral fractures in women with pre-existing vertebral fractures.Citation65 No consistent effect on nonvertebral or hip fractures has been demonstrated. An oral SCT preparation is currently in development for clinical use.Citation63
Anabolic agents
PTH
A PTH analog is the only anabolic agent currently approved for treatment of osteoporosis in the US where it is available in the form of human recombinant PTH peptide 1−34 (teriparatide), a fragment of PTH that has a similar affinity for PTH receptor-1. An additional form, rhPTH1–84, which is identical to the endogenous full length PTH in humans, is currently available in Europe.
Although physiologically PTH is released in response to low serum calcium and acts to mobilize calcium from the bone, pharmacologically, when given intermittently at low doses, it has been shown to have predominantly anabolic effects on osteoblasts. As indicated by markers of bone turnover, PTH initiates bone formation first and only later promotes bone resorption, resulting in an “anabolic window” of approximately 18−24 months in duration.Citation67
The recommended dose of teriparatide is 20 µg/day; given as a subcutaneous injection with a modified insulin-pen. In clinical trials overall, teriparatide was shown to: increase BMD at both the spine, up to 10%, and femur, to a lesser degree; and decrease vertebral fractures by about 65% and nonvertebral fractures by about 35%.Citation68,Citation69 Because its effects on BMD have not been consistent across trials, teriparatide is only approved for osteoporosis treatment and not prevention. Because the long-term safety and efficacy are not known, PTH can be prescribed for no more than 24 months. It is contraindicated in patients with hyperparathyroidism, hypercalcemia, or at risk of osteosarcoma, including those with unexplained high alkaline phosphatase levels, Paget’s disease, or who have undergone irradiation on the bones.Citation67
Strontium ranelate
Strontium ranelate is an oral agent that has been approved for use in osteoporosis treatment in European countries since 2004. It is not approved in the US, but a related compound, strontium malonate, has FDA investigational new drug status. Strontium ranelate consists of two atoms of strontium and an organic moiety (ranelic acid) which dissociates in the digestive tract. Like calcium, strontium is a cation that is incorporated into the crystal structure of bone.
Strontium ranelate acts by both stimulating bone formation and decreasing bone resorption. In vitro, strontium ranelate has been shown to increase osteoblastic activity, including increasing collagen synthesis and modulating the OPG/RANKL system in favor of OPG, as well as decrease bone resorption by decreasing osteoclast differentiation and resorbing activity, and increasing osteoclast apoptosis.Citation70 However, in vivo, some evidence suggests bone formation is favored with nonsignificant effects on bone resorption.Citation71
In a summary of the results of four clinical trials of strontium ranelate, three for treatment of osteoporosis72−74 and one for prevention,Citation75 2 g/day of strontium ranelate resulted in increased BMD at all sites, a 37% reduction in vertebral fractures and a 14% reduction in nonvertebral fractures over three years.Citation71 As a result, the treatment received a “silver level of evidence” for reducing vertebral, and to a lesser degree nonvertebral, fractures in postmenopausal women from the Cochrane Collaboration.Citation71 More recently, a five-year follow-up of one of the treatment trials demonstrated a 43% reduction in hip fractures and 24% reduction in vertebral fractures.Citation76
New agents
New PTH analogs
Ostabolin-C is a cyclic 31-amino acid analog of PTH that activates the same PTH1 Type receptor activated by the other currently available PTH analogs.Citation77 Unlike the current PTH analogs, however, ostabolin-C stimulates adenylyl cyclase alone and not in combination phospholipase C. These modifications are expected to limit its side effects.Citation78 In a Phase II trial, daily subcutaneous injections of ostabolin-C in postmenopausal women with osteoporosis resulted in an increase in spine BMD of up to 5% after four months as reported by the drug’s manufacturer.Citation79 Episodes of hypercalcemia were more frequent than in the placebo group only at the highest doses. Phase III trials of the injectable medication are now ongoing and a nasal spray preparation is under development.Citation79
New agents with new targets
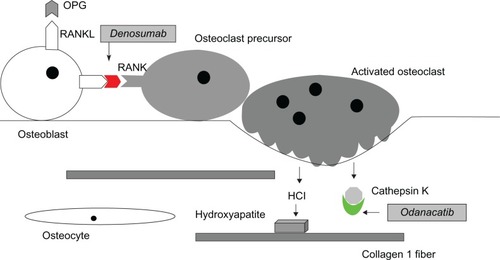
Denosumab is a human monoclonal antibody that binds to RANKL, the principal mediator of osteoclastic bone resorption (). By inhibiting the action of RANKL, denosumab causes a reduction in the differentiation, activity, and survival of osteoclasts, leading to lower rates of bone resorption.Citation80 It is given subcutaneously at a dose of 60 mg every six months. Denosumab has been proposed to have several advantages over bisphosphonate therapy, including the potential for increased compliance due to less frequent and easier administration (subcutaneous injection vs intravenous for zoledronic acid) with potentially fewer side effects.Citation81
Figure 2 New drug targets in RANK/RANKL/Osteoprotegerin signaling system. Odanacatib is an inhibitor of cathepsin K that prevents the osteoclast-secreted enzyme from breaking down collagen and other components of the bone matrix. Denosumab is a monoclonal antibody that targets the RANKL molecule, preventing its activation of the RANK receptor molecule on osteoclasts.
