Abstract
Fibrolamellar carcinoma (FLC) is a variant of hepatocellular carcinoma (HCC), which comprises ∼1%–9% of all HCCs. Although FLC is a variant of HCC, it is distinct from HCC in that it most often affects younger patients (10–35 years of age) with no underlying liver disease. FLC often presents with vague abdominal pain, nausea, abdominal fullness, malaise, and weight loss. Surgery is the current mainstay of treatment for FLC and remains the only potentially curative option. While FLCs are considered less responsive to chemotherapy than their classic HCC counterparts, there have been suggestions that multimodality treatments may be effective, especially in advanced cases. Further research is necessary to determine effective systemic therapies as an adjunct to surgery for FLC.
Introduction
Fibrolamellar carcinoma (FLC) is a variant of hepatocellular carcinoma (HCC) that comprises ∼1%–9% of all HCCs according to the SEER database.Citation1 FLC was first described by Edmondson in 1956 as an adult type of liver tumor in a 14-year-old female with no underlying liver disease.Citation2 The term FLC was not suggested, however, until 1980 when Craig et al described a set of patients with a unique histologic variant of HCC.Citation3 The World Health Organization (WHO) Classification of Tumors subsequently recognized FLC as having a unique histological pattern; however, it took until 2010 for the WHO to designate this clinical entity with its own WHO classification number.Citation4
Although FLC is a variant of HCC, it is distinct from HCC in that FLC most often affects younger patients (10–35 years of age) with no underlying liver disease.Citation5,Citation6 On pathological analysis, FLC is characterized by large tumor cells with deeply eosinophilic cytoplasm due to abundant mitochondria and prominent nuclei arranged in cords surrounded by lamellated collagen fibers.Citation3,Citation7 The tumor cells can demonstrate hepatocellular features; however, FLC tumors also can display both biliary and neuroendocrine differentiation. While the etiology of FLC tumors remains still unclear, FLC is thought to have an overall better prognosis than other primary liver tumors (eg, HCC, intrahepatic cholangiocarcinoma). We herein review the epidemiology, diagnosis, treatment, and prognosis of patients with FLC.
Epidemiology
FLC accounts for between 1% and 9% of all HCCs depending on the population studied.Citation8–Citation15 From an epidemiologic viewpoint, one feature that often distinguishes FLC from HCC is the age at diagnosis. FLC typically occurs in young adults, with most patients being 10–35 years of age at presentation compared with an average age of 65 years at presentation among patients with HCC.Citation5 Compared with HCC, some studies note that FLC patients are more likely to be female, while others have noted no specific sex predilection.Citation5,Citation10,Citation13 Regarding race, one study that utilized SEER data noted a higher incidence of FLC versus HCC among patients of Caucasian ethnicity; however, the association of race with HCC subtype did not remain significant after adjustment for age.Citation5 In addition, FLC has been reported with similar prevalence in countries across the globe including the United States, Mexico, Sweden, Saudi Arabia, Thailand, France, Canada, South Africa, Japan, Korea, India, Taiwan, and United Kingdom. As such, the data would suggest that there is no strong association of race or ethnicity with the risk of FLC.Citation5,Citation8–Citation26
Presentation
FLC often presents with vague abdominal pain, nausea, abdominal fullness, malaise, and weight loss.Citation3 While the physical examination is often within normal limits, when present, common physical findings include a palpable abdominal mass or hepatomegaly with or without pain in the right upper quadrant. Other reported rare presentations include jaundice due to biliary obstruction,Citation27–Citation29 gynecomastia in males,Citation30 fulminant liver failure,Citation6,Citation31–Citation33 recurrent deep vein thrombosis,Citation34 encephalopathy,Citation35 thrombophlebitis of the lower extremity,Citation36 anemia,Citation37 ascites,Citation38 and hypoglycemia.Citation39
On serum analysis, beta human chorionic gonadotropin can sometimes be elevated.Citation40 Typically, liver function markers such as aspartate aminotransferase, alanine aminotransferase, and alkaline phosphatase levels are normal or mildly elevated.Citation3,Citation10,Citation41 Elevated alkaline phosphatase levels in the setting of FLC are likely due to the growth of the tumor into the biliary tree or biliary obstruction.Citation42 Alpha fetoprotein levels are predominately normal in patients with FLC unlike in traditional HCC.Citation43 While uncommon, other serum proteins may be elevated with FLC. For example, transcobalamin I (also known as haptocortin), which normally protects vitamin B12 from degradation in the digestive tract, may be elevated.Citation44–Citation46 Transcobalamin II, a vitamin B12-binding protein induced by vitamin K absence/antagonist-II levels, may also be high.Citation13,Citation22,Citation47 Less frequently, elevations in serum proteins including fibrinogen and neurotensin can be noted.Citation33,Citation48 No large study has determined, however, the diagnostic accuracy of these serum proteins as tumor markers.
