Abstract
Studies examining post-traumatic stress disorder (PTSD) have either emphasized a relationship between PTSD and a systemically pro-inflammatory state or identified a link between PTSD and chronic disease. The aim of this study was to evaluate the evidence for a relationship between individuals with PTSD and systemic low-grade inflammation that has been proposed to underlie chronic disease development in this population. The authors conducted a systematic review of the literature (January 2006 to April 2017) in accordance with the PRISMA statement in the following four databases: PubMed, MEDLINE, PsycINFO, and SPORTDiscus with Full Text. The search strategy was limited to articles published in peer-reviewed journals and to human studies. Nine studies measuring systemic inflammation and discussing its role in chronic disease development were selected for inclusion in this review. The association between markers of systemic inflammation and PTSD was evaluated by the measurement of a variety of systemic inflammatory markers including acute-phase proteins, complement proteins, pro- and anti-inflammatory cytokines, natural killer cells, and white blood cells. In general, systemic inflammatory biomarkers were elevated across the studies in the PTSD groups. There is evidence that PTSD is underpinned by the presence of a systemic low-grade inflammatory state. This inflammation may be the mechanism associated with increased risk for chronic disease in the PTSD population. From this, future research should focus on interventions that help to reduce inflammation, such as exercise.
Introduction
Post-traumatic stress disorder (PTSD) is a debilitating psychiatric condition that manifests after experiencing trauma. Defined as an Axis I disorder in the Diagnostic and Statistical Manual of Mental Disorders, fifth edition, PTSD is characterized by a number of symptoms such as re-experiencing the traumatic event, avoidance of reminders of the traumatic event, negative changes in mood and cognitions, and hyperarousal.Citation1,Citation2 These symptoms must persist and cause marked distress and/or functional impairment for at least one month.Citation1 The lifetime prevalence rate for PTSD is estimated to be 8%, making it the fourth most commonly diagnosed psychiatric disorder, with 12% and 18% of US soldiers suffering from PTSD upon their return from Afghanistan and Iraq, respectively.Citation3,Citation4 Similarly, among Australian war veterans, PTSD is the most commonly diagnosed mental health disorder, with a prevalence of 8.1% in Australian male soldiers.Citation5
PTSD places a significant burden on the individual, his or her family, and society at large, as not only is it associated with multiple negative social consequences such as marital difficulties and unemployment but also it seems to be correlated with an increased risk of developing chronic somatic diseases such as cardiovascular disease (CVD), metabolic syndrome, pulmonary disease, autoimmune disorders, and other psychiatric disorders that are often associated with PTSD.Citation2,Citation6–Citation8 Notably, low-grade systemic inflammation is seen as a key mechanism underlying chronic disease and may be present too in PTSD, leading to the development of chronic diseases in this population.Citation2,Citation9
The underlying psychobiological mechanisms linking PTSD to an increased chronic disease risk have been proposed to be altered autonomic nervous system (ANS) activity and an impaired reaction of the hypothalamic–pituitary–adrenal (HPA) axis to perceived stress, resulting in a chronic low-grade pro-inflammatory state.Citation10 In the context of a chronically hyperaroused state (as seen in individuals suffering from PTSD), the ANS has been shown to display an inappropriate response characterized by a delay in parasympathetic nervous system (PNS) reactivation and sympathetic nervous system (SNS) domination continuing long after the stressful event has dissipated.Citation11 The consequence of prolonged autonomic reactivity in PTSD patients may center around the bi-directional relationship between the ANS and HPA axis, as represented by vagal activity.Citation2 Considering that a function of the vagus nerve is to regulate the immune system, an attenuated vagal response would fail to re-establish PNS dominance at rest. This, in turn, may compromise the normal immune profile, exacerbating the risk for chronic disease.Citation2 In addition, the dysregulated HPA axis may contribute to a chronic low-grade inflammatory state due to alterations within the glucocorticoid (GC) receptor itself and reduced GC signaling. Changes to GC responsiveness may also contribute to allostatic load, resulting in chronic disease development.Citation12
Dantzer and colleaguesCitation13 proposed that systemic low-grade inflammation is typically defined by a two- to threefold increase in plasma concentrations of pro-inflammatory cytokines, such as interleukin (IL)-1, tumor necrosis factor-α (TNF-α), and IL-6.Citation14,Citation15 However, the origin of this low-grade inflammation remains unclear. Neigh and AliCitation16 proposed that PTSD leads to a pro-inflammatory state as a consequence of the dysregulations in the aforementioned ANS and HPA axis biological pathways, thereby increasing physical disease risk. Conversely, Walker et alCitation17 suggested an alternative hypothesis for developing PTSD, emphasizing that chronic occupational exposures such as physical exhaustion, smoke, heat exposure, and sleep restriction (mainly experienced by military veterans and first responders who regularly encounter traumatic events) may have a “priming” inflammatory effect for the later development of PTSD, ultimately leading to chronic somatic illness.