In the recently reported Phase III FREEDOM (Fracture Reduction Evaluation of Denosumab in Osteoporosis every six Months) trial of 7,868 women ages of 60–90 years with T-scores of −4.0 to −2.5 at the lumbar spine or total hip, subjects receiving denosumab had a significant reduction in vertebral fracture of 68%, in hip fracture of 40%, and in other nonvertebral fracture of 20% compared to those receiving placebo after three years.Citation82
In August 2009, the drug received FDA fast-track status for treatment of osteoporosis. Final approval was delayed in October 2009, pending additional information on the proposed post-marketing surveillance program and updated safety data. The information was provided in January 2010 and approval is expected in July 2010.Citation83 Denosumab received a positive opinion from the European Medicines Agency in December 2009, with final approval also expected in 2010.Citation84
Odanacatib is an orally administered inhibitor of cathepsin K being developed for treatment of osteoporosis and bone metastases. As described above, cathepsin K is the major collagenase secreted by osteoclasts to degrade the organic bone matrix during the bone remodeling process (). In a recently reported Phase II clinical trial in postmenopausal women with osteoporosis, 24 months of treatment with odanacatib 50 mg/week produced increases in BMD of 5.5% at the spine and 3.2% at the hip.Citation85 Side effects appeared to be minimal, in contrast to earlier trials of another cathepsin K inhibitor that had been associated with skin problems including sclerosis.Citation86 Phase III trials of odanacatib that will involve up to 20,000 women are ongoing.
Emerging therapies
New discoveries related to pathways regulating osteoblast and osteoclast function are leading to the development an increasing number of osteoporosis drugs with novel targets. The Wnt/β-catenin pathway that regulates gene transcription of proteins important for osteoblast function is one such target (). Wnt signaling is activated by one of 19 secreted Wnt proteins binding to one of 10 frizzled receptors, initiating a signaling cascade which results in the release of β-catenin from a complex containing glycogen synthase kinase 3β (GSK3β), and its subsequent accumulation and translocation into the nucleus. β-catenin then binds with the transcription factor tcf/lef and initiates target gene transcription that leads to increased bone formation.Citation87
Figure 3 Wnt/β-catenin pathway in osteoblasts. Binding of the Wnt molecule to co-receptors on the osteoblast–lipoprotein-related protein (LRP 5/6) and Frizzled (Frzd) – activates release of β-catenin within the cell from a complex containing glycogen serine kinase (GSK-3β), resulting in accumulation of β-catenin and translocation into the nucleus where it regulates gene expression. Sclerostin (Sost) and dickkopf (DKK-1) are two proteins that inhibit LRP 5/6 from activating this pathway, resulting in degradation of β-catenin by GSK-3β. Antibodies to both sclerostin and DKK-1 are currently under development as potential anabolic (osteoblast-stimulating) osteoporosis therapies. (Graphic adapted from Hoeppner et alCitation95 and Gallagher and Sai.Citation98)