Diagnosis
Imaging
Due to the vague symptoms associated with FLC, diagnosis is usually made on the basis of both clinical presentation and diagnostic imaging studies. Imaging studies including ultrasound, computed tomography (CT) scan, and magnetic resonance imaging (MRI) may all be useful. On ultrasound, FLC is characterized as a well-defined mass that has heterogenous echogenicity.Citation49 Rather than ultrasound, cross-sectional imaging is the preferred mechanism to characterize most liver lesions, including FLC. CT scans that included an unenhanced phase followed by an intravenous contrast-enhanced hepatic arterial phase, a portal venous phase, and a delayed phase are recommended.Citation50 Using contrast-enhanced CT, FLC typically presents as a large (7–20 cm), heterogeneous, well-defined mass with a lobulated outline.Citation51 On the unenhanced phase, FLC is most often hypoattenuating with calcifications (40%–68%) and a central stellate scar (65%–75%), which is not seen in traditional HCC.Citation49,Citation51,Citation52 Necrosis without intratumoral hemorrhage is also a common finding in FLC.Citation49,Citation51 On hepatic arterial phase, most FLC lesions appear with heterogeneous hyperattenuation due to the large hypervascular tumor cells surrounding hypovascular fibrotic bands, as well as necrosis.Citation49,Citation51 The portal venous-phase CT characteristics of FLC are more variable. In ∼50% of patients, FLC tumors are isoattenuating to the liver in the portal venous phase, while in 30%–40% and 10%–20%, the lesions are either hyperattenuating or hypoattenuating, respectively.Citation50,Citation51
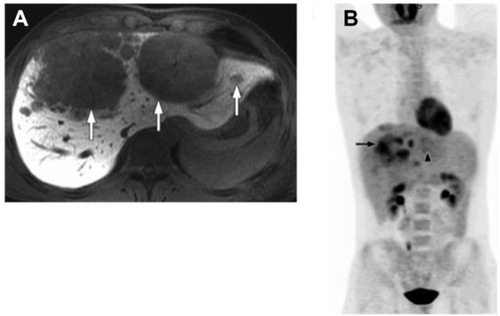
In many centers, MRI is the preferred imaging modality. MRI can be quite helpful in distinguishing FLC from other liver lesions. FLC tumors are usually hypointense on T1-weighted images and hyperintense on T2-weighted images with a fibrous central scar that remains hypointense on both T1- and T2-weighted images.Citation50,Citation51 The hypointensity of the central scar can help differentiate FLC from benign liver masses such as focal nodular hyperplasia, which typically has a predominately hyperintense central scar on T2-weighted images. Gadolinium contrast-enhanced MRI is used by many institutions to help further characterize liver lesions. On gadolinium-enhanced MRI, FLC is characterized by marked heterogeneous enhancement on the arterial phase that washes out and leaves an isointense or hypointense lesion on the portal venous phase.Citation50,Citation51
The role of 18F-FDG positron emission tomography–computed tomography (PET/CT) in the workup of FLC has not been well studied. Limited case series have suggested that PET/CT may be a useful tool in the diagnosis and monitoring of FLC as it may be FDG avid in up to 75% of patients ().Citation53,Citation54 As such, FDG-PET may be especially helpful in distinguishing FLC from focal nodular hyperplasia, the latter not being FDG avid.Citation53 Before routine utilization of PET/CT can be recommended, further investigations of the effectiveness of PET/CT in FLC are warranted.
Figure 1 A 22-year-old man with fibrolamellar HCC.
Abbreviations: HCC, hepatocellular carcinoma; MR, magnetic resonance; PET, positron emission tomography; CT, computed tomography; FDG, fludeoxyglucose.
Pathology
While cross-sectional imaging can strongly suggest FLC, confirmation of the diagnosis can only be achieved with the use of a biopsy. While a needle biopsy is often obtained, a definitive diagnosis can be difficult to confirm by fine-needle biopsy, and occasionally, additional tissue (eg, core biopsy) is required for accurate diagnosis. It is important to note, however, that biopsy is typically not necessary – nor recommended – if the lesion is highly suspicious for FLC on cross-sectional imaging and resection is feasible. Under these circumstances, rather than biopsy, surgery should be recommended. Rather, biopsy should more commonly be reserved for those circumstances of true diagnostic uncertainty or when the lesion is not amenable to resection and the tissue is required to direct other nonsurgical therapy.
