Abstract
Beyond its critical function in calcium homeostasis, vitamin D has recently been found to play an important role in the modulation of the immune/inflammation system via regulating the production of inflammatory cytokines and inhibiting the proliferation of proinflammatory cells, both of which are crucial for the pathogenesis of inflammatory diseases. Several studies have associated lower vitamin D status with increased risk and unfavorable outcome of acute infections. Vitamin D supplementation bolsters clinical responses to acute infection. Moreover, chronic inflammatory diseases, such as atherosclerosis-related cardiovascular disease, asthma, inflammatory bowel disease, chronic kidney disease, nonalcoholic fatty liver disease, and others, tend to have lower vitamin D status, which may play a pleiotropic role in the pathogenesis of the diseases. In this article, we review recent epidemiological and interventional studies of vitamin D in various inflammatory diseases. The potential mechanisms of vitamin D in regulating immune/inflammatory responses in inflammatory diseases are also discussed.
Introduction
Vitamin D insufficiency or deficiency has increased in the general population and become an important public health issue.Citation1 Vitamin D is mainly known for its favorable effects in calcium and bone metabolism. However, increasing numbers of studies have established that vitamin D insufficiency contributes to a number of diseases, suggesting a range of physiological functions of vitamin D.Citation2–Citation4 Several clinical studies have confirmed that vitamin D plays a crucial role in modulating innate immune responses toward various pathogens.Citation5 Moreover, recent studies indicate that vitamin D can regulate the adaptive immune response in various inflammatory and autoimmune diseases.Citation6,Citation7 These results suggest the beneficial effects of vitamin D supplementation in decreasing the risk and adverse outcomes of inflammatory diseases, although the precise effect remains to be elucidated in large clinical trials.
The two major physiologically relevant forms of vitamin D are vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol). In humans, vitamin D3 seems to be more effective than vitamin D2 in maintaining the circulatory level of 25-hydroxyvitamin D3 (25[OH]D3), a stable marker of vitamin D status.Citation8,Citation9 The main sources of vitamin D3 are endogenous production from 7-dehydrocholesterol in the skin by ultraviolet B energy and dietary intake from foods, including egg yolk, beef liver, and milk products.Citation8,Citation9 Vitamin D3 is metabolized to 25(OH)D3 in the liver by vitamin D 25-hydroxylase and then further hydroxylated by the key enzyme 25-hydroxyl vitamin D3-1α-hydroxylase (CYP27B1) to the biologically active form: calcitriol (1,25-dihydroxycholecalciferol [1,25{OH}2D3]).Citation10 1,25(OH)2D3 binds and activates the vitamin D receptor (VDR), a member of the superfamily of nuclear receptors and functions as a ligand-activated transcription factor.Citation11 It is now well recognized that CYP27B1 and VDR are expressed in cells involved in the immune/inflammation system in the human body,Citation12 which provides the biological basis for the role of vitamin D in inflammatory diseases.
Most clinical studies support the view that serum 25(OH)D3 levels of less than 20 ng/mL (50 nmol/L) indicate vitamin D deficiency. Serum 25(OH)D3 levels below 30 ng/mL indicate insufficiency, while levels between 30 and 60 ng/mL (75 and 150 nmol/L) represent normal values.Citation1,Citation13 Epidemiological studies suggest an inverse association between circulating levels of 25(OH)D3 and inflammatory markers, including CRP and interleukin (IL)-6.Citation14 Supplemental vitamin D and calcium have been found to decrease the biomarkers of inflammation.Citation15,Citation16 However, a role for supplementation of vitamin D in modifying inflammatory disease has not been well defined, and it is unclear at present whether vitamin D status is causally related to the pathogenesis of the disease or is merely a marker of health.Citation17 This review summarizes and critically evaluates the data from preclinical, epidemiological, and interventional studies in order to elucidate the role and mechanisms of vitamin D in inflammatory diseases.
Vitamin D signaling and immune/inflammation system
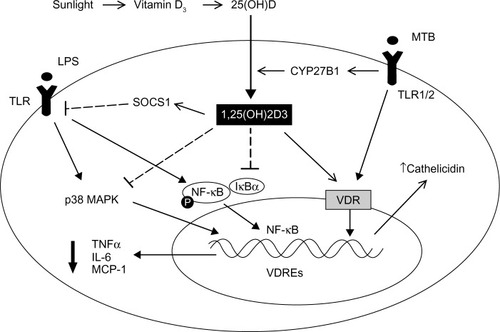
VDR expression has been documented in macrophages, a crucial cell type in the innate immune response.Citation18 In macrophages, activation of the toll-like receptor (TLR1/2) heterodimer by Mycobacterium tuberculosis results in the upregulation of VDR and CYP27B1, leading to induction of the antimicrobial peptide cathelicidin and the killing of intracellular M. tuberculosis.Citation19 In this process, IL-15 links TLR2/1-induced macrophage differentiation to the vitamin D-dependent antimicrobial pathway.Citation20 The increase of CYP27B1 results in the accumulation of 1,25(OH)2D3, which further activates VDR, leading to the target gene transcription via vitamin D response elements located in the regulatory regions of 1,25(OH)2D3 target genes.Citation21 Chen et alCitation22 found that 1,25(OH)2D3 can regulate TLR signaling via stimulating SOCS1 by downregulating miR-155 in macrophages, which provide a novel negative feedback regulatory mechanism for vitamin D to control innate immunity. In a recent study, both forms of vitamin D – 1,25(OH)2D3 and 25(OH)D3 – dose-dependently inhibited lipopolysaccharide-induced p38 phosphorylation, IL-6, and TNFα production by human monocytes via histone H4 in an acetylation-dependent manner.Citation23 Moreover, 1,25(OH)2D3 or its analogs have been shown to initiate the differentiation of myeloid progenitors into macrophages,Citation24 and to reduce MCP-1 and IL-6 expression via inhibiting the activation of NF-κB in macrophages.Citation25 In addition, Vitamin D has been thought to be a natural endoplasmic reticulum stress reliever,Citation26 and can selectively suppress key effector functions of interferon (IFN)-γ-activated macrophages.Citation27 Interestingly, in the presence of 1,25(OH)2D3, VDR has also been found to repress gene transcription via displacing the deoxyribonucleic acid-bound nuclear factor of activated T-cells, thus repressing inflammatory cytokine expressionCitation28 ().
Figure 1 Schematic representation of the primary mechanisms through which vitamin D regulates macrophage-mediated innate immune response.
Notes: vitamin D from sunlight or dietary sources is hydroxylated by the 25-hydroxylase to form its major circulating form – 25(OH)D3. 25(OH)D3 is then hydroxylated by 1α-hydroxylase (CYP27B1) to form the hormonal form of vitamin D – 1,25(OH)2D3. 1,25(OH)2D3 acts to modulate TLR signaling via stimulating SOCS1, inhibiting the phosphorylation of p38 MAPK and activation of NF-κB signaling in human macrophages, which reduces the gene expression and protein release of proinflammatory mediators, such as TNFα, IL-6, and MCP-1, leading to decreased recruitment of monocytes/macrophages and overall inflammation within tissue. In addition, 1,25(OH)2D3 acts to increase the production of the antimicrobial peptide cathelicidin and the killing of intracellular mycobacterium tuberculosis (MTB).
Abbreviations: LPS, lipopolysaccharide; VDR, vitamin D receptor; VDREs, vitamin D response elements; IL-6, interleukin-6; MAPK, mitogen-activated protein kinase; MCP-1, monocyte chemoattractant protein-1; TLR, toll-like receptor; TNFα, tumor necrosis factor-α.
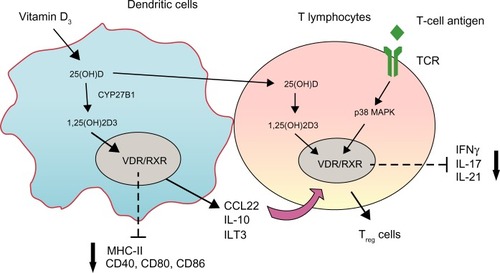
Dendritic cells (DCs) are the most potent antigen-presenting cells. A number of studies have shown that 1,25(OH)2D3 inhibits the differentiation, maturation, and immunostimulatory capacity of human DCs, characterized as the tolerogenic properties, in a VDR-dependent manner.Citation29,Citation30 Molecular mechanisms underlying the modulation of tolerogenic properties of DCs by 1,25(OH)2D3 include decreasing surface expression of major histocompatibility complex II and costimulatory molecules (CD40, CD80, CD86), upregulating inhibitory immunoglobulin-like transcript 3 molecules, and enhancing secretion of chemokine (C–C motif) ligand 22 and IL-10Citation29,Citation31 (). The enhancement of DC tolerogenicity by 1,25(OH)2D3 results in the induction of T-regulatory cells, a critical event for suppressing the inflammatory response of T-effector cells.Citation31 1,25(OH)2D3 also acts directly with VDR on the T lymphocyte to inhibit its proliferation.Citation32 Although native T-cells did not express VDR, VDR expression was induced by T-cell antigen-receptor signaling via the alternative p38 MAPK pathway, which is crucial for T-cell antigen-receptor responsiveness in naïve T-cells.Citation33 Recent work has revealed that 1,25(OH)2D3 inhibited production of proinflammatory cytokines, including IFNγ, IL-17, and IL-21 in CD4+CD25− T lymphocytes, and promoted development of T-regulatory cells expressing cytotoxic T-lymphocyte antigen 4 and FOXP3Citation34 (). T-cell cytokines also control vitamin D metabolism in macrophages. For example, IFNγ, a T-helper (Th)-1 cytokine, upregulates the macrophage CYP27B1, leading to enhanced bioconversion of 25(OH)D3 to its active metabolite – 1,25(OH)2D3. In contrast, the Th2 cytokine IL-4 induces catabolism of 25(OH)D3 to the inactive metabolite 24,25(OH)2D3,Citation35 suggesting a potential mechanism by which vitamin D metabolism links the cell-mediated immune responses to the innate immune responses, although the exact role of vitamin D in this process remains unclear.
