Abstract
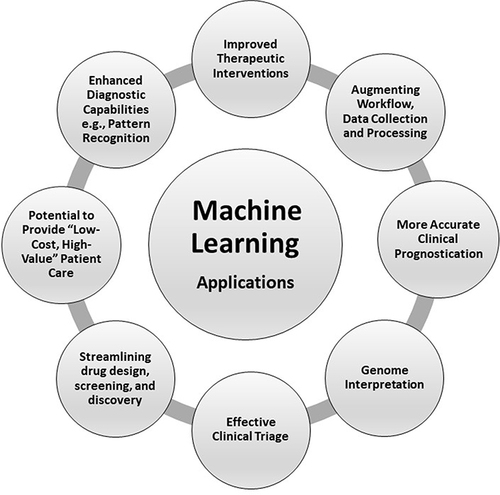
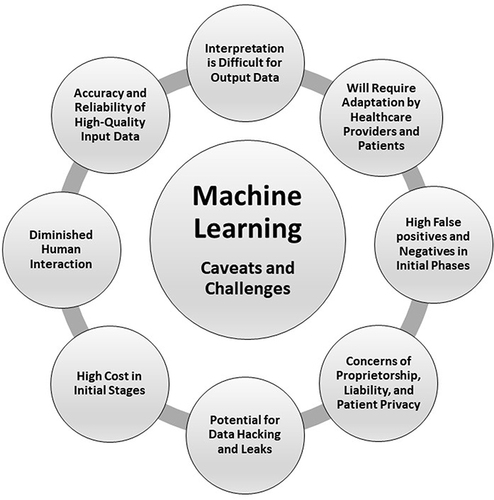
Artificial Intelligence (AI) and Machine Learning (ML) promise to transform all facets of medicine. Expected changes include more effective clinical triage, enhanced accuracy of diagnostic interpretations, improved therapeutic interventions, augmented workflow algorithms, streamlined data collection and processing, more precise disease prognostication, newer pharmacotherapies, and ameliorated genome interpretation. However, many caveats remain. Reliability of input data, interpretation of output data, data proprietorship, consumer privacy, and liability issues due to potential for data breaches will all have to be addressed. Of equal concern will be decreased human interaction in clinical care, patient satisfaction, affordability, and skepticism regarding cost-benefit. This descriptive literature-based treatise expounds on the promise and provisos associated with the anticipated import of AI and ML into all domains of medicine and healthcare in the very near future.
Innovative scientific and technological developments have ushered in a remarkable transformation in medicine that continues to impact virtually all stakeholders from patients to providers to Healthcare Organizations (HCOs) and the community in general.Citation1,Citation2 Increasingly incorporated into clinical practice over the past few decades, these innovations include widespread use of Electronic Health Records (EHR), telemedicine, robotics, and decision support for surgical procedures. Ingestible microchips allow healthcare providers to monitor patient compliance with prescribed pharmacotherapies and their therapeutic efficacy through big data analysis,Citation1–5 as well as streamlining drug design, screening, and discovery.Citation6 Adoption of novel medical technologies has allowed US healthcare to maintain its vanguard position in select domains of clinical care such as improving access by reducing wait times, enriching patient-provider communication, enhancing diagnostic accuracy, improving patient satisfaction, augmenting outcome prediction, decreasing mortality, and extending life expectancy.Citation3–5,Citation7
Yet despite the theoretical advantages of these innovative medical technologies, many issues remain requiring careful consideration as we integrate these novel technologies into our armamentarium. This descriptive literature-based article explicates on the advantages, future potential, challenges, and caveats with the predictable and impending importation of AI and ML into all facets of healthcare.