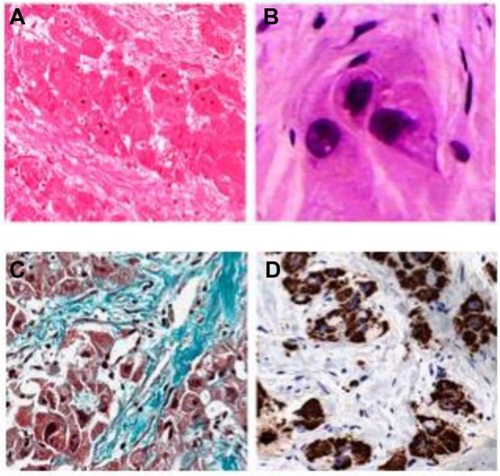
On pathology, FLC tumors tend to be large, yellow/tan, hypervascular, well-circumscribed masses with areas of necrosis in otherwise normal liver parenchyma. Up to 75% of tumors may have a central stellate scar and prominent fibrous tissue.Citation55 Microscopically, FLC is characterized by large polygonal or spindle-shaped tumor cells with deeply eosinophilic cytoplasm due to abundant mitochondria and prominent nuclei arranged in cords surrounded by lamellated collagen fibers ().Citation3,Citation7,Citation56 In fact, the average size of FLC tumors cells is roughly three times larger than normal hepatocytes and 1.6 times larger than HCC tumor cells.Citation57 Round- to oval-shaped cytoplasmic pale bodies lacking a nucleus and intracytoplasmic hyaline droplets are also seen on microscopy but are not required for diagnosis.Citation58 Generally, there is no cirrhosis in the surrounding liver parenchyma; however, there may be nonspecific inflammation suggested by the presence of mononuclear cells and lymphocytes.Citation56 Electron microscopy often demonstrates an increase in the number of mitochondria – a pathological feature specific to FLC.Citation3
Figure 2 Typical histological features of FLHCC.
Abbreviation: FLHCC, fibrolamellar hepatocellular carcinoma.
Immunohistochemical staining of FLC has some similarities to HCC, including staining positive for hepatocyte paraffin 1. However, unlike HCC, FLC often stains strongly for CK7 and epithelial membrane antigen, which are characteristic of biliary differentiation as well as markers of hepatic differentiation (CK19 and EpCAM).Citation51,Citation59 In addition, unlike most HCC, FLC stains negative for alpha fetoprotein.Citation51,Citation59 Furthermore, FLC tends to express CD133 and CD44 markers that are associated with stem cells.Citation60 FLC also stains more often and more diffusely for epithelial growth factor receptor and transforming growth factor beta than classic HCC.Citation59,Citation61 Transforming growth factor beta has been shown to be a profibrotic factor that may account for the lamellar pattern characteristic of FLC tumors on pathology.Citation59,Citation61
In addition to pathologic evaluation and immunohistochemical staining, there are genetic differences discovered recently which distinguish FLC from normal liver parenchyma and HCC. A 400 kb deletion in chromosome 19 seen in 100% of the FLC tumors tested by Honeyman et al results in a functional DNAJB1-PRKACA chimeric transcript, which further defines FLC as a unique entity.Citation62,Citation63
Treatment
Surgical resection
When feasible, surgery is the cornerstone therapeutic modality for patients with FLC as it represents the only potentially curative option. Complete surgical resection of the FLC tumor with negative margins along with an adequate lymph node dissection is the ideal treatment. In a systematic review by Mavros et al, the authors analyzed 575 patients with FLC.Citation64 The authors noted that patients who underwent resection of FLC had a 5-year survival of 70% compared with 0% among those patients who did not undergo surgical resection.Citation64 The average size of the FLC tumor resected was between 9 cm and 13 cm.Citation6,Citation50,Citation65 In a separate study, Stipa et al reported on 28 resected FLC patients and noted that 75% of the patients who underwent surgery for FLC required either a hemi-hepatectomy or an extended hepatectomy.Citation6 As the surgeries are often complex, a complete (R0) resection is not always possible, but it is important for survival. In a study by Darcy et al, which looked at 21 patients who underwent resection for FLC at a highly specialized cancer center, a complete (R0) resection was achieved in 17 (80.9%) patients, an R1 in two patients (9.5%), and an R2 in two patients (9.5%).Citation65 The overall 5-year survival in this cohort was 42.6% (95% confidence interval, 20–65.2), while the 5-year overall survival of those who underwent complete resection was 51.6%. Improved long-term overall survival was associated with R0 resection (P=0.003).Citation65 In addition to R0 resection, regional lymph node dissection is warranted due to the high incidence of lymph node metastasis and regional recurrence in patients with nodal disease.Citation6,Citation66,Citation67