However, this proposed state of low-grade inflammation characteristic of both PTSD and chronic disease is not always indicated. While various studies have demonstrated elevations in inflammatory markers in PTSD sufferers, others have presented opposing findings.Citation6,Citation18–Citation25 In light of these discrepancies, the aim of this systematic review was to assess the research that examines the association between PTSD and low-grade systemic inflammation.
Material and methods
This systematic review was conducted in accordance with the established guidelines from the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement.Citation26,Citation27
Search strategy
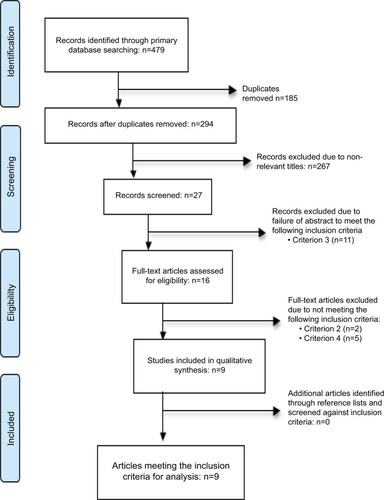
An electronic literature search of peer-reviewed journal articles was conducted using four databases: PubMed, MEDLINE, PsycINFO, and SPORTDiscus. Medical Subject Headings (MeSH) were considered in the development of the search terms. The search was limited to the English language and to human studies. Studies from before 2006 were excluded. The lead author screened titles, abstracts, and methods for relevance based on the selection criteria, and all duplicates were removed. Those articles deemed relevant were selected for further consideration (). The search was further limited to peer-reviewed original research articles with full text available. Reviews, meta-analyses, and other types of paper (e.g. author manuscripts, letters to the editor) were excluded. A hand search was undertaken of the reference lists of relevant articles, and those deemed eligible were included with the intent to ensure that all articles relevant to the research had been captured by the search strategy. The abstracts of the articles deemed relevant by the lead author were then independently reviewed by a second investigator for relevance. If consensus was not reached, the article was moved on to the next stage for a review of the full text. The full texts of the remaining eligible studies were independently reviewed by the investigators against the inclusion and exclusion criteria. Disagreements were discussed until consensus was reached in all cases.
Search terminology
The search terms used included: “post-traumatic stress disorder” OR “PTSD,” AND “cardiovascular disease” OR “CVD” OR “physical health” OR “metabolic disease” OR “immune system” OR “inflammation” OR “C-reactive protein” OR “CRP” OR “cytokines” OR “leukocytes” OR “white blood cells” OR “WBC” OR “acute phase proteins” OR “complement” OR “innate immunity” OR “hypothalamic pituitary adrenal axis” OR “HPA axis.” These were combined using the Boolean operators as stated above.
Selection criteria and data extraction
Studies were eligible for inclusion if the following applied: (1) they examined trauma leading to PTSD; (2) they examined the relationship between PTSD, inflammation, and chronic disease risk; (3) they had a correlational or longitudinal design (observational, randomized trials); (4) they had a control group; and (5) they measured at least one systemic inflammatory biomarker.
All papers identified from the initial electronic search process were imported into EndNote (version X7; Thomson Reuters), where all duplicates were removed. Upon completion of the title and abstract reviews, a total of 16 articles were identified for full-text review, of which nine were identified as meeting the inclusion criteria. The reasons for excluding each article were recorded.