Innovative Technological Advances and Applications
By far the most revolutionary of these novel technologies is Artificial Intelligence (AI), a branch of computer science that attempts to construct intelligent entities via Machine Learning (ML), which is the “ability of computers to learn without being explicitly programed”.Citation8 ML utilizes algorithms to identify patterns, and its subspecialty Deep Learning (DL) employs artificial neural networks with intervening frameworks to identify patterns and data.Citation1,Citation8 Although ML was first conceived by computer scientist Arthur Samuel as far back as 1956, applications of AI have only recently begun to pervade our daily life with computers simulating human cognition—eg, visual perception, speech recognition, decision-making, and language translation.Citation8 Everyday examples of AI include smart phones, autonomous vehicles, digital assistants (eg, Siri, Alexa), chatbots and auto-correcting software, online banking, facial recognition, and transportation (eg, Uber, air traffic control operations, etc.). The iterative nature of ML allows the machine to adapt its systems and outputs following exposure to new data with supervised learning—ie, utilizing training algorithms to predict future events from historical data inputs—or unsupervised learning, whereby the machine explores the data and attempts to develop patterns or structures de novo. The latter methodology is often used to determine and distinguish outliers. Neural networks in AI utilize an adaptive system comprised of an interconnected group of artificial neurons and mathematical or computational modeling for processing information from input and output data via pattern recognition.Citation9 Through predictive analytics, ML has demonstrated its effectiveness in the realm of finance (eg, identifying credit card fraud) and in the retail industry to anticipate customer behavior.Citation1,Citation10,Citation11
Extrapolation of AI to medicine and healthcare is expected to increase exponentially in the three principal domains of research, teaching, and clinical care. With improved computational efficiencies, common applications of ML in healthcare will include enhanced diagnostic modalities, improved therapeutic interventions, augmenting and refining workflow by processing large amounts of hospital and national EHR data, more accurate clinical course and prediction through precision and personalized medicine, and genome interpretation. ML can provide basic clinical triage in geographical areas inaccessible to specialty care. It can also detect treatable psychiatric conditions via analysis of affective and anxiety disorders using speech patterns and facial expressions (eg, bipolar disorder, major depression, anxiety spectrum and psychotic disorders, attention deficit hyperactivity disorder, addiction disorders, Tourette’s Syndrome, etc.)Citation12,Citation13 (). Deep learning algorithms are highly effective compared to human interpretation in medical subspecialties where pattern recognition plays a dominant role, such as dermatology, hematology, oncology, histopathology, ophthalmology, radiology (eg, programmed image analyses), and neurology (eg, analysis for seizures utilizing electroencephalography). Artificial neural networks are being developed and employed for diagnostic accuracy, timely interventions, outcomes and prognostication of neurosurgical conditions, such as spinal stenosis, traumatic brain injury, brain tumors, and cerebral vasospasm following aneurysmal subarachnoid hemorrhage.Citation14 Theoretically, ML can improve triage by directing patients to proper treatments at lower cost and by keeping those with chronic conditions out of costly and time-intensive emergency care centers. In clinical practice, ~5% of all patients account for 50% of healthcare costs, and those with chronic medical conditions comprise 85% of total US healthcare costs.Citation3
Patients can benefit from ML in other ways. For follow-up visits, not having to arrange transportation or take time off work for face-to-face interaction with healthcare providers may be an attractive alternative to patients and to the community, even more so in restricted circumstances like the recent COVID-19 pandemic-associated lockdowns and social distancing.
Ongoing ML-related research and its applications are robust. Companies developing automation, topological data analysis, genetic mapping, and communications systems include Pathway Genomics, Digital Reasoning Systems, Ayandi, Apixio, Butterfly Network, Benevolent AI, Flatiron Health, and several others.Citation1,Citation10
Caveats and Challenges
Despite the many theoretical advantages and potential benefits of ML in healthcare, several challenges () must be metCitation15 before it can achieve broader acceptance and application.