Several factors are associated with a better prognosis following surgery including younger age at diagnosis, earlier tumor stage at diagnosis, as well as absence of large vessel invasion or thrombosis.Citation5,Citation12 Factors associated with a particularly poor prognosis include lymph node metastasis, multiple tumors, metastatic disease at presentation, and vascular invasion.Citation6,Citation13,Citation65,Citation68 There have been conflicting data regarding sex as a prognostic factor, as studies have variably reported female sex to be both a favorable and adverse factor associated with long-term survival ().Citation5,Citation68,Citation69 Prognosis following resection of FLC has also been suggested to be better than typical HCC ().Citation3,Citation5–Citation7,Citation58,Citation70 There are several factors that may contribute to the better prognosis of FLC patients, including that FLC patients are typically younger and healthier. In addition, FLC patients have normal underlying liver parenchyma, which may allow for more aggressive resections and decrease the risk of de novo future disease. As noted, the ability to perform complete resection has been reported to be one of the most important and well described prognostic factors for FLC.Citation5,Citation6,Citation65,Citation68,Citation71
Figure 3 Overall survival of patients with FLC or HCC managed with a liver-directed procedure from the time of diagnosis in SEER from 1986 to 2008.
Abbreviations: FLC, fibrolamellar carcinoma; HCC, hepatocellular carcinoma; SEER, Surveillance, Epidemiology, and End Results Program.
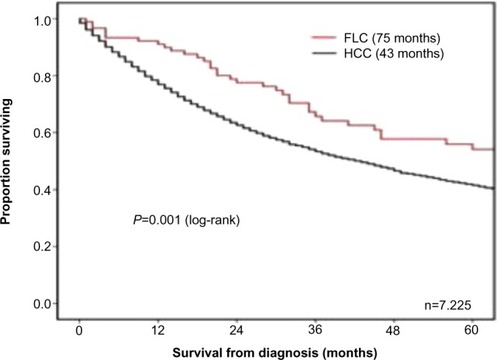
Table 1 Prognostic factors in fibrolamellar carcinoma
Despite a generally good long-term prognosis, recurrence following resection of FLC is relatively common with rates ranging from 33% to 100% and a median recurrence-free survival of 20–48 months.Citation6,Citation72 For example, in a small series of 28 patients who underwent resection of FLC, Stipa et al reported a 5-year recurrence-free survival of only 18% with an overall recurrence rate of 60%.Citation6 The most common sites of recurrence include lymph nodes, liver, peritoneum, lungs, and bone.Citation73 Due to the high recurrence associated with FLC, diligent postoperative surveillance is indicated. For example, Maniaci et al have proposed an intensive surveillance protocol following surgery that includes CT and serum vitamin B12-binding protein levels every 3–6 months for the first 2–3 years postoperatively.Citation54 In cases where serum vitamin B12-binding protein is elevated and CT scan is negative, the authors recommend PET/CT.Citation54 While this or other protocols have not been vigorously studied – and therefore cannot be endorsed – the data collectively suggest that close surveillance is warranted. If recurrence is detected, depending on the site and number of recurrent lesions, repeat surgical resection should be considered, as other treatment options are not effective. For example, Maniaci et al reported on ten patients with FLC treated with resection followed by close surveillance and re-excision, systemic chemotherapy, as well as radiotherapy for any relapses. This study showed a median overall survival of 9.3 years (95% confidence interval, 3.0–18.5) with two patients showing at least partial response to cisplatin and fluorouracil.Citation54
For patients with FLC who present with unresectable disease, liver transplantation should be considered as 3-year survival following 75%–80% transplantation approaches.Citation74 While transplantation may be used in cases of FLR, it is much more commonly indicated for HCC than FLC.Citation70 This is likely due to the fact HCC is more common than FLC as well as the fact that regional lymph node metastasis (a relative contraindication to transplant) is more common in FLC (42.2%) compared with HCC (22.2%).Citation70
Systemic therapy
FLC is not typically responsive to chemotherapy. While there is no consensus regarding the ideal chemotherapeutic regimen for FLC, platinum-based chemotherapy regimens, as well as combination regimens including interferon alpha-2b have been used with some success.Citation54,Citation75,Citation76 In a Phase II trial, Patt et al reported a complete or partial response in five out of eight patients treated with a combination therapy of fluorouracil and recombinant interferon alpha-2b.Citation75,Citation76 Recent case reports have described the use of gemcitabine/oxaliplatin and 5-FU/folinic acid/oxaliplatin with some success.Citation77–Citation79
In addition to systemic chemotherapy, recent research has focused on taking advantage of the new understanding of the pathogenesis and molecular genetics of FLC. For example, one current multi-institutional, randomized controlled trial is evaluating mTOR inhibition in combination with estrogen suppression in the treatment of FLC.Citation80 In addition, FLC has been shown to express increased levels of epithelial growth factor receptor as well as transforming growth factor beta.Citation81 Thus, these two factors are potential targets in the future treatment of FLC.