Data analysis
After study selection, criteria were followed to maintain the evaluation of the studies within narrow standards. The first and essential criterion was that all details regarding inflammatory marker collection should be verified, with description of the instruments, data collection protocol, and methods.
Data extraction of included studies was completed by two independent reviewers and compiled into a table. This included the following: author and year of publication, number of participants, study design, focus of the study, the inflammatory markers tested, and the statistical significance of study findings.
Risk of bias
Two independent authors used the Physiotherapy Evidence Database (PEDro) scale to assess the quality and risk of bias of each of the studies identified as eligible (). The PEDro scale has proven constructive validity.Citation28 It is an 11-item scale that is used to assess the quality of the methodology in studies.Citation29,Citation30 The PEDro scale measures/ assesses the eligibility criteria, randomization, allocation processes, similarity of baseline groups, blinding process, near-complete data sets obtained for the key outcome, between-group statistics reported, and measures of variability in the selected studies.Citation29 Criterion 1 is used to help determine the external validity of the study; criteria 2–9 are designed to help identify whether the study has internal validity; and criteria 10 and 11 assist in determining whether there is sufficient statistical information for the results to be interpreted appropriately.Citation29 Each of these items was allocated a score in relation to the study. A point was allocated if the study met the specified criterion and a zero was awarded when the item did not. A total score of bias for the study was then calculated by adding all of the items together. The risk of bias for the studies was established using the criteria from the PEDro scale, summating items 2–4 and 7–9. The six criteria that were used in the current review were: (i) adequacy of randomization (criterion 2); (ii) allocation concealment (criterion 3); (iii) between-group baseline comparability (criterion 4); (iv) blinding of outcome assessors (criterion 7); (v) adequate follow-up (more than 85%) (criterion 8); and (vi) intention-to-treat analysis (criterion 9). A score of 5 or 6 was considered to have a low risk of bias, 3 or 4 a moderate risk, and 2 or less a high risk.
Table 1 PEDro scale outcomes
Results
Study design and characteristics
In total, 479 records were screened, after the data had been filtered and duplicates removed. From these, nine studies were identified as meeting the inclusion criteria (). All of the selected studies were of a cross-sectional design. Data are presented in with a description of the studies (including population and design) according to their focus relating inflammation to chronic physical disease in PTSD sufferers, the variables that were tested (inflammatory markers) and the significant statistical findings.
Table 2 Representation of selected articles examining the relationship between PTSD and systemic low-grade inflammation
The purpose of all included studies was to investigate the systemic inflammatory status of individuals affected by PTSD.
Populations assessed
The PTSD populations included in the nine studies included in this analysis comprised military veterans and individuals who had experienced traumatic accidents or interpersonal violence such as physical and sexual assault, although one article did not specify the source of trauma.Citation6,Citation18–Citation25 Some studies included only male subjects, whereas most consisted of males and females, and only one included just females.Citation6,Citation18–Citation25 All studies included in this review evaluated various cytokines to portray the inflammatory state of the PTSD group against that of the control group. Out of these nine studies, all but one demonstrated a statistically significant (p≤0.05) difference in at least one inflammatory marker in the PTSD compared to the control group, with the PTSD population displaying an elevated level of pro-inflammatory cytokines, acute-phase proteins, and/or white blood cells.Citation25 The research conducted by Gola and co-workersCitation25 did not reveal statistically significant intergroup differences in basal concentrations of IL-6, IL-8, IL-10, TNF-α, or monocyte chemoattractant protein-1 (MCP-1).