Figure 2 Schematic representation of the primary mechanisms through which vitamin D-regulated dendritic cells (DCs) and T-lymphocyte function.
Notes: vitamin D precursors can be further processed to their active metabolite, 1,25(OH)2D3, in DCs and T lymphocytes. In DCs, 1,25(OH)2D3 binds to the vitamin D receptor–retinoid X receptor (VDR/RXR) complex in the nucleus, leading to a tolerogenic DC phenotype, characterized by decreased expression of major histocompatibility complex (MHC)-II, CD40, CD80, CD86, enhanced expression of immunoglobulin-like transcript (ILT)-3, and increased secretion of interleukin (IL)-10 and CCL22, which results in the induction of T-regulatory (Treg) cells. The 1,25(OH)2D3 signaling in T-cells is dependent on the stimulation of T-cell antigen-receptor (TCR) signaling. VDR expression can be induced by TCR signaling via the alternative p38 MAPK pathway. 1,25(OH)2D3 binds to VDR, leading to inhibition of proinflammatory cytokine expression, including interferon (IFN)-γ, IL-17, and IL-21, and promotion of the development of Treg cells.
Abbreviations: CCL22, chemokine (C-C motif) ligand 22; MAPK, mitogen-activated protein kinase.
Vitamin D and inflammatory diseases
Acute infections
Epidemiology studies have indicated seasonal variations in influenza and pneumococcal community-acquired pneumonia, suggesting an association between vitamin D insufficiency due to less sun exposure and acute respiratory infection (ARI).Citation36 A number of clinical studies have suggested an inverse association between 25(OH)D3 levels and ARI ().Citation37–Citation42 Ginde et alCitation41 performed a secondary analysis of the Third National Health and Nutrition Examination Survey, and found a strong negative association between serum 25(OH)D3 levels (<30 ng/mL) and risk of upper respiratory tract infection, which seemed to be stronger in individuals with asthma and chronic obstructive pulmonary disease. In a large retrospective study, vitamin D status was found to have a linear association with seasonal infections and lung function, in which each 10 nmol/L increase in 25(OH) D3 was associated with a 7% lower risk of infection and an 8 mL increase in forced expiratory volume in 1 second.Citation39 Several prospective cohort studies in adults and children further demonstrated that serum vitamin D concentration was associated with acute respiratory tract infection (ARTI): 25(OH)D3 levels <38 ng/mL were associated with increased risk of ARTI.Citation37,Citation40,Citation42 Recently, Mohamed et alCitation38 found that low cord blood 25(OH)D3 levels are associated with increased risk of ARTI in the first 2 years of life, suggesting a necessary early intervention for vitamin D starting from newborns.
Table 1 Summary of the major clinical studies evaluating the relationship between vitamin D status and acute respiratory infections
Evidence from double-blinded randomized clinical trials (RCTs) for vitamin D interventional studies is warranted to confirm the clinically relevant effect of vitamin D in RTIs. Camargo et alCitation43 investigated whether vitamin D supplementation in children with vitamin D deficiency would lower the risk of ARI. Compared with controls, children receiving vitamin D (300 IU/daily) have been reported to have significantly fewer ARIs during the study period. In another placebo-controlled double-blinded study comprising 164 voluntary young Finnish men (18–28 years of age), the proportion of men remaining healthy throughout the 6-month study period was greater in the intervention group (vitamin D3, 400 IU/daily) than in the placebo group.Citation44 More RCTs with larger populations, however, are warranted to investigate the role of vitamin D supplementation on respiratory health and ARI.
Studies with VDR-knockout mice have been critical in demonstrating the relationship between vitamin D and acute infections.Citation45–Citation49 Compared with VDR+/+ mice, VDR−/− mice exhibited significantly higher Chlamydia trachomatis loading and reduced clearance of chlamydial infection than wild-type VDR+/+ mice, suggesting a vitamin D–VDR pathway involved in respiratory mucosal defense against infections.Citation46 VDR-knockout mice developed an unaltered Th1 response to infection due to impaired upregulation of arginase 1 expression under Leishmania infection.Citation45 Although 1,25(OH)2D3 inhibits the proliferation and differentiation of both T and B lymphocytes, the central mechanism underlying microbial eradication of vitamin D seems to be the inhibition of activation of TLRs in the host cell, which induces the formation of potent antimicrobial peptides.Citation19,Citation50 The additional anti-infection mechanism of vitamin D may be related to the ability to modulate inflammatory factor levels in ARI patients. 25(OH)D3 levels below 21 ng/mL have an inverse relationship with CRP concentration in asymptomatic ambulatory patients.Citation51 However, these associations were not found in symptomatic patients.Citation52 In a randomized controlled trial of vitamin D supplements (1,400 IU/week) in infants, there were no differences in plasma levels of CRP or inflammatory cytokines between the treatment group and the control group.Citation53 The exact effects and mechanisms of vitamin D in infectious diseases therefore require further study.
The functioning of VDR is affected by gene polymorphisms, in which a start codon polymorphism (rs2228570) and three polymorphisms in the 3′ untranslated region (UTR) of the VDR gene (rs1544410, rs7975232, and rs731236) are the most commonly studied polymorphisms in the VDR gene.Citation54 There are reports that VDR polymorphism is linked to increased susceptibility to infection. Alagarasu et al have found that the frequency of the C/C genotype of rs7975232 was significantly lower in dengue virus infection patients (DEN) compared to health controls.Citation54 Aslan et al examined VDR gene polymorphisms in urinary tract infections, and found that the ff genotype in rs2228570 was significantly increased in UTI children with urinary tract infection.Citation55 Rathored et al have also found that the patients with ff genotypes in rs2228570 were at high risk of multidrug-resistant tuberculosis with smear-positive disease.Citation56 In a multicenter clinical trial, Levin et al recently investigated the relationship of common variation within genes encoding the vitamin D-binding protein, megalin, cubilin, CYP27B1, CYP24A1, and VDR with low 25(OH)D levels, and found some minor alleles at rs7968585 and rs7968585 within the VDR gene that were related to low 25(OH)D3.Citation57 The results of these studies suggest that VDR gene polymorphisms can be important for the susceptibility of inflammatory diseases, which may be due to the lower 25(OH)D3 status affected by VDR gene polymorphisms.
Atherosclerosis-related cardiovascular disease
It is well known that inflammation plays a key role in the development of atherosclerosis. Inflammatory cells, mainly macrophages and T lymphocytes, produce a wide range of inflammatory cytokines in atherosclerotic lesions, which are critically important in the progression of atherosclerosis-related cardiovascular disease (CVD).Citation58 Numerous studies have verified vitamin D deficiency (25[OH]D3 <20 ng/mL) as one of the new risk factors for coronary heart disease (CHD).Citation59,Citation60 Many potential functions of vitamin D – including protection of endothelial function, inhibition of smooth-muscle cell (SMC) proliferation, improvement of lipid profile, and others – have been thought to contribute to the antiatherogenic effect of vitamin D.Citation61–Citation63
Clinical studies have indicated an inverse association between 25(OH)D3 levels and CHD risk (). Three large retrospective studies demonstrated that 25(OH)D3 levels below 20 ng/mL are associated with increased risk for CHD, including hypertension, diabetes mellitus, obesity, high serum low-density lipoprotein (LDL), triglyceride (TG), and low high-density lipoprotein (HDL) levels.Citation17,Citation64,Citation65 Several cross-sectional prospective studies further strengthened this evidence, which demonstrated a significant increase for all-cause mortality when serum 25(OH)D3 levels were less than 30 ng/mL.Citation66–Citation70 In a population-based cohort study, Lim et alCitation71 reported that a low 25(OH)D3 concentration had a higher risk of significant coronary artery stenosis. The odds ratios were 2.08 for 25(OH)D3 concentration of 15–29.9 ng/mL versus at least 30 ng/mL and 3.12 for 25(OH)D3 concentration below 15 ng/mL versus at least 30 ng/mL.
Table 2 Summary of major clinical studies evaluating the relationship between vitamin D status and cardiovascular disease (CVD) risk
Although observational studies suggest that vitamin D deficiency or insufficiency is related to a higher risk for CVD, data from recent RCTs designed to assess the impact of vitamin D supplementation on cardiovascular outcomes are conflicting (). Some RCT results have shown that a higher intake of vitamin D is associated with a lower risk of CVD, especially in men, due to the improvement of vascular endothelial function and decrease in inflammation.Citation72–Citation74 However, most evidence at present shows that vitamin supplementation has no effect on vascular disease mortality or all-cause mortality.Citation73–Citation78 Since large well-controlled double-blinded RCTs aiming primarily for cardiovascular end points are still absent, whether or not vitamin D supplementation can significantly improve cardiovascular outcomes is largely unknown. At this time, larger RCTs, which can be used to evaluate the application of vitamin D in cardiology, have yet to be implemented.