Locoregional therapy
As FLC is not typically responsive to systemic chemotherapy, locoregional therapies have been considered. While not well studied, radiation therapy has been used to treat recurrent FLC in a few small case series. In one case report, Peacock et al demonstrated an 85% decrease in tumor volume of FLC metastases using 40 Gy in ten fractions over a 13-day time period.Citation82 External beam radiation therapy was delivered as 21 Gy to the involved field in seven fractions over 10 days for most patients. In a separate retrospective study of ten patients with nonresectable metastatic disease who were treated with external beam radiation in addition to chemotherapy, three patients had objective partial responses by volumetric analysis, six patients had stabilization of their tumor volume, and one patient had early progression.Citation83 While regional liver-directed therapies (eg, chemoembolization, yttrium 90, ablation) have been well described for HCC, their use in FLC remains poorly defined.
Conclusion
FLC has a distinct epidemiology, radiographic appearance, as well as pathologic characteristic than HCC. Most often, patients who present with FLC have an absence of common risk factors seen in classic HCC. While physical findings are often not helpful, cross-sectional imaging with CT or MRI will typically display features highly suggestive of FLC. For patients with resectable disease, surgical resection with lymphadenectomy is the recommended treatment. The long-term prognosis for patients with resected FLC is good; however, many patients will experience a recurrence. A subset of patients who recur may be candidates for surgery. For patients who present with initially unresectable disease or develop an unresectable recurrence, other therapeutic options including systemic or locoregional therapy should be considered. Unfortunately, nonsurgical options for patients with FLC remain limited, and future research is needed to identify better multimodality therapies.
Disclosure
The authors report no conflicts of interest in this work.
References
- National Cancer Institute D SRPCancer Statistics BranchSurveillance, Epidemiology, and End Results (SEER) Program2015 Available from: http://www.seer.cancer.gov
- EdmondsonHADifferential diagnosis of tumors and tumor-like lesions of liver in infancy and childhoodAMA J Dis Child195691216818613282629
- CraigJRPetersRLEdmondsonHAOmataMFibrolamellar carcinoma of the liver: a tumor of adolescents and young adults with distinctive clinico-pathologic featuresCancer19804623723796248194
- BosmanFTWorld Health OrganizationInternational Agency for Research on CancerWHO Classification of Tumours of the Digestive System4th edLyonInternational Agency for Research on Cancer2010
- El-SeragHBDavilaJAIs fibrolamellar carcinoma different from hepatocellular carcinoma? A US population-based studyHepatology200439379880314999699
- StipaFYoonSSLiauKHOutcome of patients with fibrolamellar hepatocellular carcinomaCancer200610661331133816475212
- BermanMMLibbeyNPFosterJHHepatocellular carcinoma. Polygonal cell type with fibrous stroma – an atypical variant with a favorable prognosisCancer1980466144814556251961
- Arista-NasrJGutierrez-VillalobosLNuncioJMaldonaldoHBornstein-QuevedoLFibrolamellar hepatocellular carcinoma in Mexican patientsPathol Oncol Res20028213313712172578
- BismuthHChicheLCastaingDSurgical treatment of hepatocellular carcinomas in noncirrhotic liver: experience with 68 liver resectionsWorld J Surg199519135417740808
- HemmingAWLangerBSheinerPGreigPDTaylorBRAggressive surgical management of fibrolamellar hepatocellular carcinomaJ Gastrointest Surg1997143423469834368
- MooreSWDavidsonAHadleyGPMalignant liver tumors in South African children: a national auditWorld J Surg20083271389139518305988
- Moreno-LunaLEArrietaOGarcía-LeivaJClinical and pathologic factors associated with survival in young adult patients with fibrolamellar hepatocarcinomaBMC Cancer2005514216259635