Control for confounding factors
Through the inclusion and exclusion criteria and statistical analyses, the reviewed studies controlled for the following confounding factors that have known implications on the validity of inflammatory marker results: age,Citation6,Citation18–Citation24 gender,Citation6,Citation18–Citation25 psychiatric co-morbidities,Citation6,Citation18–Citation21,Citation23,Citation25 medication,Citation6,Citation19,Citation21–Citation25 asthma/allergies,Citation6,Citation23 ethnicity,Citation6,Citation19–Citation21,Citation23,Citation25 education,Citation6,Citation19,Citation20,Citation23 length of time since trauma,Citation6,Citation18,Citation19,Citation23 body mass index (BMI),Citation6,Citation18–Citation21,Citation23,Citation24 type of trauma,Citation6,Citation19,Citation23,Citation25 alcohol/substance abuse,Citation18,Citation19,Citation24,Citation25 smoking status,Citation6,Citation18,Citation19,Citation21,Citation23–Citation25 physical activity,Citation18,Citation24 employment,Citation20 physical disease,Citation6,Citation18,Citation19,Citation22–Citation25 marital status,Citation20 and early life trauma.Citation6,Citation23
Definitions of low-grade inflammation
All studies included in this review conducted research investigating the association between PTSD and an increased chronic disease risk. Each study aimed to provide physiological evidence for this relationship by measuring biological inflammatory markers of individuals suffering from PTSD versus a control group. However, only three out of nine studies clearly defined low-grade inflammation (C-reactive protein [CRP] >3 mg/L; 3 standard deviations > mean value of IL-6, IL-8, IL-10, TNF-α, and MCP-1).Citation6,Citation24,Citation25 All of the included studies compared between-group inflammatory cytokine levels, acute-phase proteins, and/ or white blood cells, and tested for statistical significance (p≤0.05).
Discussion
Normal physiological responses to stress are disrupted in individuals suffering from PTSD, as evidenced by an altered response from the ANS (attenuation of vagal tone resulting in a delayed reactivation of the PNS and sympathetic tone domination) and an impaired HPA axis reaction to ongoing stress (inhibition of the HPA axis negative feedback loop involving cortisol).Citation16 Dennis and co-workersCitation2 emphasized that the synchronicity underlying the suggested interaction between these two systems is vital to maintaining healthy adaptive physiological functioning. Disruptions in these biological pathways (as noted in PTSD-affected people) appear to have downstream effects on other bodily systems such as the immune system, as illustrated by chronic low-grade inflammation, which may ultimately lead to a higher risk of developing a number of physical diseases.Citation16,Citation31
While research has identified the possible biological mechanistic impairments that seem to be characteristic of PTSD, disagreements remain regarding the potential catalysts for developing PTSD. Specifically, it has not been established whether an individual is “primed” to develop PTSD through an already existing pro-inflammatory state or if chronic low-grade inflammation manifests after the development of PTSD.Citation17,Citation32 Furthermore, there are discrepancies between previous studies’ findings of various inflammatory markers compared to a control group. However, while these inconsistencies are apparent, it is inarguable that there is a significant association between PTSD, inflammation, and declining physical health.
In addition to the altered levels of inflammatory markers in PTSD sufferers compared to their non-PTSD counterparts, all reviewed studies identified a clear risk and prevalence of physical co-morbidities of the participants with PTSD. Moreover, these studies interpreted chronic inflammation (measured through acute-phase proteins such as CRP and complement proteins, pro- and anti-inflammatory cytokine levels, innate immune cells, and/or white blood cells) as the link tying PTSD to chronic disease risk, with CVD having the highest prevalence compared to other chronic diseases in this population.Citation33 Furthermore, all investigators cited an urgent need for the development of interventions that address inflammation and chronic disease in PTSD, as its physical comorbidities reduce life expectancy by 10–17 years.Citation34
Given the importance of improving the debilitating co-morbid chronic physical health conditions of PTSD, this review contributed by investigating the evidence for systemic inflammation in PTSD to substantiate the proposed link between PTSD and chronic disease. Despite the majority of the studies demonstrating significant between-group differences in inflammatory markers, these findings were not unanimous. In addition, there was a limited number of studies that met the criteria for this review, all of a cross-sectional design, and they were not without multiple confounders. Out of the nine studies included in this review, one had a relatively small (n=28) sample size and all studies had either a moderate or high risk of bias according to the PEDro scale.Citation18 Furthermore, there were clear differences in the populations comprising the control groups between studies. Some studies controlled for trauma exposure in both groups, while the non-PTSD groups in the remaining studies included participants who had no trauma record whatsoever.Citation6,Citation18–Citation25 As a consequence, regarding the studies that did not have a trauma-exposed control group, the notion that trauma exposure is the factor affecting inflammation cannot be dismissed.Citation18 Similarly, only three studies took into account timing of exposure to the trauma and none of the studies investigated the possible effect of the duration of participants’ PTSD status on systemic inflammation.Citation6,Citation22,Citation23 Having said that, one of the reviewed studies measured the effect of repeated exposure to trauma on inflammation in PTSD participants and concluded that the number of traumatic exposures was directly proportional to systemic inflammation.Citation25
As there is a multitude of variables to account for in psychoneuroimmunological research, this review recognizes that demonstrating psychobiological relationships and the consequential effects if their underlying mechanisms are impaired is relatively new; as such, the investigations included in this review have provided crucial information regarding preliminary psychological and physiological information in regard to systemic low-grade inflammation and chronic disease prevalence in the PTSD-afflicted population.Citation35 These studies have established the foundation upon which further research can build as a means to provide individuals suffering from PTSD with novel, long-term, effective treatment plans not only to improve the psychological symptoms of PTSD but also to reduce the physical morbidity and early mortality rates demonstrated in this population.Citation36 The universal theme embedded across the reviewed studies was the clear association between PTSD and systemic low-grade inflammation.
