Dear editor
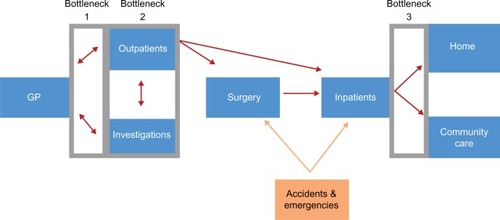
We read with great interest the article by Zaghloul and El Enein and agree with the conclusions made in particular regarding overbooking of outpatient services due to a mismatching of resources and the need for efficient outpatient scheduling.Citation1 We believe these points to be relevant to the current status of the National Health Service (NHS), which is facing an ever growing demand for its services, leading to increasing waiting times as a result.Citation2 Across NHS England, 838,600 patients were waiting for a key diagnostic test at the end of November 2015, a 5.6% increase from November 2014.Citation3 Waiting times have been associated with lower patient satisfaction and reduced clinical outcomes.Citation4,Citation5 It is therefore crucial that management teams take an active approach to reducing waiting times. illustrates a process map through which we have developed strategies for minimization of waiting times by facilitating patient flow.
Strategy
Minimizing unnecessary appointments
The current referral process involves too many steps causing delays in access to consultations with hospital specialists. As highlighted by Zaghloul and El Enein, follow-up appointments contribute significantly to overall outpatient appointments.Citation1 There are 37 million yearly follow-up appointments in the NHS, many of which are deemed clinically unnecessary. Furthermore, there are currently 6 million missed appointments each year where patients have failed to notify the hospital in advance. Ultimately, this wastes valuable resources such as time, labor, and money, which would be better suited to treating others in true need of medical attention.Citation6
These issues can be improved by eliminating steps, which do not create patient value within the referral process, in accordance with lean transformation model.Citation7 Referrals should be direct between hospital departments rather than the traditional path of returning referrals to general practitioners. Furthermore, NHS England found that only 50% of general practitioners use e-referral effectively, despite the system’s ability to reduce the number of DNA appointments by up to 60% when its use is optimized throughout a trust.Citation8 A qualitative analysis should be performed to understand the current barriers to the use of e-referrals among practitioners.Citation9
Optimizing appointment scheduling
Currently, the scheduling of outpatient and investigation appointments is not aligned to the predictable, fluctuating demands of patient care. The national audit office identified that between Friday and Saturday demand for elective and emergency services falls dramatically, with the former dropping more significantly.Citation8 Multiple carve-out queues add inefficiency throughout this process, especially at times of high demand, increasing waiting times for patients.Citation6
Hence, when forecasted emergency admissions are low, strain on the system is relieved; thus, we propose shifting the demand for elective services to these periods.Citation8 Alternatively, transferring capacity within the system may allow meeting overflow demand. This will include adding appointment slots as needed or making infrastructural changes such as outsourcing demand to other departments.Citation10
Reducing delays in transfer of care
Delays in transfer of care create a bottleneck at the end of the patient process pathway, resulting in backlog throughout the entire trust. Data from NHS England have shown that these delays have been increasing consistently, despite one-third of delays having been shown to be avoidable.Citation11 Two clear problems facilitate these delays; absence of a clear protocol in the discharge process and a lack of available, trained staff competent in discharging patients.
Discharging a patient must become a core goal in treatment, and hence the discharge process must be planned as soon as a patient is admitted. Implementing a guideline-based discharge system, specific to various patient pathways, would significantly decrease length of stay.Citation12,Citation13 Diversifying the workforce by multiskilling nurses can speed up the discharge process when doctors are scarce, allowing discharges to proceed more efficiently.Citation14,Citation15 An educational program must be established, with focus on protocol-driven discharge, ensuring a regulated diffusion of responsibility from doctors to nurses.Citation16
Conclusion
There are many factors contributing to the growing waiting times within the NHS. We have identified three key areas that contribute to waiting and have outlined general strategies for their improvement. We agree with Zaghloul and El Enein that each health care system must focus on scheduling of patients as a key method of optimizing resources,Citation1 although we have highlighted further areas to supplement reduction of waiting times. Ultimately, we believe that it is important to focus on all areas simultaneously in order to improve patient flow, as focusing on just one would shift strain on the system to a different area.
Disclosure
The authors report no conflicts of interest in this communication.
References
- ZaghloulAAZEl EneinNYAHourly-block and standard patient scheduling systems at two private hospitals in AlexandriaJ Multidiscip Healthc2010322523221289863
- SmithPMcKeonABluntIEdwardsNNHS hospitals under pressure: trends in acute activity up to 2022London, UKNuffield Trust2014 Report
- England NHSNHS diagnostic waiting times and activity dataLeeds, UK2015 Report
- SpahosTHindmarshACameronEEndoscopy waiting times and impact of the two week wait scheme on diagnosis and outcome of upper gastrointestinal cancerPostgrad Med J20058196172873016272239
- Bar-dayanYLeibaAWeissYCarrollJSBenedekPWaiting time is a major predictor of patient satisfaction in a primary military clinicMil Med20021671084284512392252
- Agency NHSM10 high impact changes for service improvement and deliveryLondon, UK2004 Report
- ChadhaRSinghAKalraJLean and queuing integration for the transformation of health care processes: a lean health care modelClin Governance2012173191199
- Comptroller, Auditor GNHS waiting times for elective care in EnglandLondon, UKNational Audit Office2014 Report
- StrausSGChenAHYeeHJrKushelMBBellDSImplementation of an electronic referral system for outpatient specialty careAMIA Annu Symp Proc201120111337134622195195
- CymruANHS waiting times for elective care in Wales technical reportWales Audit Office 2015 Contract No: Report
- England NHSDelayed Transfer of Care Time SeriesNHS England. Delayed Transfer of Care Time SeriesLeeds, UK2015 Report
- Nottingham University HDischarge case study – Nottingham University Hospital NHS TrustNottingham, UK2014 Report
- MaloneyCGWolfeDGestelandPHHalesJWNkoyFLA tool for improving patient discharge process and hospital communication practices: the “patient tracker”AMIA Annu Symp Proc2007200749349718693885
- Improvement IfHTry Scheduling Hospital DischargesCambridge, MAImprovement IfH2015
- CrockerCKellerRNurse-led discharge to the ward from high dependency: a service improvement projectIntensive Crit Care Nurs200521636336616271294
- LeesLMaking nurse-led discharge work to improve patient careNurs Times200410037303215485146