- PinnaADIwatsukiSLeeRGTreatment of fibrolamellar hepatoma with subtotal hepatectomy or transplantationHepatology19972648778839328308
- StevensWRJohnsonCDStephensDHNagorneyDMFibrolamellar hepatocellular carcinoma: stage at presentation and results of aggressive surgical managementAm J Roentgenol19951645115311587717223
- TeitelbaumDHTuttleSCareyLCClausenKPFibrolamellar carcinoma of the liver. Review of three cases and the presentation of a characteristic set of tumor markers defining this tumorAnn Surg1985202136412409935
- KaczynskiJGustavssonBHanssonGWallerstedtSFibrolamellar hepatic carcinoma in an area with a low incidence of primary liver cancer: a retrospective studyEur J Surg199616253673718781917
- SooklimKSriplungHPiratvisuthTHistologic subtypes of hepatocellular carcinoma in the southern Thai populationAsian Pac J Cancer Prev20034430230614728587
- Al-MathamKAlabedIZaidiSZQushmaqKACold agglutinin disease in fibrolamellar hepatocellular carcinoma: a rare association with a rare cancer variantAnn Saudi Med201131219720021293066
- DadkeDJaganathPKrishnamurthySChiplunkarSThe detection of HBV antigens and HBx-transcripts in an Indian fibrolamellar carcinoma patient: a case studyLiver2002221879111906624
- HaratakeJHorieALeeSDHuhMHFibrolamellar carcinoma of the liver in a middle-aged Korean manJ UOEH19901233493542173092
- HoshinoHKatadaNNishimuraDCase report: fibrolamellar hepatocellular carcinoma in a Japanese woman: a case report and review of Japanese casesJ Gastroenterol Hepatol19961165515558792309
- ParadinasFJMeliaWMWilkinsonMLHigh serum vitamin B12 binding capacity as a marker of the fibrolamellar variant of hepatocellular carcinomaBr Med J198228563458408426288165
- ThirabanjasakDSosothikulDMahayosnondAThornerPSFibrolamellar carcinoma presenting as a pancreatic mass: case report and review of the literatureJ Pediatr Hematol Oncol200931537037219415023
- YenJBChangKWFibrolamellar hepatocellular carcinoma-report of a caseChang Gung Med J200932333633919527614
- YuanCYYuanCCShiouGFTsengCHYauMTFibrolamellar variant of hepatocellular carcinoma – report of a Chinese patientHepatogastroenterology19954221821847672769
- VaideeswarPPanditMJDeshpandeJRSivaramanAVoraIMFibrolamellar carcinoma of the liver – an unusual presentationJ Postgrad Med19933931591618051651
- AlbaughJSKeeffeEBKrippaehneWWRecurrent obstructive jaundice caused by fibrolamellar hepatocellular carcinomaDig Dis Sci19842987627676086253
- EcksteinRPBambachCPStielDRocheJGoodmanBNFibrolamellar carcinoma as a cause of bile duct obstructionPathology19882043263312853861
- SoyerPRocheALevesqueMFibrolamellar hepatocellular carcinoma presenting with obstructive jaundice. A report of two casesEur J Radiol19911331961981661675
- McCloskeyJJGermain-LeeELPermanJAPlotnickLPJanoskiAHGynecomastia as a presenting sign of fibrolamellar carcinoma of the liverPediatrics19888233793822841641
- AthanasakisEMouloudiEPrinianakisGKostakiMTzardiMGeorgopoulosDMetastatic liver disease and fulminant hepatic failure: presentation of a case and review of the literatureEur J Gastroenterol Hepatol200315111235124014560159
- MyszorMFRecordCOPrimary and secondary malignant disease of the liver and fulminant hepatic failureJ Clin Gastroenterol19901244414462204655
- SoreideOCzerniakABradpieceHBloomSBlumgartLCharacteristics of fibrolamellar hepatocellular carcinoma. A study of nine cases and a review of the literatureAm J Surg198615145185232421594
- MarrannesJGryspeerdtSHaspeslaghMvan HolsbeeckBBaekelandtMLeferePFibrolamellar hepatocellular carcinoma in a 65-year-old woman: CT featuresJBR-BTR200588523724016302333
- SethiSTagejaNSinghJHyperammonemic encephalopathy: a rare presentation of fibrolamellar hepatocellular carcinomaAm J Med Sci2009338652252420010160
- MansouriDVan NhieuJTCouanetDFibrolamellar hepatocellular carcinoma: a case report with cytological features in a sixteen-year-old girlDiagn Cytopathol200634856857116850484