PTSD and inflammation
The major finding regarding the association between inflammation and PTSD was the significant difference in specific pro- and anti-inflammatory cytokines, acute-phase proteins, innate immune cells, and/or white blood cells between the PTSD-affected and unaffected, “healthy” groups. The most commonly tested acute-phase proteins, cytokines, innate immune cells, and white blood cells included CRP, IL-6, IL-10, TNF-α and IFN-γ, T lymphocytes, various complement components (classical and alternative pathways), and natural killer (NK) cells. Some of these biomarkers, such as CRP, IL-6, TNF-α, and IFN-γ, are known to display pro-inflammatory effects, while IL-10 is recognized as anti-inflammatory in nature.Citation29,Citation33 None of the reviewed studies found a statistically significant inter-group difference in IL-10.
Considering the studies that measured CRP, IL-6, TNF-α, and IFN-γ in PTSD sufferers versus non-PTSD sufferers, all but one found significantly higher levels of pro-inflammatory markers in the PTSD group compared with the non-PTSD group. While the outlying studies by Gola et alCitation25 and von Känel et alCitation18 argued for an overall pro-inflammatory state in individuals with PTSD, they did not find (contrary to their hypothesis) significant between-group differences in pro-inflammatory biomarkers. However, with regard to IL-4 and IL-6, none of the included studies took into account their dual role as both pro- and anti-inflammatory cytokines. This makes interpretation of the between-group measurements of IL-4 and IL-6 levels difficult because it is unclear whether they are acting as a pro- or anti-inflammatory cytokines in PTSD.Citation37,Citation38
The findings highlighted in this review are clinically important in the treatment of PTSD, because if an ongoing systemic low-grade inflammatory state is consistently detected in this population, treatment may then be directed towards managing the under-regulated inflammatory aspects of the disease to provide symptom relief and potential co-morbid chronic disease prevention.
PTSD and chronic disease risk
As evident in the included studies, PTSD is associated with overall elevated levels of various immune/inflammatory markers. Similarly, this pro-inflammatory state is also present in the pathogenesis of chronic physical illnesses such as CVD, insulin resistance, metabolic syndrome, pulmonary disorders, and autoimmune diseases.Citation9,Citation32 In the nine studies included for this review, it was the overarching view that these inflammatory processes found in both PTSD and chronic disease are related, and the catalyst for this elevated systemic inflammation may be stress induced.Citation9
The key findings presented were that acquiring PTSD leads to an increased risk for developing physical co-morbidities, with cardiovascular, metabolic, musculoskeletal, dermatological, and pulmonary diseases being diagnosed in this population most frequently.Citation39
From the evidence provided linking PTSD, inflammation, and chronic disease risk, it is essential to ensure that treatments are designed for this population such that the outcome provides a better quality of life for individuals with PTSD.