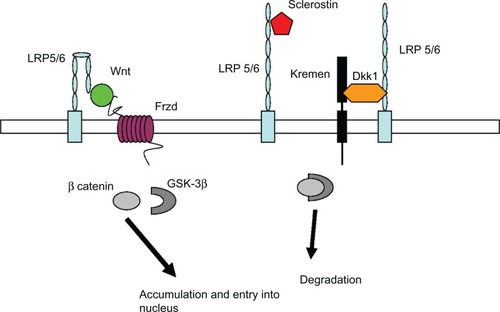
The first clues of the importance of the pathway in bone regulation were studies showing specific mutations of the gene for a Wnt receptor, lipoprotein receptor-like protein 5 (LRP5), were involved in syndromes of osteoporosis (osteoporosis pseudoglioma); other mutations of the same gene were subsequently associated with high bone mass. LRP5 is a co-receptor along with the frizzled receptors for Wnt proteins. Study of the pathway has led to further discovery of inhibitors of Wnt signaling secreted by osteocytes. These include sclerostin and dickkopf 1 protein (DKK1), both of which block binding of Wnt to LRP5 (or the related LRP6 receptor), thereby inhibiting osteoblast stimulation. Sclerostin is the protein product of the SOST gene, mutations of which cause sclerosing bone diseases.Citation88,Citation89 Decreased sclerostin secretion has been implicated as the signal for increasing Wnt pathway activity in mechanical stimulation of bone.Citation90
Monoclonal antibodies designed to block the inhibiting action of both sclerostin and DKK1 are being considered for clinical trials based on promising results in animal models.91−93 Because both of these molecules appear to be secreted only by bone, it is hoped that they will have fewer systemic adverse effects than other Wnt pathway-related therapies. Therapies targeted at other molecules in the pathway, for example a small molecule inhibitor of GSK3β,Citation94 the enzyme which causes degradation of β-catenin in the absence of Wnt signaling, are considered less desirable targets due to their action in many tissues in addition to bone.Citation95
Therapies being developed based on other targets include calcium receptor antagonists that stimulate transient release of PTH from the parathyroid gland.Citation96 Bone morphogenetic proteins, growth factors belonging to TGF-β superfamily and involved in a multitude of processes including embryonic and post natal development, are potent bone inducers being used in clinical studies for local fracture healing. Their potential for treatment in osteoporosis is also being explored.Citation97
Conclusion
Many new agents for osteoporosis therapy are currently in the development pipeline. Several of these agents, including denosumab, a monoclonal antibody that blocks the actions of the collagenase cathepsin K, are nearing US FDA approval. Further elucidation of the role of Wnt signaling and other pathways in osteoblasts promises to add more treatment options in the coming decade, with a greater emphasis on anabolic agents. These agents may also be useful in combination with existing antiresorptive agents, further expanding therapeutic options in the future.
Acknowledgments
This is manuscript 20746-MEM. The work was supported by a grant from the National Institutes of Health AR054901-01A2.
Disclosure
The author reports no conflicts of interest in this work.