- TanakaJBabaNAriiSTypical fibrolamellar hepatocellular carcinoma in Japanese patients: report of two casesSurg Today19942454594638054819
- GuptaPDharSStricklandNHFibrolamellar carcinoma: an unusual clinico-radiological presentationEur J Radiol199932211912310628420
- TangkijvanichPThong-NgamDKullavanijayaPSuwangoolPFibrolamellar hepatocellular carcinoma in a Thai man who presented with hypoglycemia: case report and review of literatureJ Med Assoc Thai200083780981610932518
- DahanMHKastellPFibrolamellar hepatic carcinoma with a presentation similar to that of septic pregnancy. A case reportJ Reprod Med2002471474911838311
- TorbensonMFibrolamellar carcinoma: 2012 updateScientifica2012201274379024278737
- LloretaJVadellCFabregatXSerranoSFibrolamellar hepatic tumor with neurosecretory features and systemic deposition of AA amyloidUltrastruct Pathol1994181–22872928191640
- WardSCHuangJTickooSKThungSNLadanyiMKlimstraDSFibrolamellar carcinoma of the liver exhibits immunohistochemical evidence of both hepatocyte and bile duct differentiationMod Pathol20102391180119020495535
- FrémontSChampigneulleBGérardPBlood transcobalamin levels in malignant hepatomaTumour Biol19911263533591724707
- LildballeDLNguyenKQPoulsenSSNielsenHONexoEHaptocorrin as marker of disease progression in fibrolamellar hepatocellular carcinomaEur J Surg Oncol2011371727921111562
- WheelerKPritchardJLuckWRossiterMTranscobalamin I as a “marker” for fibrolamellar hepatomaMed Pediatr Oncol19861442272293018464
- KanaiTTakabayashiTKawanoYKuramochiSMiyazawaNA case of postoperative recurrence of fibrolamellar hepatocellular carcinoma with increased vitamin B12 binding capacity in a young Japanese femaleJpn J Clin Oncol200434634635115333688
- CollierNAWeinbrenKBloomSRLeeYCHodgsonHJBlumgartLHNeurotensin secretion by fibrolamellar carcinoma of the liverLancet1984183765385406199633
- FriedmanACLichtensteinJEGoodmanZFishmanEKSiegelmanSSDachmanAHFibrolamellar hepatocellular carcinomaRadiology198515735835872997835
- GaneshanDSzklarukJKundraVKasebARashidAElsayesKMImaging features of fibrolamellar hepatocellular carcinomaAm J Roentgenol2014202354455224555590
- IchikawaTFederleMPGrazioliLMadariagaJNalesnikMMarshWFibrolamellar hepatocellular carcinoma: imaging and pathologic findings in 31 recent casesRadiology1999213235236110551212
- BlacharAFederleMPFerrisJVRadiologists’ performance in the diagnosis of liver tumors with central scars by using specific CT criteriaRadiology2002223253253911997564
- LiuSWah ChanKTongJWangYWangBQiaoLPET-CT scan is a valuable modality in the diagnosis of fibrolamellar hepatocellular carcinoma: a case report and a summary of recent literatureQJM2011104647748321493692
- ManiaciVDavidsonBRRollesKFibrolamellar hepatocellular carcinoma: prolonged survival with multimodality therapyEur J Surg Oncol200935661762119144491
- IchikawaTFederleMPGrazioliLMarshWFibrolamellar hepatocellular carcinoma: pre- and posttherapy evaluation with CT and MR imagingRadiology2000217114515111012437
- LiuSChanKWWangBQiaoLFibrolamellar hepatocellular carcinomaAm J Gastroenterol20091041026172624 quiz 262519638962
- Perez-GuillermoMMasgrauNAGarcia-SolanoJSola-PerezJde Agustin y de AgustinPCytologic aspect of fibrolamellar hepatocellular carcinoma in fine-needle aspiratesDiagn Cytopathol199921318018710450103
- BermanMABurnhamJASheahanDGFibrolamellar carcinoma of the liver: an immunohistochemical study of nineteen cases and a review of the literatureHum Pathol19881977847942456977
- WardSCWaxmanSFibrolamellar carcinoma: a review with focus on genetics and comparison to other malignant primary liver tumorsSemin Liver Dis2011311617021344351
- ZenaliMJTanDLiWDhingraSBrownREStemness characteristics of fibrolamellar hepatocellular carcinoma: immunohistochemical analysis with comparisons to conventional hepatocellular carcinomaAnn Clin Lab Sci201040212613420421623