Heterogeneity of included studies
Of the studies included, it is clear that there is a link between PTSD, chronic disease risk, and a chronically pro-inflamed state. However, the large degree of heterogeneity between the studies cannot be ignored. There was a glaring absence of an included definition of “low-grade inflammation” in the majority of studies.Citation18–Citation23 The exclusion of this definition makes it difficult to determine the exact significance of the inter-group results in the context of inflammatory marker levels. In addition, all of the included studies measured inflammatory markers through the collection of plasma samples; however, recent research has shown that inflammatory markers collected via saliva more accurately depict the dysregulated immune state of PTSD participants.Citation40 There was also a lack of uniformity in psychological assessment and biomarker collection methods, as well as variations in the time of day at which samples were collected. These disparities make it difficult to directly compare the studies, as different methods for assessment and collection would have differing reliability and/or sensitivity, and diurnal variance in cytokine collection would certainly confound results as cytokine concentrations fluctuate throughout the day.Citation18
There were also inconsistencies between the studies included in this review and the confounding variables known to influence inflammation. These confounders include age, gender, ethnicity, education, marital status, employment, medications, psychiatric co-morbidities, asthma/allergies, physical co-morbidities, early life trauma, time since trauma, trauma type, BMI, alcohol/substance abuse, smoking status, and physical activity. This review recognizes that the included studies did attempt to control for various combinations of the aforementioned confounders (statistically through their results or via their inclusion/exclusion criteria) as well as the difficulty in controlling for all of these confounding factors; however, the reliability of the results still remains questionable. Without total control over the confounding variables, determining the exact cause of the demonstrated pro-inflammatory state in individuals with PTSD becomes difficult. Nonetheless, the results still displayed inconsistencies, with some studies indicating non-significance of results after controlling for certain confounding factors and the remaining studies demonstrating significance even after accounting for many of the above confounders.Citation6,Citation18–Citation25 Notably, the studies that did not consistently demonstrate statistically significant findings for elevation in all inflammatory markers in the PTSD participants still reported the presence of an overall pro-inflammatory state in this population compared to their healthy counterparts. The researchers from both studies attribute this conclusion to a suggested correlation between PTSD symptom severity and TNF-α levels in the PTSD sample, such that the more severe the PTSD symptoms, the higher the levels of TNF-α.Citation18,Citation25
Based upon the limitations discussed above, it appears that there is a definite need for future studies to establish inter-study homogeneity by defining “low-grade inflammation,” controlling assessment and collection methods, standardizing the time of day at which samples are collected, and accounting for the various confounding factors to the best of their abilities.
Clinical applications
There is a growing body of literature suggesting that there is a strong association between PTSD and chronic disease. Furthermore, this association may be independent of multiple confounding variables such as age, depression, and/ or co-morbid anxiety disorders.Citation41 There is agreement that PTSD appears to involve shifts within the central nervous system and immune/inflammatory processes, such that the effects of PTSD-related chronic stress causes a dysregulation of these systems, which then incurs an elevated risk for the subsequent development of multiple chronic illnesses with an inflammatory pathophysiology.Citation42,Citation43
Current standard PTSD management lies within the psychiatric parameters of this disorder.Citation43 However, there is a staggering lack of treatment targeting the co-morbid physical disease risk factors that ultimately result in overall impairment of long-term health and well-being.Citation42 In addition, there is limited research examining acute physiological recovery from stress in PTSD sufferers.Citation43 Such research will provide clarity on the appropriateness of their acute stress response that will help in the development of more effective treatment plans for this population.
Given that PTSD is not solely a psychiatric disorder, and the nature of its associated physical co-morbidities with inflammatory underpinnings, it is essential to develop appropriate cardiometabolic preventive therapy and treatment plans (in conjunction with therapeutic management) that reduce these long-term deleterious health outcomes.
Future research
Despite the research-based evidence of a chronic, low-grade pro-inflammatory state in individuals with PTSD and its link to long-term adverse health outcomes, the development of appropriate treatment methods to target these findings is yet to be established. As previously stated, the underlying link between PTSD and chronic somatic disease is illustrated by impaired psycho-physiological mechanisms leading to ongoing inflammation in these individuals. Therefore, treatment of both the psychological symptoms and physical co-morbidities in this population should address this chronically inflamed state.