Table 3 Summary of interventional studies evaluating the effect of vitamin D supplements on cardiovascular disease (CVD) risk
The regulation of the immune/inflammatory response is one of the most verified mechanisms of the antiatherogenic effect of vitamin D. First, vitamin D exerts protective effects against endothelial dysfunction, an inflammatory process that precedes atherosclerosis, via multiple mechanisms, including stimulating nitric oxide production and inhibiting oxidative stress.Citation59,Citation79 Vitamin D has been found to inhibit contractions, which were endothelium-dependent through inhibiting cyclooxygenase-1 expression and reactive oxygen species production.Citation59,Citation79 In addition, calcitriol significantly repressed the expression of cyclooxygenase 2 and promoted prostaglandin catabolism, both of which reduce the level of prostaglandins and suppress proinflammatory cytokine expression in endotheliocytes.Citation80 Second, 1,25(OH)2D3 may alter macrophage function and gene expression, which is crucial in the formation of foam cells and vascular inflammation response that promote the process of atherosclerosis.Citation26 In patients with type 2 diabetes mellitus, 1,25(OH)2D3 can inhibit foam-cell formation, and suppresses macrophage cholesterol uptake via reducing peroxisome proliferated-activated receptor-γ-dependent CD36 expression.Citation81 In addition, vitamin D induces an antiatherogenic monocyte/macrophage phenotype via regulating endoplasmic reticulum stress.Citation26 Previous studies by our group have found vitamin D deficiency causes increased proinflammatory cytokine expression in epicardial adipose tissue, which is coupled with increased inflammatory cellular infiltrate, suggesting the anti-inflammation effect of vitamin D in epicardial adipose tissue is a novel mechanism for atheroprotection.Citation82 Third, 1,25(OH)2D3 inhibits the proliferation of vascular SMCs (VSMCs),Citation83 and exerts protective effects against VSMC morphological changes, which further inhibit the secretion of inflammatory molecules.Citation84
In a hypercholesterolemic swine model, our group has found that vitamin D deficiency significantly increases the expression of TNFα in neointimal lesions after balloon angioplasty and that calcitriol has antiproliferative properties in TNFα-stimulated human VSMCs.Citation85 Besides the direct antiatherogenic effect, vitamin D has a variety of indirect effects on the systemic pathophysiological conditions that promote atherosclerosis, such as improving insulin resistance and hypertension.Citation59 However, Ponda et alCitation17,Citation77 recently reported repletion of 25(OH)D3 levels in the short term does not correct or even ameliorate dyslipidemia, suggesting that the definitive role of vitamin D in CVD remains to be elucidated.
Asthma
Asthma is a disorder characterized by varying and recurring symptoms of airflow obstruction and bronchial hyperresponsiveness in the setting of inflammation.Citation86 Epidemiologic studies suggest an association between vitamin D deficiency and asthma ().Citation87–Citation92 Some prospective studies and case-control studies have shown the majority of asthmatic children to be vitamin D-deficient.Citation91,Citation93 Vitamin D deficiency has been found to increase the risk of severe asthma exacerbation, defined as the need for emergency room evaluation or hospitalization.Citation94 A prospective study of adults and children found that low serum 25(OH)D3 levels were associated with increased requirement of steroids in the pediatric asthma group.Citation90 Higher maternal circulating 25(OH)D3 concentrations in pregnancy were independently associated with lower risk of asthma at 5 years old in offspring.Citation92 However, another study showed that high 25(OH)D3 levels in pregnant women could pose an increased risk of asthma in offspring,Citation95 indicating a reasonable level of vitamin D in pregnant women is crucial for maintaining normal bronchial responsiveness in offspring.
Table 4 Summary of major clinical studies evaluating the relationship between vitamin D status and asthma risk
The mechanisms of vitamin D deficiency in asthma pathophysiology are not fully understood. Many researchers have focused on the potential effect of vitamin D in inflammatory response that inhibits the progress of asthma.Citation86 Vitamin D has been found to increase the production of IL-10, an anti-inflammatory cytokine, while decreasing the expression of proinflammatory cytokines in airway SMCs.Citation96,Citation97 In a mouse model, Gorman et alCitation98 recently examined asthma-like responses 24 hours after airway challenge with the experimental allergen ovalbumin in adult offspring born to vitamin D3-replete and vitamin D3-deficient mothers. They found the ability of airway-draining lymph-node cells to proliferate and secrete cytokines in response to ovalbumin ex vivo was significantly enhanced by vitamin D deficiency.Citation98 In a mouse model of allergic airway inflammation, our group has previously found vitamin D deficiency causes an increase in the expression of TNFα, which decreases the expression of VDR and prohibitin, a vitamin D target gene.Citation95 Vitamin D supplementation reduces the levels of TNFα, thereby increasing the expression of VDR and prohibitin, which could be responsible for reducing allergic airway inflammation.Citation99
Inflammatory bowel diseases
Vitamin D deficiency is common in patients with inflammatory bowel diseases (IBDs), including ulcerative colitis (UC) and Crohn’s disease (CD)Citation100–Citation105 (). Several retrospective and cross-sectional studies have reported a high prevalence of vitamin D deficiency in patients with IBD, which was associated with disease activity and quality of life.Citation101–Citation105 Recently, a prospective cohort study of 72,719 women enrolled in the Nurses’ Health Study examined the relationship between vitamin D status and risk of CD and UC.Citation100 In this study, researchers used Cox proportional hazard modeling to examine the hazard ratio (HR) for incident CD or UC after adjusting for potential confounders. Compared with women with a predicted 25(OH)D3 level less than 20 ng/mL, the multivariate-adjusted HR was 0.38 (95% confidence interval 0.15–0.97) for CD and 0.57 (95% confidence interval 0.19–1.70) for UC for women with a predicted 25(OH) D3 level greater than 30 ng/mL, suggesting higher predicted plasma levels of 25(OH)D3 significantly reduce the risk for incident CD.Citation100
Table 5 Summary of major clinical studies evaluating the role of vitamin D status and vitamin D supplementation in inflammatory bowel disease (IBD)
Vitamin D supplementation has shown potential therapeutic benefit for IBD in some small, randomized, double-blind studies (). Jørgensen et alCitation106 reported that oral supplementation with vitamin D3 (1,200 IU/day for 12 months) significantly reduced the risk of IBD relapse from 29% to 13%. Yang et alCitation107 investigated the effect of high-dose vitamin D3 on serum vitamin D levels and CD activity index. They found supplementation of vitamin D3 (5,000 IU/day for 24 weeks) effectively raised serum 25(OH)D3 and reduced CD activity index scores. Pappa et alCitation108 reported oral doses of 2,000 IU vitamin D3 daily or 50,000 IU vitamin D2 weekly seem to be superior to 2,000 IU vitamin D2 daily in raising serum 25(OH)D3 concentration, and was tolerated among children and adolescents with IBD. Another study has shown that 1,25(OH)2D3 (active form of vitamin D) has a more prominent short-term beneficial effect than 25(OH)D3 (plain vitamin-D) on CD activity.Citation109 Although most studies have now shown vitamin D3 treatment might be effective in IBD, larger, randomized, double-blind, placebo-controlled trials needed to elucidate this correlation are lacking.
In VDR-knockout mice models, vitamin D deficiency increases susceptibility to dextran sodium sulfate-induced colitis.Citation110 Histological examination revealed the disruption in the epithelial junctions in dextran sodium sulfate-treated VDR−/− mice. 1,25(OH)2D3 preserved the integrity of the tight junctions in Caco-2 cell monolayers.Citation110 Ryz et alCitation111 found that 1,25(OH)2D3 treatment increases host susceptibility to Citrobacter rodentium, an extracellular microbe that causes acute colitis, by suppressing mucosal Th17 immune responses. Taken together, these observations suggest that vitamin D plays a critical role in mucosal barrier homeostasis by preserving the integrity of junctions via regulating the host immune/inflammatory response, leading to decreased susceptibility to mucosal damage and decreased risk of IBD.