References
- CurtisJRMcClureLADelzellEPopulation-based fracture risk assessment and osteoporosis treatment disparities by race and genderJ Gen Intern Med20092495696219551449
- McClungMRThe relationship between bone mineral density and fracture riskCurr Osteoporos Rep20053576316036103
- World Health OrganizationAssessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study GroupWorld Health Organ Tech Rep Ser199484311297941614
- International Osteoporosis FoundationFacts and statistics about osteoporosis and its impact2009 Available from: http://www.iofbone-health.org/facts-and-statistics.htmlAccessed Apr 7, 2010
- National Osteoporosis FoundationFast facts on osteoporosis2008 Available from: http://www.nof.org/osteoporosis/diseasefacts.htmAccessed Apr 7, 2010
- KanisJAMcCloskeyEVJohanssonHStromOBorgstromFOdenAHow to decide who to treatBest Pract Res Clin Rheumatol20092371172619945684
- LimLSHoeksemaLJSherinKScreening for osteoporosis in the adult US population: ACPM position statement on preventive practiceAm J Prev Med20093636637519285200
- World Health OrganizationFRAX®WHO fracture risk assessment tool2008 Available from: http://www.sheffield.ac.uk/FRAX/Accessed Apr 7, 2010
- National Osteoporosis Foundation2008Clinician’s guide to prevention and treatment of osteoporosis Available from: http://www.nof.org/professionals/pdfs/NOF_ClinicianGuide2009_v7.pdfAccessed Apr 7, 2010
- SeemanECompstonJAdachiJNon-compliance: the Achilles’ heel of anti-fracture efficacyOsteoporos Int20071871171917245547
- CawstonTEYoungDAProteinases involved in matrix turnover during cartilage and bone breakdownCell Tissue Res201033922123519915869
- SommerfeldtDWRubinCTBiology of bone and how it orchestrates the form and function of the skeletonEur Spine J200110Suppl 2S86S9511716022
- AhlborgHGJohnellONilssonBEJeppssonSRannevikGKarlssonMKBone loss in relation to menopause: a prospective study during 16 yearsBone20012832733111248665
- ChristakosSDhawanPShenQPengXBennBZhongYNew insights into the mechanisms involved in the pleiotropic actions of 1,25 dihydroxyvitamin D3Ann N Y Acad Sci2006106819420316831919
- De PaulaFJRosenCJBack to the future: revisiting parathyroid hormone and calcitonin control of bone remodelingHorm Metab Res20104229930620217631
- NakamuraTImaiYMatsumotoTEstrogen prevents bone loss via estrogen receptor alpha and induction of Fas ligand in osteoclastsCell200713081182317803905
- KrumSAMiranda-CarboniGAHauschkaPVEstrogen protects bone by inducing Fas ligand in osteoblasts to regulate osteoclast survivalEMBO J20082753554518219273
- WrightHLMcCarthyHSMiddletonJMarshallMJRANK, RANKL, and osteoprotegerin in bone biology and diseaseCurr Rev Musculoskelet Med20092566419468919
- LewieckiEMMonitoring pharmacological therapy for osteoporosisRev Endocr Metab Disord201029 Epub ahead of print
- National Osteoporosis FoundationUpdated recommendations for calcium and vitamin D intake102008 Available from: http://www.nof.org/prevention/calcium_and_VitaminD.htmAccessed Apr 7, 2010
- GindeAALiuMCCamargoCAJrDemographic differences and trends of vitamin D insufficiency in the US population, 1988–2004Arch Intern Med200916962663219307527
- DeLucaHFOverview of general physiologic features and functions of vitamin DAm J Clin Nutr200480Suppl 61689S1696S15585789
- LipsPWorldwide status of vitamin D nutritionJ Steroid Biochem Mol Biol20101211–229730020197091
- National Institutes of Health, Office of Dietary SupplementsDietary supplement fact sheet: vitamin D11132009 Available from: http://ods.od.nih.gov/factsheets/vitamind.aspAccessed May 19, 2010
- AdamsJSHewisonMUpdate in vitamin DJ Clin Endocrinol Metab20109547147820133466
- American College of Sports MedicineExercise and osteoporosis2007 Available from: http://www.acsm.org/AM/Template.cfm?Section=Home_Page&Template=/CM/HTMLDisplay.cfm&ContentID=8170Accessed May 19, 2010
- National Osteoporosis FoundationExercise for healthy bones2008 Available from: http://www.nof.org/prevention/exercise.htmAccessed May 19, 2010
- FitzpatrickLASecondary causes of osteoporosisMayo Clin Proc20027745346812004995