Conclusion
PTSD is a severely crippling disorder that manifests in active-duty combat soldiers, military veterans, first responders and civilians alike, resulting in a number of long-term psychological and physical adverse health outcomes. The common feature underlying these conditions is a chronically elevated inflammatory state. Considering the devastating effects that PTSD has on the individual, his or her family, and society at large, there is a critical need to better understand the exact causes of PTSD and the regulatory systems/biological factors involved that contribute to the inflammatory state seen in PTSD. Once this has been achieved, implementation of an effective, easily accessible adjuvant treatment to usual care can be put in place to improve the quality of life of the PTSD population.
Disclosure
The authors report no conflicts of interest in this work.
References
- American Psychiatric AssociationDiagnostic and Statistical Manual of Mental Disorders, Fifth Edition: DSM-5Washington DCAmerican Psychiatric Publishing2013
- DennisPAWeinbergBJCalhounPSAn investigation of vago-regulatory and health-behavior accounts for increased inflammation in posttraumatic stress disorderJ Psychsom Res2016833339
- YehudaRPost-traumatic stress disorderN Engl J Med200234610811411784878
- HogeCWCastroCAMesserSCMcGurkDCottingDIKoffmanRLCombat duty in Iraq and Afghanistan, mental health problems, and barriers to careN Engl J Med2004351132215229303
- Foreign Affairs Defence and Trade References CommitteeMental Health of Australian Defence Force Members and VeteransCanberraDepartment of the Senate2016
- LindqvistDDhabharFSMellonSHIncreased pro-inflammatory milieu in combat related PTSD - a new cohort replication studyBrain Behav Immun20175926026427638184
- BabsonKAHeinzAJRamirezGThe interactive role of exercise and sleep on veteran recovery from symptoms of PTSDMent Health Phys Act201581520
- WolffEGaudlitzKvon LindenbergerBLPlagJHeinzAStröhleAExercise and physical activity in mental disordersEur Arch Psychiatry Clin Neurosci2011261Suppl 2S186S19121935629
- BlackPHThe inflammatory consequences of psychologic stress: relationship to insulin resistance, obesity, atherosclerosis and diabetes mellitus, type IIMed Hypotheses200667487989116781084
- DedertEACalhounPSWatkinsLLSherwoodABeckhamJCPosttraumatic stress disorder, cardiovascular, and metabolic disease: a review of the evidenceAnn Behav Med2010391617820174903
- ReevesJWFisherAJNewmanMGGrangerDASympathetic and hypothalamic-pituitary-adrenal asymmetry in generalized anxiety disorderPsychophysiology201653695195726934635
- DaskalakisNPLehrnerAYehudaREndocrine aspects of post-traumatic stress disorder and implications for diagnosis and treatmentEndocrinol Metab Clin North Am20134250351324011883
- DantzerRO’ConnorJCFreundGGJohnsonRWKelleyKWFrom inflammation to sickness and depression: when the immune system subjugates the brainNat Rev Neurosci200891465618073775
- MaesMBerkMGoehlerLDepression and sickness behavior are Janus-faced responses to shared inflammatory pathwaysBMC Med2012106622747645
- KrabbeKSReichenbergAYirmiyaRSmedAPedersenBKBruunsgaardHLow-dose endotoxemia and human neuropsychological functionsBrain Behav Immun200519545346015963684
- NeighGNAliFFCo-morbidity of PTSD and immune system dysfunction: opportunities for treatmentCurr Opin Pharmacol20162910411027479489
- WalkerAMcKuneAFergusonSPyneDBRattrayBChronic occupational exposures can influence the rate of PTSD and depressive disorders in first responders and military personnelExtrem Physiol Med20165827429749
- von KänelRHeppUKraemerBEvidence for low-grade systemic proinflammatory activity in patients with posttraumatic stress disorderJ Psychiatr Res200741974475216901505
- BersaniFSWolkowitzOMMilushJMA population of atypical CD56−CD16+ natural killer cells is expanded in PTSD and is associated with symptom severityBrain Behav Immun20165626427027025668