Chronic kidney disease
Normal renal function is crucial for vitamin D metabolism.Citation1 Vitamin D deficiency is highly prevalent among patients with chronic kidney disease (CKD; 20%–85%).Citation112,Citation113 Studies have demonstrated a strong association between vitamin D deficiency and increased all-cause and CKD mortality in the general population ().Citation113–Citation118 Chronic low-grade inflammation is a hallmark of CKD, and has been disclosed as one important factor contributing to the progression of CKD and high cardiovascular mortality.Citation10 A prospective cohort study of 444 patients with eGFR <60 mL/min/1.73 m2 (follow-up time 9.4 years) showed that most patients died from cardiovascular causes.Citation116 Cox proportional hazard modeling has shown multivariate-adjusted HRs (with 95% confidence intervals) in severely vitamin D-deficient (25[OH]D3 <10 ng/mL) compared to vitamin D-sufficient patients (25[OH]D3 ≥30 ng/mL) were 3.79 (1.71–8.43) for all-cause and 5.61 (1.89–16.6) for cardiovascular mortality, suggesting low 25(OH)D3 levels are a crucial factor linking CKD to CVD.Citation116 Another cross-sectional study strengthened this evidence, demonstrating that higher vascular stiffness and endothelial dysfunction were associated with low levels of 25(OH) D3 and 1,25(OH)2D3 in CKD patients.Citation119 Vitamin D intake for more than 12 months can significantly reduce the probability of cardiovascular events.Citation117 Low 25(OH)D3 and 1,25(OH)2D3 levels are independently associated with albuminuria, a major risk factor for the progression of renal disease linked to all-cause mortality and cardiovascular mortality.Citation114 Treatment with active vitamin D preparations also has a beneficial effect in decreasing albuminuria.Citation120 Besides regulating inflammation and proteinuria, vitamin D has been found to improve aerobic capacity and increase the level of fetuin-A, an important protective factor for cardiovascular morbidity in pediatric CKD patients.Citation115,Citation121
Table 6 Summary of major clinical studies evaluating the relationship between vitamin D status and chronic kidney disease (CKD) risk
Several randomized, double-blind, placebo-controlled studies have examined the role of vitamin D as a therapeutic agent for CKD ().Citation120,Citation122–Citation127 High-dose cholecalciferol supplementation (50,000 IU/week for 12 weeks) was safe and sufficient to maintain serum 25(OH)D3 concentrations (≥30 ng/mL) and simultaneously decreased serum MCP-1 concentrations in early CKD.Citation122–Citation124 In moderate CKD patients, both cholecalciferol (vitamin D3) and ergocalciferol (vitamin D2) are effective in increasing 25(OH)D3 and decreasing parathyroid hormone and inflammatory cytokine levels.Citation125,Citation127 In nonhemodialysis patients, supplementation of cholecalciferol with 40,000 IU/week for 8 weeks significantly increased the level of 1,25(OH)2D3 and decreased serum parathyroid hormone and inflammatory cytokine levels.Citation126 However, this effect was not observed in end-stage renal disease (ESRD) patients.Citation126 As patients with CKD progress to ESRD, renal CYP27B1 activity decreases, resulting in the impaired formation of 1,25(OH)2D3 in many of these patients.Citation128 Previous attempts to counteract these changes in mineral metabolism with nutritional vitamin D therapy have been unsuccessful.Citation129 For this reason, most therapeutic approaches to treat vitamin D deficiency in ESRD patients favor the use of calcitriol or its associated analogs instead of the use of nutritional vitamin D forms.Citation128,Citation130 Interestingly, in an uncontrolled trial of seven ESRD patients, Stubbs et alCitation128 reported significant and favorable effects after 8 weeks of cholecalciferol supplementation on circulating monocytes and concentration of inflammatory cytokines, which may be have been due to extrarenal production of calcitriol in the setting of minimal renal CYP27B1 activity in ESRD patients.
Table 7 Summary of interventional studies evaluating the effect of vitamin D supplements on chronic kidney disease (CKD) risk
Experimental studies have demonstrated that vitamin D can control inflammation and oxidative stress that prevent CKD progress.Citation131,Citation132 Using a mouse model of obstructed nephropathy, Tan et alCitation132 reported that the synthetic vitamin D analog paricalcitol reduced the infiltration of inflammatory T-cells and macrophages in the obstructed kidney, which was accompanied by a decreased expression of RANTES and TNFα. In a human proximal tubular cell line (HKC-8), paricalcitol inhibited RANTES messenger ribonucleic acid and protein expression and abolished the ability of tubular cells to recruit lymphocytes and monocytes after TNFα stimulation.Citation132 In a study using a uremic rat model, paricalcitol significantly decreased cardiac oxidative stress. When combining with the angiotensin-converting enzyme inhibitor enalapril, paricalcitol further prevented inflammation and oxidative injury in uremic rats.Citation131 These studies provide experimental evidence supporting the role of inflammation in providing a pathological link between vitamin D and CKD.
Liver inflammatory disease
Nonalcoholic fatty liver disease (NAFLD) refers to the presence of hepatic steatosis without significant alcohol use or other known liver disease, and is characterized by chronic portal inflammation.Citation133 Recent studies emphasize the role of insulin resistance, metabolic syndrome, and proinflammatory cytokines in the development and progression of NAFLD.Citation134,Citation135 Vitamin D serum levels negatively correlate with insulin resistance and metabolic syndrome. Supplementation of vitamin D has been found to reduce insulin resistance in obese children.Citation134 Recently, lower vitamin D levels were found to be independently associated with increased severity of steatosis, necroinflammation, and fibrosis in NAFLD.Citation136,Citation137 Furthermore, serum vitamin D levels that could predict the severity of NAFLD independently of other metabolic characteristics and relate vitamin D to NAFLD are largely unknown. Considering that inflammation is followed by steatosis in most NAFLD patients,Citation138 vitamin D may be involved in NAFLD through its ability to modulate the immune/inflammation system. Recently, Roth et alCitation139 fed young (25-day-old) Sprague Dawley rats with a low-fat diet alone, with vitamin D depletion, or with a Westernized diet, and found that vitamin D-depleted animals fed a Westernized diet exhibited significantly greater hepatic steatosis and inflammation compared to low-fat diet groups, which may be related to the upregulation of TLR2, TLR4, TLR9, and endotoxin receptor CD14 in the liver, suggesting vitamin D depletion exacerbates NAFLD, possibly by way of endotoxin exposure in a Westernized diet rat model. Low vitamin D serum levels have also been found to correlate with the severity of inflammation and fibrosis in chronic hepatitis B and C viruses, where cellular immunity played crucial roles in the progress of diseases.Citation140,Citation141 In hepatitis B, VDR polymorphisms have been associated with infection susceptibility and clinical course in different populations.Citation142 Taken together, these data indicate a potential link between vitamin D and viral hepatitis.
Multiple sclerosis
Multiple sclerosis (MS) is a chronic inflammatory disease of the central nervous system, which affects more than 2 million individuals worldwide. Growing evidence suggest that vitamin D deficiency might be one of the most important environmental factors for the prevalence, relapse rate, and progression of MSCitation143–Citation146 (). In a large prospective case-control study of 7 million US military personnel, high circulating levels of 25(OH)D3 were found to be associated with a lower risk of MS, in which every 50 nmol/L increase in serum 25(OH)D3 led to a 41% decrease in MS risk.Citation145 Another prospective study of 35,794 mothers of participants in the Nurses’ Health Study II has shown that the relative risk of MS was lower among women born to mothers with high milk or vitamin D intake during pregnancy.Citation147 In addition, serum 25(OH)D3 concentrations in patients with MS were also found to be related to the relapse of the disease. Mowry et al found that each 10 ng/mL increase in 25(OH)D3 level was associated with a 15% lower risk of a new T2 lesion and a 32% lower risk of a gadolinium-enhancing lesion. Each 10 ng/mL increase in vitamin D level was associated with lower subsequent disability, suggesting higher vitamin D levels were associated with lower relapse risk.Citation143
Table 8 Summary of the major clinical studies evaluating the relationship between vitamin D status and multiple sclerosis (MS) risk
Although a link between vitamin D supplementation and decreased risk of MS has been widely assumed, present vitamin D-repletion therapies have not yet shown a significant effect on the progress of MS (). In a retrospective cohort study of 116,671 female registered nurses, intake of vitamin D (≥400 IU/day) from multivitamins was not been found to statistically reduce the risk of MS.Citation145 Moreover, no published RCTs of vitamin D repletion so far – low dose or high dose – have shown any benefit on relative risk of MS relapse.Citation148–Citation150 However, in a high-dose vitamin D3-supplementation RCT (20,000 IU/day for 12 weeks) in MS patients, vitamin D was found to increase proportion of IL-10+ CD4+ T-cells and decrease the ratio between IFNγ+ and IL-4+ CD4+ T-cells.Citation151 Moreover, in a myelin oligodendrocyte glycoprotein-induced animal model of MS, vitamin D significantly attenuated central nervous system inflammation and demyelination, accompanied by a lower amount of IFNγ-producing myelin oligodendrocyte glycoprotein-specific T-cells via a developmental stage-dependent manner.Citation152
These results suggest the exact effect of vitamin D repletion on the risk of MS remains to be clarified, since large, high-quality, randomized trials are still lacking.
Other inflammation/immune-related disorders
Inflammation has also been found to play an important role in other chronic diseases, including hypertension, diabetes, chronic lower-back pain (CLBP), and congestive heart failure (HF). Several reviews have thoroughly discussed the relationship between vitamin D and hypertension or diabetes.Citation153,Citation154 There is clear evidence to support an association between low plasma levels of 25(OH)D3 and hypertension and type 2 diabetes.Citation153,Citation154 Furthermore, clinical trials aimed at testing the effect of vitamin D supplementation on hypertension and type 2 diabetes documented a dose-dependent blood pressure-lowering and insulin sensitivity-increasing effect of vitamin D in patients.Citation155–Citation157 However, in a recent randomized, double-blind, placebo-controlled clinical trial, high-dose oral vitamin D3 (100,000 IU) for 6 months seemed not to reduce blood pressure or left ventricular mass in patients with resistant hypertension.Citation158 Because the 6-month period used in this study may have been too short a period to detect meaningful effects of vitamin D on left ventricular mass and function, longer trials and detailed studies are needed to better investigate the definite role of vitamin D supplementation in various forms of hypertension.