- HanleyDAIoannidisGAdachiJDEtridronate therapy in the treatment and prevention of osteoporosisJ Clin Densitom20003799510745305
- FredianiBCavalieriLCremonesiGClodronic acid formulations available in Europe and their use in osteoporosis: a reviewClin Drug Investig200929359379
- DrakeMTClarkeBLKhoslaSBisphosphonates: mechanism of action and role in clinical practiceMayo Clin Proc2008831032104518775204
- WattsNBDiabDLLong-term use of bisphosphonates in osteoporosisJ Clin Endocrinol Metab2010951555156520173017
- RussellRGWattsNBEbetinoFHRogersMJMechanisms of action of bisphosphonates: similarities and differences and their potential influence on clinical efficacyOsteoporos Int20081973375918214569
- KhoslaSBurrDCauleyJBisphosphonate-associated osteonecrosis of the jaw: report of a task force of the American Society for Bone and Mineral ResearchJ Bone Miner Res2007221479149117663640
- BlackDMKellyMPGenantHKBisphosphonates and fractures of the subtrochanteric or diaphyseal femurN Engl J Med20103621761177120335571
- National Institutes of HealthOsteoporosis. NIH consensus development conference statementNatl Inst Health Consens Dev Conf Consens Statement1984536
- HershALStefanickMLStaffordRSNational use of postmenopausal hormone therapy: annual trends and response to recent evidenceJAMA2004291475314709575
- HaasJSKaplanCPGerstenbergerEPKerlikowskeKChanges in the use of postmenopausal hormone therapy after the publication of clinical trial resultsAnn Intern Med200414018418814757616
- BarbagliaGMaciaFComasMTrends in hormone therapy use before and after publication of the Women’s Health Initiative trial: 10 years of follow-upMenopause2009161061106419369903
- FaberABouvyMLLoskampLvan de BergPBEgbertsTCde Jong-van den BergLTDramatic change in prescribing of hormone replacement therapy in The Netherlands after publication of the Million Women Study: a follow-up studyBr J Clin Pharmacol20056064164716305589
- HuotLCourisCMTainturierVJaglalSColinCSchottAMTrends in HRT and anti-osteoporosis medication prescribing in a European population after the WHI studyOsteoporos Int2008191047105418373055
- MartinRMWheelerBWMetcalfeCGunnellDWhat was the immediate impact on population health of the recent fall in hormone replacement therapy prescribing in England? Ecological studyJ Public Health (Oxf)2010328 Epub ahead of print
- RossouwJEAndersonGLPrenticeRLRisks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trialJAMA200228832133312117397
- AndersonGLLimacherMAssafAREffects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trialJAMA20042911701171215082697
- StefanickMLEstrogens and progestins: background and history, trends in use, and guidelines and regimens approved by the US Food and Drug AdministrationAm J Med200519118 Suppl 12647316414329
- GoldsteinSRDuvernoyCSCalafJRaloxifene use in clinical practice: efficacy and safetyMenopause20091641342119092711
- DelmasPDBjarnasonNHMitlakBHEffects of raloxifene on bone mineral density, serum cholesterol concentrations, and uterine endometrium in postmenopausal womenN Engl J Med1997337164116479385122
- JohnstonCCJrBjarnasonNHCohenFJLong-term effects of raloxifene on bone mineral density, bone turnover, and serum lipid levels in early postmenopausal women: three-year data from 2 double-blind, randomized, placebo-controlled trialsArch Intern Med20001603444345011112238
- EttingerBBlackDMMitlakBHReduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: results from a 3-year randomized clinical trial. Multiple Outcomes of Raloxifene Evaluation (MORE) InvestigatorsJAMA199928263764510517716
- MartinoSCauleyJABarrett-ConnorEContinuing outcomes relevant to Evista: breast cancer incidence in postmenopausal osteoporotic women in a randomized trial of raloxifeneJ Natl Cancer Inst2004961751176115572757
- GennariLMerlottiDNutiRSelective estrogen receptor modulator (SERM) for the treatment of osteoporosis in postmenopausal women: focus on lasofoxifeneClin Interv Aging20105192920169039
- LewieckiEMLasofoxifene for the prevention and treatment of postmenopausal osteoporosisTher Clin Risk Manag2009581782719898646