Data Acquisition and Validation
Frequent software updates will be necessary to ensure continued improvement in ML-assisted models over time. Encouraging the use of such software, the Food and Drug Administration has recommended a “pre-certified approach” for agility.Citation1,Citation2 To be of pragmatic clinical import, high-quality input-data is paramount for validating and refining diagnostic and therapeutic procedures. At present, however, there is a dearth of robust comparative data that can be validated against the commonly accepted gold standard, comprised of blinded, placebo-controlled randomized clinical trials versus the ML-output data that is typically an “area-under-the-curve” analysis.Citation1,Citation7 Clinical data generated from ML-assisted calculations and more rigorous multi-variate analysis will entail integration with other relevant patient demographic information (eg, socio-economic status, including values, social and cultural norms, faith and belief systems, social support structures in-situ, etc.).Citation16
Paradigm Shift in Patient Care
All stakeholders in the healthcare delivery system (HCOs, providers, patients, and the community) will have to adjust to the paradigm shift away from traditional in-person interactions. Healthcare providers will have to surmount actual or perceived added workload to avoid “burnout” especially during the initial adaptive phase. They will also have to cope with increased ML-generated false-positive and -negative alerts. The traditional practice of clinical medicine is deeply entrenched in the framework of formulating a clinical hypothesis via rigorous history-taking and physical examination followed by sequential confirmation through judicious ancillary and diagnostic testing. Such traditional in-person interactions have underscored the importance of an empathetic approach to the provider-patient relationship. This traditional view has been characterized as “archaic”, particularly by those with a “futuristic” mindset, who envision an evolutionary change leading to “whole body scans” that deliver a more accurate assessment of health and diagnosis of disease. However, incidental findings not attributable to symptoms may lead to excessive ancillary tests underscoring the adage “testing begets more testing”.Citation17
Cost-Benefit and Value Proposition
Healthcare is one of the fastest growing segments of the world economy and is presently at a crossroads of unprecedented transformation. As an example, US healthcare expenditure has accelerated dramatically over the past several decades (~19% of Gross National Product; exceeding $4.1 trillion, or $12,500 per person per year)Citation18 with widespread ramifications for all stakeholders including patients and their families, healthcare providers, government, community, and the US economy.Citation1,Citation3–5 A paradigm shift from “volume-based” to “performance-based” reimbursements from third-party payers warrants focus on some of the most urgent issues in healthcare including cost containment, access, and providing “low-cost, high-value” healthcare commensurate with the proposed six-domain framework (“safe, effective, patient-centered, timely, efficient, and equitable”) articulated by the Institute of Medicine in 2001.Citation3–5,Citation19 Of note, uncontrolled use of expensive technology and excessive ancillary testing account for ~25–30% of total healthcare costs.Citation17 While technologies will probably never completely replace the function of healthcare providers, they will definitely transform healthcare, benefiting both providers and patients. However, there is a paucity of cost–benefit data and analysis of the use of these innovative emerging medical technologies. All stakeholders should remain cost-conscious as the newer technological diagnostic approaches may further drive up the already rising costs of healthcare. Educating and training the next generation of healthcare providers in the context of AI will also require transformation with simulation approaches and inter-professional education. Therefore, the value proposition of novel technologies must be critically appraised via longitudinal and continuous valuations and patient outcomes in terms of its impact on health and disease management.Citation13 To mitigate healthcare costs, we must control the “technological imperative”—the overuse of technology because of easy availability without due consideration to disease course or outcomes and irrespective of cost–benefit ratio.Citation3
Data Ownership and Integrity
Issues surrounding consumer privacy and proprietorship of colossal quantities of healthcare data under an AI regime are legitimate concerns. Malicious or unintentional breaches may result in financial or other harm. Akin to the challenges encountered with EHR, easy access to data and interoperability with broader compatibility of interfaces by healthcare providers spread across space and time will present unique challenges. Databases will likely be owned by large profit-oriented technology companies who may decide to dispense data to third parties. Additional costs are predictable as well, particularly during the early stages of development of ML algorithms, which is likely to be more bearable to large HCOs. Delay in the use of such processes is anticipated by smaller organizations with resulting potential for mergers and acquisitions or even failure of smaller hospitals and clinics. Concerns regarding ownership, responsibility, and accountability of ML algorithms may arise owing to the probability of detrimental outcomes, which ideally should be apportioned between developer, interpreter, healthcare provider, and patient.Citation1 Simulation techniques can be preemptively utilized for ML training for clinical scenarios; practice runs may require formal certification courses and workshops. Regulations must be developed by policymakers and legislative bodies to delineate the role of third-party payers in ML-assisted healthcare financing. Finally, education and training via media outlets, internet, and social media will be necessary to address public opinion, misperceptions, and naïve expectations about ML-assisted algorithms.Citation7
Conclusions and Future Directions
For centuries, the practice of medicine has been deeply embedded in a tradition of meticulous history-taking, physical examination, and thoughtful ancillary investigations to confirm clinical hypotheses and diagnoses. The great physician, Sir William Osler (1849–1919)Citation14,Citation20 encapsulated the desired practice of good medicine with his famous quotes, “Listen to your patient – he is telling you the diagnosis”, “The good physician treats the disease; the great physician treats the patient who has the disease”, and “Medicine is a science of uncertainty and an art of probability”. With rapid technological advances, we are at the crossroads of practicing medicine that would be distinctly different from the traditional approach and practice(s), a change that may be characterized as “evolutionary”.