Nonspecific lower-back pain is one of the most common reasons for CLBP that burdens health care systems with high cost. Human population studies have shown that plasma levels of vitamin D are inversely associated with risk for CLBP.Citation159 However, results from a double-blind RCT of 53 patients aged 18–40 years with nonspecific CLBP showed no significant effect of vitamin D supplementation (50,000 IU) in decreasing the pain visual analog scale score of the patients.Citation160 Vitamin D deficiency is associated with loss of muscle strength and poor outcomes in patients with HF. In a double-blind RCT in 31 patients (25[OH]D3 levels ≤37.5 ng/mL), vitamin D3 repletion (50,000 IU) decreased aldosterone in patients with HF and low serum vitamin D, suggesting that vitamin D may be an important adjunct to standard HF therapy.Citation161
Apart from inflammatory disorders, vitamin D deficiency has been found to be associated with immune-related disorders, such as rheumatoid arthritis and systemic lupus erythematosus.Citation162,Citation163 Randomized placebo-controlled trials have shown that vitamin D supplementation seems to ameliorate inflammatory and hemostatic markers and show a tendency toward subsequent clinical improvement in these diseases.Citation146,Citation163,Citation164 In a healthy population, vitamin D levels were significantly higher in antinuclear antibody-negative individuals than antinuclear antibody-positive individuals.Citation165 Along with this finding is the additional observation that vitamin D deficiency is associated with certain immune abnormalities in such autoimmune disorders as systemic lupus erythematosus and rheumatoid arthritis.Citation163,Citation166 Recently, a retrospective cross-sectional study showed the risk of auto- and cellular immune abnormalities is increased in women with recurrent pregnancy losses and vitamin D deficiency.Citation167
Conclusion
The remarkable expression of the CYP27B1 and VDR genes by macrophages, DCs, and T lymphocytes suggests that the immune/inflammation system could be a target for the effect of vitamin D. Emerging evidence from clinical studies has indicated that vitamin D deficiency is associated with several inflammatory diseases; however, the question remains whether or not vitamin D deficiency contributes to the etiology of inflammatory disease or if vitamin D deficiency is simply a manifestation of these diseases. In acute infection and autoimmune disorders, preliminary evidence suggests an important role of vitamin D supplementation in decreasing the risk of disease. The pathophysiological process in many chronic inflammatory diseases, including atherosclerosis, is complex and confounded by various metabolic factors. Whether vitamin D supplementation is beneficial in the prognosis of these diseases requires further evaluation in larger prospective trials with a focus on major outcome events. In addition, dose-response randomized trials are necessary to identify threshold effects and possible adverse effects in vitamin D therapy. Future studies should aim to characterize optimal ranges of vitamin D status following vitamin D therapy, and should focus on determining the exact relationship between vitamin D dose and outcomes during the progression of diseases.
The identification and characterization of the molecular mechanisms responsible for recognizing and responding to vitamin D in the immune/inflammation system has widened our view of the essential components of a healthy immune response. Nonetheless, many key questions remain to be addressed. These include the cell type-specific roles of VDR in the progression of inflammatory diseases and the mechanisms of cross talk between VDR and other nuclear receptors, such as the retinoid X receptor and liver X receptor, which stimulate the intracellular pathway to exert the anti-inflammation effect. In addition, a single measurement of serum vitamin D status or the current standard value is unlikely to be valid in all situations. The development of research to refine existing biomarkers or establish new indicators that takes many factors into account and to identify useful functional biomarkers of vitamin D status in specific tissues will offer key insights into the development of targeted therapies for individuals with functional vitamin D insufficiency or deficiency in inflammatory diseases, though the research methodology for these potential biomarkers remains to be elucidated.
Acknowledgments
This work was supported by research grants HL112597, HL116042, and HL120659 from the US National Institutes of Health to DKA. The content of this review is solely the responsibility of the authors, and does not necessarily represent the official views of the NIH.
Disclosure
The authors report no conflicts of interest in this work.
References
- HolickMFVitamin D deficiencyN Engl J Med200735726628117634462
- LangloisMDuprezDDelangheJDe BuyzereMClementDLSerum vitamin C concentration is low in peripheral arterial disease and is associated with inflammation and severity of atherosclerosisCirculation20011031863186811294804
- PittasAGHarrisSSStarkPCDawson-HughesBThe effects of calcium and vitamin D supplementation on blood glucose and markers of inflammation in nondiabetic adultsDiabetes Care20073098098617277040
- WuSSunJVitamin D, vitamin D receptor, and macroautophagy in inflammation and infectionDiscov Med20111132533521524386
- WhiteJHVitamin D signaling, infectious diseases, and regulation of innate immunityInfect Immun2008763837384318505808
- TiosanoDWildbaumGGepsteinVThe role of vitamin D receptor in innate and adaptive immunity: a study in hereditary vitamin D-resistant rickets patientsJ Clin Endocrinol Metab2013981685169323482605
- OlliverMSpelminkLHiewJMeyer-HoffertUHenriques-NormarkBBergmanPImmunomodulatory effects of vitamin D on innate and adaptive immune responses to Streptococcus pneumoniaeJ Infect Dis20132081474148123922371
- LoganVFGrayARPeddieMCHarperMJHoughtonLALong-term vitamin D3 supplementation is more effective than vitamin D2 in maintaining serum 25-hydroxyvitamin D status over the winter monthsBr J Nutr20131091082108823168298
- ArmasLAHollisBWHeaneyRPVitamin D2 is much less effective than vitamin D3 in humansJ Clin Endocrinol Metab2004895387539115531486
- QuerfeldUVitamin D and inflammationPediatr Nephrol20132860561023239393
- NagyLSzantoASzatmariISzelesLNuclear hormone receptors enable macrophages and dendritic cells to sense their lipid environment and shape their immune responsePhysiol Rev20129273978922535896
- BrennanAKatzDRNunnJDDendritic cells from human tissues express receptors for the immunoregulatory vitamin D3 metabolite, dihydroxycholecalciferolImmunology1987614574612832307
- RosenCJClinical practice. Vitamin D insufficiencyN Engl J Med201136424825421247315
- LiuLCVoorsAAvan VeldhuisenDJVitamin D status and outcomes in heart failure patientsEur J Heart Fail20111361962521543375
- Björkhem-BergmanLNylénHNorlinACSerum levels of 25-hydroxyvitamin D and the CYP3A biomarker 4β-hydroxycholesterol in a high-dose vitamin D supplementation studyDrug Metab Dispos20134170470823386704
- HopkinsMHOwenJAhearnTEffects of supplemental vitamin D and calcium on biomarkers of inflammation in colorectal adenoma patients: a randomized, controlled clinical trialCancer Prev Res (Phila)201141645165421724580
- PondaMPHuangXOdehMABreslowJLKaufmanHWVitamin D may not improve lipid levels: a serial clinical laboratory data studyCirculation201212627027722718799
- KreutzMAndreesenRKrauseSWSzaboARitzEReichelH1,25-Dihydroxyvitamin D3 production and vitamin D3 receptor expression are developmentally regulated during differentiation of human monocytes into macrophagesBlood199382130013078394753
- LiuPTStengerSLiHToll-like receptor triggering of a vitamin D-mediated human antimicrobial responseScience20063111770177316497887
- KrutzikSRHewisonMLiuPTIL-15 links TLR2/1-induced macrophage differentiation to the vitamin D-dependent antimicrobial pathwayJ Immunol20081817115712018981132
- KorfHWenesMStijlemansB1,25-Dihydroxyvitamin D3 curtails the inflammatory and T cell stimulatory capacity of macrophages through an IL-10-dependent mechanismImmunobiology20122171292130022944250
- ChenYLiuWSunT1,25-Dihydroxyvitamin D promotes negative feedback regulation of TLR signaling via targeting microRNA-155-SOCS1 in macrophagesJ Immunol20131903687369523436936
- ZhangYLeungDYRichersBNVitamin D inhibits monocyte/macrophage proinflammatory cytokine production by targeting MAPK phosphatase-1J Immunol20121882127213522301548
- OhtaMOkabeTOzawaKUrabeATakakuF1α,25-Dihydroxyvitamin D3 (calcitriol) stimulates proliferation of human circulating monocytes in vitroFEBS Lett19851859133838944
- Sanchez-NiñoMDBozicMCórdoba-LanúsEBeyond proteinuria: VDR activation reduces renal inflammation in experimental diabetic nephropathyAm J Physiol Renal Physiol2012302F647F65722169009