- GennariLMerlottiDValleggiFMartiniGNutiRSelective estrogen receptor modulators for postmenopausal osteoporosis: current state of developmentDrugs Aging20072436137917503894
- CummingsSREnsrudKDelmasPDLasofoxifene in postmenopausal women with osteoporosisN Engl J Med201036268669620181970
- GennariLMerlottiDDe PaolaVMartiniGNutiRBazedoxifene for the prevention of postmenopausal osteoporosisTher Clin Risk Manag200841229124219337430
- MillerPDChinesAAChristiansenCEffects of bazedoxifene on BMD and bone turnover in postmenopausal women: 2-yr results of a randomized, double-blind, placebo-, and active-controlled studyJ Bone Miner Res20082352553518072873
- KanisJAJohanssonHOdenAMcCloskeyEVBazedoxifene reduces vertebral and clinical fractures in postmenopausal women at high risk assessed with FRAXBone2009441049105419254788
- LindsayRGallagherJCKaganRPickarJHConstantineGEfficacy of tissue-selective estrogen complex of bazedoxifene/conjugated estrogens for osteoporosis prevention in at-risk postmenopausal womenFertil Steril2009921045105219635616
- CummingsSREttingerBDelmasPDThe effects of tibolone in older postmenopausal womenN Engl J Med200835969770818703472
- De PaulaFJRosenCJDeveloping drugs to treat osteoporosis: lessons learned?Expert Opin Pharmacother20101186786920113199
- ShellyWDraperMWKrishnanVWongMJaffeRBSelective estrogen receptor modulators: an update on recent clinical findingsObstet Gynecol Surv20086316318118279543
- VogelvangTEvan der MoorenMJMijatovicVKenemansPEmerging selective estrogen receptor modulators: special focus on effects on coronary heart disease in postmenopausal womenDrugs20066619122116451093
- ChesnutCHIIIAzriaMSilvermanSEngelhardtMOlsonMMindeholmLSalmon calcitonin: a review of current and future therapeutic indicationsOsteoporos Int20081947949118071651
- OvergaardKEffect of intranasal salmon calcitonin therapy on bone mass and bone turnover in early postmenopausal women: a dose-response studyCalcif Tissue Int19945582867953984
- ChesnutCHIIISilvermanSAndrianoKA randomized trial of nasal spray salmon calcitonin in postmenopausal women with established osteoporosis: the prevent recurrence of osteoporotic fractures study. PROOF Study GroupAm J Med200010926727610996576
- ChesnutCHIIIMajumdarSNewittDCEffects of salmon calcitonin on trabecular microarchitecture as determined by magnetic resonance imaging: results from the QUEST studyJ Bone Miner Res2005201548156116059627
- Pleiner-DuxneunerJZwettlerEPaschalisERoschgerPNell-DuxneunerVKlaushoferKTreatment of osteoporosis with parathyroid hormone and teriparatideCalcif Tissue Int20098415917019189037
- TrevisaniVFRieraRImotoAMSaconatoHAtallahANTeriparatide (recombinant human parathyroid hormone 1–34) in postmenopausal women with osteoporosis: systematic reviewSao Paulo Med J200812627928419099162
- VestergaardPJorgensenNRMosekildeLSchwarzPEffects of parathyroid hormone alone or in combination with anti-resorptive therapy on bone mineral density and fracture risk – a meta-analysisOsteoporos Int200718455716951908
- NeuprezAHiligsmannMScholtissenSBruyereOReginsterJYStrontium ranelate: the first agent of a new therapeutic class in osteoporosisAdv Ther2008251235125619066755
- O’DonnellSCranneyAWellsGAAdachiJDReginsterJYStrontium ranelate for preventing and treating postmenopausal osteoporosisCochrane Database Syst Rev20063CD00532616856092
- MeunierPJSlosmanDODelmasPDStrontium ranelate: dose-dependent effects in established postmenopausal vertebral osteoporosis – a 2-year randomized placebo controlled trialJ Clin Endocrinol Metab2002872060206611994341
- MeunierPJRouxCSeemanEThe effects of strontium ranelate on the risk of vertebral fracture in women with postmenopausal osteoporosisN Engl J Med200435045946814749454
- ReginsterJYSeemanEDe VernejoulMCStrontium ranelate reduces the risk of non-vertebral fractures in postmenopausal women with osteoporosis: Treatment of Peripheral Osteoporosis (TROPOS) studyJ Clin Endocrinol Metab2005902816282215728210