- HeathNMChesneySAGerhartJIInterpersonal violence, PTSD, and inflammation: potential psychogenic pathways to higher C-reactive protein levelsCytokine201363217217823701836
- HogeEABrandstetterKMoshierSPollackMHWongKKSimonNMBroad spectrum of cytokine abnormalities in panic disorder and posttraumatic stress disorderDepress Anxiety200926544745519319993
- HovhannisyanLPMkrtchyanGMSukiasianSHBoyajyanASAlterations in the complement cascade in post-traumatic stress disorderAllergy Asthma Clin Immunol201061320298515
- LindqvistDWolkowitzOMMellonSProinflammatory milieu in combat-related PTSD is independent of depression and early life stressBrain Behav Immun201442818824929195
- SpitzerCBarnowSVölzkeHAssociation of posttraumatic stress disorder with low-grade elevation of C-reactive protein: evidence from the general populationJ Psychiatr Res2010441152119628221
- GolaHEnglerHSommershofAPosttraumatic stress disorder is associated with an enhanced spontaneous production of pro-inflammatory cytokines by peripheral blood mononuclear cellsBMC Psychiatry20131314023360282
- LiberatiAAltmanDGTetzlaffJThe PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaborationPLoS Med200967e100010019621070
- MoherDLiberatiATetzlaffJAltmanDThe PRISMA GroupPreferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA StatementPLoS Med200967e100009719621072
- MacedoLGElkinsMRMaherCGMoseleyAMHerbertRDSherringtonCThere was evidence of convergent and construct validity of Physiotherapy Evidence Database quality scale for physiotherapy trialsJ Clin Epidemiol201063892092520171839
- VerhagenAPde VetHCde BieRAThe Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensusJ Clin Epidemiol1998511235124110086815
- MaherCGSherringtonCHerbertRDMoseleyAMElkinsMReliability of the PEDro scale for rating quality of randomized controlled trialsPhys Ther200383871372112882612
- SegerstromSCOutDGrangerDASmithTWBiological and physiological measures in health psychologyBenyaminiYJohnstonMKarademasECAssessment in Health PsychologyBoston, MAHogrefe2016227238
- GillJMSaliganLWoodsSPageGPTSD is assoicated with an excess of inflammatory immune activitiesPerspect Psychiatr C2009454262277
- McLeaySCHarveyWMRomaniukMNPhysical comorbidities of post-traumatic stress disorder in Australian Vietnam War veteransMed J Aust2017206625125728359007
- CorrellCUSolmiMVeroneseNPrevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: a large-scale meta-analysis of 3,211,768 patients and 113,383,368 controlsWorld Psychiatry201716216318028498599
- GroerMWKaneBWilliamsSNDuffyARelationship of PTSD symptoms with combat exposure, stress, and inflammation in American soldiersBiol Res Nurs201517330331025202037
- BoscarinoJAA prospective study of PTSD and early-age heart disease mortality among Vietnam veterans: implications for surveillance and preventionPsychosom Med200870666867618596248
- CavaillonJ-MPro- versus anti-inflammatory cytokines: myth or realityCell Mol Biol (Noisy-le-grand)200147469570211502077
- LuzinaIGKeeganADHellerNMRookGAShea-DonohueTAtamasSPRegulation of inflammation by interleukin-4: a review of “alternatives”J Leukoc Biol201292475376422782966
- BritvićDAntičevićVKaliternaMComorbidities with Post-traumatic Stress Disorder (PTSD) among combat veterans: 15 years postwar analysisInt J Clin Health Psychol20151528192
- WangZMandelHLevingstonCAYoungMRIAn exploratory approach demonstrating immune skewing and a loss of coordination among cytokines in plasma and saliva of Veterans with combat-related PTSDHum Immunol201677865265727216157
- KiblerJLPosttraumatic stress and cardiovascular disease riskJ Trauma Dissociation200910213515019333845
- PaceTWHeimCMA short review on the psychoneuroimmunology of posttraumatic stress disorder: from risk factors to medical comorbiditiesBrain Behav Immun201125161320934505
- LevineABLevineLMLevineTBPosttraumatic stress disorder and cardiometabolic diseaseCardiology2014127111924157651