- RiekAEOhJSpragueJEVitamin D suppression of endoplasmic reticulum stress promotes an antiatherogenic monocyte/macrophage phenotype in type 2 diabetic patientsJ Biol Chem2012287384823849423012375
- HelmingLBoseJEhrchenJ1α,25-Dihydroxyvitamin D3 is a potent suppressor of interferon γ-mediated macrophage activationBlood20051064351435816118315
- WhiteJHVitamin D metabolism and signaling in the immune systemRev Endocr Metab Disord201213212921845364
- GriffinMDLutzWPhanVABachmanLAMcKeanDJKumarRDendritic cell modulation by 1alpha, 25 dihydroxyvitamin D3 and its analogs: a vitamin D receptor-dependent pathway that promotes a persistent state of immaturity in vitro and in vivoProc Natl Acad Sci U S A2001986800680511371626
- PiemontiLMontiPSironiMVitamin D3 affects differentiation, maturation, and function of human monocyte-derived dendritic cellsJ Immunol20001644443445110779743
- TakedaMYamashitaTSasakiNOral administration of an active form of vitamin D3 (calcitriol) decreases atherosclerosis in mice by inducing regulatory T cells and immature dendritic cells with tolerogenic functionsArterioscler Thromb Vasc Biol2010302495250320930170
- MayneCGSpanierJARellandLMWilliamsCBHayesCE1,25-Dihydroxyvitamin D3 acts directly on the T lymphocyte vitamin D receptor to inhibit experimental autoimmune encephalomyelitisEur J Immunol20114182283221287548
- von EssenMRKongsbakMSchjerlingPOlgaardKOdumNGeislerCVitamin D controls T cell antigen receptor signaling and activation of human T cellsNat Immunol20101134434920208539
- JefferyLEBurkeFMuraM1,25-Dihydroxyvitamin D3 and IL-2 combine to inhibit T cell production of inflammatory cytokines and promote development of regulatory T cells expressing CTLA-4 and FoxP3J Immunol20091835458546719843932
- EdfeldtKLiuPTChunRT-cell cytokines differentially control human monocyte antimicrobial responses by regulating vitamin D metabolismProc Natl Acad Sci U S A2010107225932259821149724
- WhiteANNgVSpainCVJohnsonCCKinlinLMFismanDNLet the sun shine in: effects of ultraviolet radiation on invasive pneumococcal disease risk in Philadelphia, PennsylvaniaBMC Infect Dis2009919619961583
- ScienceMMaguireJLRussellMLSmiejaMWalterSDLoebMLow serum 25-hydroxyvitamin D level and risk of upper respiratory tract infection in children and adolescentsClin Infect Dis20135739239723677871
- MohamedWAAl-ShehriMACord blood 25-hydroxyvitamin D levels and the risk of acute lower respiratory tract infection in early childhoodJ Trop Pediatr201359293523022743
- BerryDJHeskethKPowerCHypponenEVitamin D status has a linear association with seasonal infections and lung function in British adultsBr J Nutr20111061433144021736791
- SabettaJRDePetrilloPCiprianiRJSmardinJBurnsLALandryMLSerum 25-hydroxyvitamin D and the incidence of acute viral respiratory tract infections in healthy adultsPLoS One20105e1108820559424
- GindeAAMansbachJMCamargoCAJrAssociation between serum 25-hydroxyvitamin D level and upper respiratory tract infection in the Third National Health and Nutrition Examination SurveyArch Intern Med200916938439019237723
- LaaksiIRuoholaJPTuohimaaPAn association of serum vitamin D concentrations <40 nmol/L with acute respiratory tract infection in young Finnish menAm J Clin Nutr20078671471717823437
- CamargoCAJrGanmaaDFrazierALRandomized trial of vitamin D supplementation and risk of acute respiratory infection in MongoliaPediatrics2012130e561e56722908115
- LaaksiIRuoholaJPMattilaVAuvinenAYlikomiTPihlajamäkiHVitamin D supplementation for the prevention of acute respiratory tract infection: a randomized, double-blinded trial among young Finnish menJ Infect Dis201020280981420632889
- EhrchenJHelmingLVargaGVitamin D receptor signaling contributes to susceptibility to infection with Leishmania majorFASEB J2007213208321817551101
- HeQAnanabaGAPatricksonJChlamydial infection in vitamin D receptor knockout mice is more intense and prolonged than in wild-type miceJ Steroid Biochem Mol Biol201313571423201171
- SchauberJDorschnerRACodaABInjury enhances TLR2 function and antimicrobial peptide expression through a vitamin D-dependent mechanismJ Clin Invest200711780381117290304
- WhitcombJPDeagostinoMBallentineMThe role of vitamin D and vitamin D receptor in immunity to Leishmania major infectionJ Parasitol Res2012201213464522007288
- YangHFZhangZHChangZQTangKLLinDZXuJZVitamin D deficiency affects the immunity against Mycobacterium tuberculosis infection in miceClin Exp Med20131326527022878932
- AnandaiahASinhaSBoleMVitamin D rescues impaired Mycobacterium tuberculosis-mediated tumor necrosis factor release in macrophages of HIV-seropositive individuals through an enhanced Toll-like receptor signaling pathway in vitroInfect Immun20138121023071135
- AmerMQayyumRRelation between serum 25-hydroxyvitamin D and C-reactive protein in asymptomatic adults (from the continuous National Health and Nutrition Examination Survey 2001 to 2006)Am J Cardiol201210922623021996139
- LucidarmeOMessaiEMazzoniTArcadeMdu CheyronDIncidence and risk factors of vitamin D deficiency in critically ill patients: results from a prospective observational studyIntensive Care Med2010361609161120373095
- Trilok-KumarGAroraHRajputMEffect of vitamin D supplementation of low birth weight term Indian infants from birth on cytokine production at 6 monthsEur J Clin Nutr20126674675022510791
- AlagarasuKHonapTMulayAPBachalRVShahPSCeciliaDAssociation of vitamin D receptor gene polymorphisms with clinical outcomes of dengue virus infectionHum Immunol2012731194119922917542
- AslanSAkilIAslanGOnayHOzyurtBCOzkinayFVitamin D receptor gene polymorphism in children with urinary tract infectionPediatr Nephrol20122741742121947233
- RathoredJSharmaSKSinghBRisk and outcome of multidrug-resistant tuberculosis: vitamin D receptor polymorphisms and serum 25(OH)DInt J Tuberc Lung Dis2012161522152822990231
- LevinGPRobinson-CohenCde BoerIHGenetic variants and associations of 25-hydroxyvitamin D concentrations with major clinical outcomesJAMA20123081898190523150009
- YinKDengXMoZCTristetraprolin-dependent post-transcriptional regulation of inflammatory cytokine mRNA expression by apolipoprotein A-I: role of ATP-binding membrane cassette transporter A1 and signal transducer and activator of transcription 3J Biol Chem2011286138341384521339300
- KassiEAdamopoulosCBasdraEKPapavassiliouAGRole of vitamin D in atherosclerosisCirculation20131282517253124297817
- StojanovicOILazovicMVuceljicMAssociation between atherosclerosis and osteoporosis, the role of vitamin DArch Med Sci2011717918822291755
- MerkeJMildePLewickaSIdentification and regulation of 1,25-dihydroxyvitamin D3 receptor activity and biosynthesis of 1,25-dihydroxyvitamin D3. Studies in cultured bovine aortic endothelial cells and human dermal capillariesJ Clin Invest198983190319152542376
- RebsamenMCSunJNormanAWLiaoJK1α,25-Dihydroxyvitamin D3 induces vascular smooth muscle cell migration via activation of phosphatidylinositol 3-kinaseCirc Res200291172412114317
- WangHXiaNYangYPengDQInfluence of vitamin D supplementation on plasma lipid profiles: a meta-analysis of randomized controlled trialsLipids Health Dis2012114222433171
- ParkSLeeBKVitamin D deficiency is an independent risk factor for cardiovascular disease in Koreans aged $50 years: results from the Korean National Health and Nutrition Examination SurveyNutr Res Pract2012616216822586506
- MartinsDWolfMPanDPrevalence of cardiovascular risk factors and the serum levels of 25-hydroxyvitamin D in the United States: data from the Third National Health and Nutrition Examination SurveyArch Intern Med20071671159116517563024
- ZhaoGFordESLiCCroftJBSerum 25-hydroxyvitamin D levels and all-cause and cardiovascular disease mortality among US adults with hypertension: the NHANES linked mortality studyJ Hypertens20123028428922179077
- WassonLTShimboDRubinMRShafferJASchwartzJEDavidsonKWIs vitamin D deficiency a risk factor for ischemic heart disease in patients with established cardiovascular disease? 10-Year follow-up of the Nova Scotia Health SurveyInt J Cardiol201114838738921396725
- SembaRDHoustonDKBandinelliSRelationship of 25-hydroxyvitamin D with all-cause and cardiovascular disease mortality in older community-dwelling adultsEur J Clin Nutr20106420320919953106
- WangTJPencinaMJBoothSLVitamin D deficiency and risk of cardiovascular diseaseCirculation200811750351118180395
- DobnigHPilzSScharnaglHIndependent association of low serum 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D levels with all-cause and cardiovascular mortalityArch Intern Med20081681340134918574092
- LimSShinHKimMJVitamin D inadequacy is associated with significant coronary artery stenosis in a community-based elderly cohort: the Korean Longitudinal Study on Health and AgingJ Clin Endocrinol Metab20129716917822013101
- HarrisRAPedersen-WhiteJGuoDHVitamin D3 supplementation for 16 weeks improves flow-mediated dilation in overweight African-American adultsAm J Hypertens20112455756221311504