- ReginsterJYDeroisyRDougadosMJupsinIColetteJRouxCPrevention of early postmenopausal bone loss by strontium ranelate: the randomized, two-year, double-masked, dose-ranging, placebo-controlled PREVOS trialOsteoporos Int20021392593112459934
- ReginsterJYFelsenbergDBoonenSEffects of long-term strontium ranelate treatment on the risk of non-vertebral and vertebral fractures in postmenopausal osteoporosis: results of a five-year, randomized, placebo-controlled trialArthritis Rheum2008581687169518512789
- NemethEFZT-031, a cyclized analog of parathyroid hormone (1–31) for the potential treatment of osteoporosisIDrugs20081182784018988128
- WhitfieldJFMorleyPWillickGCyclization by a specific lactam increases the ability of human parathyroid hormone (hPTH)-(1–31) NH2 to stimulate bone growth in ovariectomized ratsJ Bone Miner Res199712124612529258755
- ZelosZelos Therapeutics’ Ostabolin-C™ increases bone mineral density in phase 2 osteoporosis trial2010 Available from: http://www.zelostherapeutics.com/news/020807.htmAccessed Jun 6, 2010
- LewieckiEMTreatment of osteoporosis with denosumabMaturitas20106618218620236778
- SchwarzEMRitchlinCTClinical development of anti-RANKL therapyArthritis Res Ther20079Suppl 1S717634146
- CummingsSRSanMJMcClungMRDenosumab for prevention of fractures in postmenopausal women with osteoporosisN Engl J Med200936175676519671655
- Amgen, IncFDA classifies prolia™ (denosumab) complete response submission and targets action date22010 Available from: http://finance.yahoo.com/news/FDA-Classifies-ProliaTM-prnews-2110666215.html?x=0&.v=1Accessed April 7, 2010
- Amgen, IncAmgen receives CHMP positive opinion for prolia™ (denosumab) in the European Union12182009 Available from: http://www.amgen.com/media/media_pr_detail.jsp?year=2009&releaseID=1367560Accessed Apr 15, 2010
- BoneHGMcClungMRRouxCOdanacatib, a cathepsin-K inhibitor for osteoporosis: a two-year study in postmenopausal women with low bone densityJ Bone Miner Res201025593794719874198
- PeroniAZiniABragaVColatoCAdamiSGirolomoniGDrug-induced morphea: report of a case induced by balicatib and review of the literatureJ Am Acad Dermatol20085912512918410981
- BaronRRawadiGTargeting the Wnt/beta-catenin pathway to regulate bone formation in the adult skeletonEndocrinology20071482635264317395698
- BalemansWEbelingMPatelNIncreased bone density in sclerosteosis is due to the deficiency of a novel secreted protein (SOST)Hum Mol Genet20011053754311181578
- BalemansWPatelNEbelingMIdentification of a 52 kb deletion downstream of the SOST gene in patients with van Buchem diseaseJ Med Genet200239919711836356
- RoblingAGNiziolekPJBaldridgeLAMechanical stimulation of bone in vivo reduces osteocyte expression of SOST/sclerostinJ Biol Chem20082835866587518089564
- LiXOminskyMSWarmingtonKSSclerostin antibody treatment increases bone formation, bone mass, and bone strength in a rat model of postmenopausal osteoporosisJ Bone Miner Res20092457858819049336
- BettsAMClarkTHYangJThe application of target information and preclinical pharmacokinetic/pharmacodynamic modeling in predicting clinical doses of a dickkopf-1 antibody for osteoporosisJ Pharmacol Exp Ther201033321320089807
- OminskyMSVlasserosFJoletteJTwo doses of sclerostin antibody in cynomolgus monkeys increases bone formation, bone mineral density, and bone strengthJ Bone Miner Res201025594895920200929
- KulkarniNHOnyiaJEZengQOrally bioavailable GSK-3alpha/beta dual inhibitor increases markers of cellular differentiation in vitro and bone mass in vivoJ Bone Miner Res20062191092016753022
- HoeppnerLHSecretoFJWestendorfJJWnt signaling as a therapeutic target for bone diseasesExpert Opin Ther Targets20091348549619335070
- KumarSMathenyCJHoffmanSJAn orally active calcium-sensing receptor antagonist that transiently increases plasma concentrations of PTH and stimulates bone formationBone20104653454219786130
- LiBBone morphogenetic protein-Smad pathway as drug targets for osteoporosis and cancer therapyEndocr Metab Immune Disord Drug Targets2008820821918782017
- GallagherJCSaiAJMolecular biology of bone remodeling: implications for new therapeutic targets for osteoporosisMaturitas20106530130720116187