- OrsattiGHytiroglouPThungSNIshakKGParonettoFLamellar fibrosis in the fibrolamellar variant of hepatocellular carcinoma: a role for transforming growth factor betaLiver19971731521569249730
- HoneymanJNSimonEPRobineNDetection of a recurrent DNAJB1-PRKACA chimeric transcript in fibrolamellar hepatocellular carcinomaScience201434361741010101424578576
- DarcyDGChiaroni-ClarkeRMurphyJMThe genomic landscape of fibrolamellar hepatocellular carcinoma: whole genome sequencing of ten patientsOncotarget20156275577025605237
- MavrosMNMayoSCHyderOPawlikTMA systematic review: treatment and prognosis of patients with fibrolamellar hepatocellular carcinomaJ Am Coll Surg2012215682083022981432
- DarcyDGMalekMMKobosRKlimstraDSDeMatteoRLa QuagliaMPPrognostic factors in fibrolamellar hepatocellular carcinoma in young peopleJ Pediatr Surg201550115315625598114
- McAteerJPGoldinABHealeyPJGowKWHepatocellular carcinoma in children: epidemiology and the impact of regional lymphadenectomy on surgical outcomesJ Pediatr Surg201348112194220124210185
- AminiNEjazASpolveratoGMaithelSKKimYPawlikTMManagement of lymph nodes during resection of hepatocellular carcinoma and intrahepatic cholangiocarcinoma: a systematic reviewJ Gastrointest Surg201418122136214825300798
- AngCSKelleyRKChotiMAClinicopathologic characteristics and survival outcomes of patients with fibrolamellar carcinoma: data from the fibrolamellar carcinoma consortiumGastrointest Cancer Res2013613923505572
- KasebAOShamaMSahinIHPrognostic indicators and treatment outcome in 94 cases of fibrolamellar hepatocellular carcinomaOncology201385419720324051705
- MayoSCMavrosMNNathanHTreatment and prognosis of patients with fibrolamellar hepatocellular carcinoma: a national perspectiveJ Am Coll Surg2014218219620524315886
- KatzensteinHMKrailoMDMalogolowkinMHFibrolamellar hepatocellular carcinoma in children and adolescentsCancer20039782006201212673731
- GroeschlRTMiuraJTWongRKMulti-institutional analysis of recurrence and survival after hepatectomy for fibrolamellar carcinomaJ Surg Oncol2014110441241524844420
- WojcickiMLubikowskiJPostMChmurowiczTWiechowska-KozlowskaAKrawczykMAggressive surgical management of recurrent lymph node and pancreatic head metastases of resected fibrolamellar hepatocellular carcinoma: a case reportJOP201213552953222964960
- El-GazzazGWongWEl-HadaryMKOutcome of liver resection and transplantation for fibrolamellar hepatocellular carcinomaTrans Int200013Suppl 1S406S409
- BowerMNewlandsESHabibNFibrolamellar hepatocellular carcinoma responsive to platinum-based combination chemotherapyClin Oncol199685331333
- PattYZHassanMMLozanoRDPhase II trial of systemic continuous fluorouracil and subcutaneous recombinant interferon Alfa-2b for treatment of hepatocellular carcinomaJ Clin Oncol200321342142712560429
- FonsecaGMVarellaADCoelhoFFAbeESDumarcoRBHermanPDownstaging and resection after neoadjuvant therapy for fibrolamellar hepatocellular carcinomaWorld J Gastrointest Surg20146610711124976904
- FakihMA case of fibrolamellar cancer with a palliative response and minor radiographic regression with erlotinib and bevacizumab combination therapyAm J Ther2014216e207e21023676344
- GrasPTruantSBoigeVProlonged Complete Response after GEMOX Chemotherapy in a Patient with Advanced Fibrolamellar Hepatocellular CarcinomaCase Rep Oncol20125116917222666208
- RiehleKJYehMMYuJJmTORC1 and FGFR1 signaling in fibrolamellar hepatocellular carcinomaMod Pathol201528110311024925055
- BuckleyAFBurgartLJKakarSEpidermal growth factor receptor expression and gene copy number in fibrolamellar hepatocellular carcinomaHum Pathol200637441041416564914
- PeacockJGCallJAOlivierKRRadiotherapy for metastatic fibrolamellar hepatocellular carcinomaRare Tumors201353e2824179640
- EpsteinBEPajakTFHaulkTLHerpstJMOrderSEAbramsRAMetastatic nonresectable fibrolamellar hepatoma: prognostic features and natural historyAm J Clin Oncol1999221222810025374