- ZittermannAFrischSBertholdHKVitamin D supplementation enhances the beneficial effects of weight loss on cardiovascular disease risk markersAm J Clin Nutr2009891321132719321573
- SunQShiLRimmEBVitamin D intake and risk of cardiovascular disease in US men and womenAm J Clin Nutr20119453454221653796
- CauleyJAChlebowskiRTWactawski-WendeJCalcium plus vitamin D supplementation and health outcomes five years after active intervention ended: the Women’s Health InitiativeJ Womens Health (Larchmt)20132291592924131320
- GepnerADRamamurthyRKruegerDCKorcarzCEBinkleyNSteinJHA prospective randomized controlled trial of the effects of vitamin D supplementation on cardiovascular disease riskPLoS One20127e3661722586483
- PondaMPDowdKFinkielsteinDHoltPRBreslowJLThe short-term effects of vitamin D repletion on cholesterol: a randomized, placebo-controlled trialArterioscler Thromb Vasc Biol2012322510251522947589
- YiuYFYiuKHSiuCWRandomized controlled trial of vitamin D supplement on endothelial function in patients with type 2 diabetesAtherosclerosis201322714014623298824
- WongMSDelansorneRManRYSvenningsenPVanhouttePMChronic treatment with vitamin D lowers arterial blood pressure and reduces endothelium-dependent contractions in the aorta of the spontaneously hypertensive ratAm J Physiol Heart Circ Physiol2010299H1226H123420693391
- KrishnanAVFeldmanDMolecular pathways mediating the anti-inflammatory effects of calcitriol: implications for prostate cancer chemo-prevention and treatmentEndocr Relat Cancer201017R19R3819926709
- OhJWengSFeltonSK1,25(OH)2 vitamin D inhibits foam cell formation and suppresses macrophage cholesterol uptake in patients with type 2 diabetes mellitusCirculation200912068769819667238
- GuptaGKAgrawalTDelCoreMGMohiuddinSMAgrawalDKVitamin D deficiency induces cardiac hypertrophy and inflammation in epicardial adipose tissue in hypercholesterolemic swineExp Mol Pathol201293829022537546
- CarthyEPYamashitaWHsuAOoiBS1,25-Dihydroxyvitamin D3 and rat vascular smooth muscle cell growthHypertension1989139549592786849
- TukajSTrzonkowskiPTukajCRegulatory effects of 1,25-dihydroxyvitamin D3 on vascular smooth muscle cellsActa Biochim Pol20125939540022910558
- GuptaGKAgrawalTDel CoreMGHunterWJ3rdAgrawalDKDecreased expression of vitamin D receptors in neointimal lesions following coronary artery angioplasty in atherosclerotic swinePLoS One20127e4278922880111
- FinkleaJDGrossmannRETangprichaVVitamin D and chronic lung disease: a review of molecular mechanisms and clinical studiesAdv Nutr2011224425322332056
- CamargoCAJrRifas-ShimanSLLitonjuaAAMaternal intake of vitamin D during pregnancy and risk of recurrent wheeze in children at 3 y of ageAm J Clin Nutr20078578879517344501
- ErkkolaMKailaMNwaruBIMaternal vitamin D intake during pregnancy is inversely associated with asthma and allergic rhinitis in 5-year-old childrenClin Exp Allergy20093987588219522996
- FreishtatRJIqbalSFPillaiDKHigh prevalence of vitamin D deficiency among inner-city African American youth with asthma in Washington, DCJ Pediatr201015694895220236657
- GolevaESearingDAJacksonLPRichersBNLeungDYSteroid requirements and immune associations with vitamin D are stronger in children than adults with asthmaJ Allergy Clin Immunol20121291243125122330698
- KornSHübnerMJungMBlettnerMBuhlRSevere and uncontrolled adult asthma is associated with vitamin D insufficiency and deficiencyRespir Res2013142523432854
- MoralesERomieuIGuerraSMaternal vitamin D status in pregnancy and risk of lower respiratory tract infections, wheezing, and asthma in offspringEpidemiology201223647122082994
- BenerAEhlayelMSTulicMKHamidQVitamin D deficiency as a strong predictor of asthma in childrenInt Arch Allergy Immunol201215716817521986034
- BrehmJMSchuemannBFuhlbriggeALSerum vitamin D levels and severe asthma exacerbations in the Childhood Asthma Management Program studyJ Allergy Clin Immunol20101265258.e520538327
- GaleCRRobinsonSMHarveyNCMaternal vitamin D status during pregnancy and child outcomesEur J Clin Nutr200862687717311057
- SongYQiHWuCEffect of 1,25-(OH)2D3 (a vitamin D analogue) on passively sensitized human airway smooth muscle cellsRespirology20071248649417587413
- XystrakisEKusumakarSBoswellSReversing the defective induction of IL-10-secreting regulatory T cells in glucocorticoid-resistant asthma patientsJ Clin Invest200611614615516341266
- GormanSTanDHLambertMJScottNMJudgeMAHartPHVitamin D(3) deficiency enhances allergen-induced lymphocyte responses in a mouse model of allergic airway diseasePediatr Allergy Immunol201223838722283404
- AgrawalTGuptaGKAgrawalDKVitamin D deficiency decreases the expression of VDR and prohibitin in the lungs of mice with allergic airway inflammationExp Mol Pathol201293748122537547
- AnanthakrishnanANKhaliliHHiguchiLMHigher predicted vitamin D status is associated with reduced risk of Crohn’s diseaseGastroenterology201214248248922155183
- LevinADWadheraVLeachSTVitamin D deficiency in children with inflammatory bowel diseaseDig Dis Sci20115683083621222159
- UlitskyAAnanthakrishnanANNaikAVitamin D deficiency in patients with inflammatory bowel disease: association with disease activity and quality of lifeJPEN J Parenter Enteral Nutr20113530831621527593
- PappaHMGordonCMSaslowskyTMVitamin D status in children and young adults with inflammatory bowel diseasePediatrics20061181950196117079566
- SentongoTASemaeoEJStettlerNPiccoliDAStallingsVAZemelBSVitamin D status in children, adolescents, and young adults with Crohn diseaseAm J Clin Nutr2002761077108112399281
- JahnsenJFalchJAMowinckelPAadlandEVitamin D status, parathyroid hormone and bone mineral density in patients with inflammatory bowel diseaseScand J Gastroenterol20023719219911843057
- JørgensenSPAgnholtJGlerupHClinical trial: vitamin D3 treatment in Crohn’s disease – a randomized double-blind placebo-controlled studyAliment Pharmacol Ther20103237738320491740
- YangLWeaverVSmithJPBingamanSHartmanTJCantornaMTTherapeutic effect of vitamin D supplementation in a pilot study of Crohn’s patientsClin Transl Gastroenterol20134e3323594800
- PappaHMMitchellPDJiangHTreatment of vitamin D insufficiency in children and adolescents with inflammatory bowel disease: a randomized clinical trial comparing three regimensJ Clin Endocrinol Metab2012972134214222456619
- MihellerPMuzesGHritzIComparison of the effects of 1,25 dihydroxyvitamin D and 25 hydroxyvitamin D on bone pathology and disease activity in Crohn’s disease patientsInflamm Bowel Dis2009151656166219408329
- KongJZhangZMuschMWNovel role of the vitamin D receptor in maintaining the integrity of the intestinal mucosal barrierAm J Physiol Gastrointest Liver Physiol2008294G208G21617962355
- RyzNRPattersonSJZhangYActive vitamin D (1,25-dihydroxyvitamin D3) increases host susceptibility to Citrobacter rodentium by suppressing mucosal Th17 responsesAm J Physiol Gastrointest Liver Physiol2012303G1299G131123019194
- AliFNArguellesLMLangmanCBPriceHEVitamin D deficiency in children with chronic kidney disease: uncovering an epidemicPediatrics200912379179619255004
- SatirapojBLimwannataPChaiprasertASupasyndhOChoovichianPVitamin D insufficiency and deficiency with stages of chronic kidney disease in an Asian populationBMC Nephrol20131420624083392
- IsakovaTGutiérrezOMPatelNMAndressDLWolfMLevinAVitamin D deficiency, inflammation, and albuminuria in chronic kidney disease: complex interactionsJ Ren Nutr20112129530220817560
- PetcheyWGHowdenEJJohnsonDWHawleyCMMarwickTIsbelNMCardiorespiratory fitness is independently associated with 25-hydroxyvitamin D in chronic kidney diseaseClin J Am Soc Nephrol2011651251821164020
- PilzSTomaschitzAFriedlCVitamin D status and mortality in chronic kidney diseaseNephrol Dial Transplant2011263603360921378153
- SantoroDGittoLFerraroASattaESavicaVBellinghieriGVitamin D status and mortality risk in patients with chronic kidney diseaseRen Fail20113318419121332341
- SeeherunvongWAbitbolCLChandarJZillerueloGFreundlichMVitamin D insufficiency and deficiency in children with early chronic kidney diseaseJ Pediatr2009154906911.e119230902
- LondonGMGuérinAPVerbekeFHMineral metabolism and arterial functions in end-stage renal disease: potential role of 25-hydroxyvitamin D deficiencyJ Am Soc Nephrol20071861362017202417
- MolinaPGórrizJLMolinaMDThe effect of cholecalciferol for lowering albuminuria in chronic kidney disease: a prospective controlled studyNephrol Dial Transplant2014299710923975842
- SchaibleJWiggerMStaudeHSerum fetuin-A and vitamin D in children with mild-to-severe chronic kidney disease: a cross-sectional studyNephrol Dial Transplant2012271107111321750155
- AlvarezJALawJCoakleyKEHigh-dose cholecalciferol reduces parathyroid hormone in patients with early chronic kidney disease: a pilot, randomized, double-blind, placebo-controlled trialAm J Clin Nutr20129667267922854402
- AlvarezJAZughaierSMLawJEffects of high-dose cholecalciferol on serum markers of inflammation and immunity in patients with early chronic kidney diseaseEur J Clin Nutr20136726426923361158