AI and ML have enormous potential to transform healthcare and the practice of medicine, although these modalities will never substitute an astute and empathetic bedside clinician. Furthermore, several issues remain as to whether their value proposition and cost-benefit are complementary to the overarching focus on providing “low-cost, high-value” healthcare to the community at large. While innovative technological advances play a critical role in the rapid diagnosis and management of disease, the phenomenon of the technological imperativeCitation3–5,Citation17 deserves special consideration among both public and providers for the future use of AI and ML in delivering healthcare.
Disclosure
The author reports no conflicts of interest in this work.
References
- Bhardwaj R, Nambiar AR, Dutta D A Study of Machine Learning in Healthcare. 2017 IEEE 41st Annual Computer Software and Applications Conference. 236–241. Available from: https://ieeexplore.ieee.org/stamp/stamp.jsp?arnumber=8029924. Accessed March 30, 2022.
- Deo RC. Machine Learning in Medicine. Circulation. 2015;132:1920–1930. doi:10.1161/CIRCULATIONAHA.115.001593
- Shi L, Singh DA. Delivering Health Care in America: A Systems Approach. 7th ed. Burlington, MA: Jones & Bartlett Learning; 2019.
- Barr DA. Introduction to US Health Policy. The Organization, Financing, and Delivery of Health Care in America. 4th ed. Baltimore, MD: John Hopkins University Press; 2016.
- Wilensky SE, Teitelbaum JB. Essentials of Health Policy and Law. Fourth ed. Burlington, MA: Jones & Bartlett Learning; 2020.
- Gupta R, Srivastava D, Sahu M, Tiwan S, Ambasta RK, Kumar P. Artificial intelligence to deep learning; machine intelligence approach for drug discovery. Mol Divers. 2021;25:1315–1360. doi:10.1007/s11030-021-10217-3
- Dabi A, Taylor AJ. Machine Learning, Ethics and Brain Death Concepts and Framework. Arch Neurol Neurol Disord. 2020;3:1–9.
- Handelman GS, Kok HK, Chandra RV, Razavi AH, Lee MJ, Asadi H. eDoctor: machine learning and the future of medicine. J Int Med. 2018;284:603–619. doi:10.1111/joim.12822
- Hopfield JJ. Neural networks and physical systems with emergent collective computational abilities. Proc Natl Acad Sci U S A. 1982;79:2554–2558. doi:10.1073/pnas.79.8.2554
- Ghassemi M, Naumann T, Schulam P, Beam AL, Ranganath R Opportunities in Machine Learning for Healthcare. 2018. Available from: https://pdfs.semanticscholar.org/1e0b/f0543d2f3def3e34c51bd40abb22a05937bc.pdf. Accessed March 30, 2022.
- Jnr YA Artificial Intelligence and Healthcare: a Qualitative Review of Recent Advances and Predictions for the Future. Available from: https://pimr.org.in/2019-vol7-issue-3/YawAnsongJnr_v3.pdf. Accessed March 30, 2022.
- Chandler C, Foltz PW, Elvevag B. Using machine learning in Psychiatry; the need to establish a Framework that nurtures trustworthiness. Schizophr Bull. 2019;46:11–14.
- Ray A, Bhardwaj A, Malik YK, Singh S, Gupta R. Artificial intelligence and Psychiatry: an overview. Asian J Psychiatr. 2022;70:103021. doi:10.1016/j.ajp.2022.103021
- Ganapathy K Artificial intelligence in neurosciences-are we really there? Available from: https://www.sciencedirect.com/science/article/pii/B9780323900379000084. Accessed June 10, 2022.
- Sunarti S, Rahman FF, Naufal M, Risky M, Febriyanto K, Mashina R. Artificial intelligence in healthcare: opportunities and risk for future. Gac Sinat. 2012;35(S1):S67–S70. doi:10.1016/j.gaceta.2020.12.019.
- Yu B, Beam A, Kohane I. Artificial Intelligence in Healthcare. Nature Biomed Eng. 2018;2:719–731. doi:10.1038/s41551-018-0305-z
- Bhardwaj A. Excessive Ancillary Testing by Healthcare Providers: reasons and Proposed Solutions. J Hospital Med Management. 2019;5(1):1–6.
- Fact Sheet NHE. Centers for Medicare and Medicaid Services. Available from: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NHE-Fact-Sheet. Accessed April 14, 2022.
- Institute of Medicine (IOM). Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C: National Academy Press; 2001.
- Bliss M. William Osler: A Life in Medicine. New York, NY: Oxford University Press; 1999.