- ChandraPBinongoJNZieglerTRCholecalciferol (vitamin D3) therapy and vitamin D insufficiency in patients with chronic kidney disease: a randomized controlled pilot studyEndocr Pract200814101718238736
- KooiengaLFriedLScraggRKendrickJSmitsGChoncholMThe effect of combined calcium and vitamin D3 supplementation on serum intact parathyroid hormone in moderate CKDAm J Kidney Dis20095340841619185400
- MarckmannPAgerskovHThineshkumarSRandomized controlled trial of cholecalciferol supplementation in chronic kidney disease patients with hypovitaminosis DNephrol Dial Transplant2012273523353122822092
- ShroffRWanMGullettAErgocalciferol supplementation in children with CKD delays the onset of secondary hyperparathyroidism: a randomized trialClin J Am Soc Nephrol2012721622322266572
- StubbsJRIdicullaASlusserJMenardRQuarlesLDCholecalciferol supplementation alters calcitriol-responsive monocyte proteins and decreases inflammatory cytokines in ESRDJ Am Soc Nephrol20102135336120007751
- ZismanALHristovaMHoLTSpragueSMImpact of ergocalciferol treatment of vitamin D deficiency on serum parathyroid hormone concentrations in chronic kidney diseaseAm J Nephrol200727364317215573
- AlbalateMde la PiedraCOrtizARisk in dosing regimens for 25-OH vitamin D supplementation in chronic haemodialysis patientsNephron Clin Pract2012121c112c11923221739
- HusainKFerderLMizobuchiMFinchJSlatopolskyECombination therapy with paricalcitol and enalapril ameliorates cardiac oxidative injury in uremic ratsAm J Nephrol20092946547219033720
- TanXWenXLiuYParicalcitol inhibits renal inflammation by promoting vitamin D receptor-mediated sequestration of NF-kappaB signalingJ Am Soc Nephrol2008191741175218525004
- BruntEMKleinerDEWilsonLAPortal chronic inflammation in nonalcoholic fatty liver disease (NAFLD): a histologic marker of advanced NAFLD-clinicopathologic correlations from the nonalcoholic steatohepatitis clinical research networkHepatology20094980982019142989
- KelishadiRSalekaSSalekaMHashemipouraMMovahedianMEffects of vitamin D supplementation on insulin resistance and cardiometabolic risk factors in children with metabolic syndrome: a triple-masked controlled trialJ Pediatr (Rio J)201490283424140383
- WongwiwatthananukitSSansanayudhNPhetkrajaysangNKrittiyanuntSEffects of vitamin D(2) supplementation on insulin sensitivity and metabolic parameters in metabolic syndrome patientsJ Endocrinol Invest20133655856323385553
- PirgonOCekmezFBilginHErenEDundarBLow 25-hydroxyvitamin D level is associated with insulin sensitivity in obese adolescents with non-alcoholic fatty liver diseaseObes Res Clin Pract20137e235e32024455759
- JablonskiKLJovanovichAHolmenJLow 25-hydroxyvitamin D level is independently associated with non-alcoholic fatty liver diseaseNutr Metab Cardiovasc Dis20132379279823415456
- TilgHMoschenAREvolution of inflammation in nonalcoholic fatty liver disease: the multiple parallel hits hypothesisHepatology2010521836184621038418
- RothCLElfersCTFiglewiczDPVitamin D deficiency in obese rats exacerbates nonalcoholic fatty liver disease and increases hepatic resistin and Toll-like receptor activationHepatology2012551103111121994008
- SchaalanMFMohamedWAAminHHVitamin D deficiency: correlation to interleukin-17, interleukin-23 and PIIINP in hepatitis C virus genotype 4World J Gastroenterol2012183738374422851868
- ZittESprenger-MährHKnollFNeyerULhottaKVitamin D deficiency is associated with poor response to active hepatitis B immunisation in patients with chronic kidney diseaseVaccine20123093193522142584
- ZúñigaSFirrincieliDHoussetCChignardNVitamin D and the vitamin D receptor in liver pathophysiologyClin Res Hepatol Gastroenterol20113529530221440524
- MowryEMWaubantEMcCullochCEVitamin D status predicts new brain magnetic resonance imaging activity in multiple sclerosisAnn Neurol20127223424022926855
- MartinelliVDalla CostaGColomboBVitamin D levels and risk of multiple sclerosis in patients with clinically isolated syndromesMult Scler20142014715523836877
- MungerKLLevinLIHollisBWHowardNSAscherioASerum 25-hydroxyvitamin D levels and risk of multiple sclerosisJAMA20062962832283817179460
- Pierrot-DeseillignyCRivaud-PéchouxSClersonPde PazRSouberbielleJCRelationship between 25-OH-D serum level and relapse rate in multiple sclerosis patients before and after vitamin D supplementationTher Adv Neurol Disord2012518719822783368
- MirzaeiFMichelsKBMungerKGestational vitamin D and the risk of multiple sclerosis in offspringAnn Neurol201170304021786297
- BurtonJMKimballSViethRA phase I/II dose-escalation trial of vitamin D3 and calcium in multiple sclerosisNeurology2010741852185920427749
- ShaygannejadVJanghorbaniMAshtariFDehghanHEffects of adjunct low-dose vitamin D on relapsing-remitting multiple sclerosis progression: preliminary findings of a randomized placebo-controlled trialMult Scler Int2012201245254122567287
- KampmanMTSteffensenLHMellgrenSIJørgensenLEffect of vitamin D3 supplementation on relapses, disease progression, and measures of function in persons with multiple sclerosis: exploratory outcomes from a double-blind randomised controlled trialMult Scler2012181144115122354743
- SmoldersJPeelenEThewissenMSafety and T cell modulating effects of high dose vitamin D3 supplementation in multiple sclerosisPLoS One20105e1523521179201
- AdzemovicMZZeitelhoferMHochmeisterSGustafssonSAJagodicMEfficacy of vitamin D in treating multiple sclerosis-like neuroinflammation depends on developmental stageExp Neurol2013249394823954214
- OzfiratZChowdhuryTAVitamin D deficiency and type 2 diabetesPostgrad Med J2010861825 quiz 2420065337
- TamezHThadhaniRIVitamin D and hypertension: an update and reviewCurr Opin Nephrol Hypertens20122149249922820371
- SugdenJADaviesJIWithamMDMorrisADStruthersADVitamin D improves endothelial function in patients with type 2 diabetes mellitus and low vitamin D levelsDiabet Med20082532032518279409
- FormanJPScottJBNgKEffect of vitamin D supplementation on blood pressure in blacksHypertension20136177978523487599
- AsemiZHashemiTKaramaliMSamimiMEsmaillzadehAEffects of vitamin D supplementation on glucose metabolism, lipid concentrations, inflammation, and oxidative stress in gestational diabetes: a double-blind randomized controlled clinical trialAm J Clin Nutr2013981425143224132976
- WithamMDIrelandSHoustonJGVitamin D therapy to reduce blood pressure and left ventricular hypertrophy in resistant hypertension: randomized, controlled trialHypertension20146370671224420547
- LewisPJVitamin D deficiency may have role in chronic low back painBMJ200533110916002895
- SandoughiMZakeriZMirhosaineeZMohammadiMShahbakhshSThe effect of vitamin D on nonspecific low back painInt J Rheum Dis Epub10142013
- BoxerRSHoitBDSchmotzerBJStefanoGTGomesANegreaLThe effect of vitamin D on aldosterone and health status in patients with heart failureJ Card Fail Epub242014
- CantornaMTMahonBDMounting evidence for vitamin D as an environmental factor affecting autoimmune disease prevalenceExp Biol Med (Maywood)20042291136114215564440
- Abou-RayaAAbou-RayaSHelmiiMThe effect of vitamin D supplementation on inflammatory and hemostatic markers and disease activity in patients with systemic lupus erythematosus: a randomized placebo-controlled trialJ Rheumatol20134026527223204220
- LeventisPPatelSClinical aspects of vitamin D in the management of rheumatoid arthritisRheumatology (Oxford)2008471617162118682414
- RitterhouseLLCroweSRNiewoldTBVitamin D deficiency is associated with an increased autoimmune response in healthy individuals and in patients with systemic lupus erythematosusAnn Rheum Dis2011701569157421586442
- KahlLEKambohMIDecrooSFerrellREAlpha-1-antitrypsin (PI) and vitamin-D binding globulin (GC) phenotypes in rheumatoid arthritis: absence of an associationDis Markers1989771782786461
- OtaKDambaevaSHanARBeamanKGilman-SachsAKwak-KimJVitamin D deficiency may be a risk factor for recurrent pregnancy losses by increasing cellular immunity and autoimmunityHum Reprod20142920821924277747
- StrickerHTosi BiandaFGuidicelli-NicolosiSLimoniCColucciGEffect of a single, oral, high-dose vitamin D supplementation on endothelial function in patients with peripheral arterial disease: a randomised controlled pilot studyEur J Vasc Endovasc Surg20124430731222831874
- BrehmJMCeledónJCSoto-QuirosMESerum vitamin D levels and markers of severity of childhood asthma in Costa RicaAm J Respir Crit Care Med200917976577119179486
- MoeSMSaifullahALaClairREUsmanSAYuZA randomized trial of cholecalciferol versus doxercalciferol for lowering parathyroid hormone in chronic kidney diseaseClin J Am Soc Nephrol2010529930620056760
- RuniaTFHopWCde RijkeYBBuljevacDHintzenRQLower serum vitamin D levels are associated with a higher relapse risk in multiple sclerosisNeurology20127926126622700811
- MungerKLChitnisTFrazierALGiovannucciESpiegelmanDAscherioADietary intake of vitamin D during adolescence and risk of multiple sclerosisJ Neurol201125847948520945071
