Abstract
Background
Major lower limb amputations result in a significant sense of loss, psychological stress, and decrease in function and overall quality of life for the amputee. The holistic, patient-centered prosthetic rehabilitation of an amputee requires input from a team of dedicated health professionals from different disciplines commonly referred to as a multidisciplinary team (MDT). MDT rehabilitation is considered crucial in the reintegration of the amputee into the community, as well as for providing psychological support after limb loss. Multidisciplinary and interdisciplinary rehabilitation has been proven to be more successful than therapy provided by individual therapists in a number of different populations, regardless of the population studied. However, in most developing countries, there is a significant lack of multidisciplinary rehabilitation.
Aim
To explore the roles and challenges of the members of the MDT involved in trans-tibial amputation rehabilitation in a rural community in South Africa (SA).
Design
An explorative sequential qualitative descriptive study.
Setting
A rural district in the KwaZulu Natal province in SA.
Participants
Nine prosthetic users, three surgeons, three traditional healers, 17 therapists, four prosthetists, and four community health workers.
Instruments for data collection
Semistructured interviews and focus group discussions.
Results
The roles of the members of the MDT were clarified, and various members of the MDT highlighted specific challenges relating to their experiences and roles in the rehabilitation team. Lack of interdisciplinary rehabilitation and communication among team members, as well as lack of resources, and patient education negatively impact the rehabilitation of trans-tibial amputees.
Conclusion
Aiming to address the limited resources available to health care professionals, as well as improved communication and interdisciplinary rehabilitation, could potentially improve the overall rehabilitation of persons with a lower limb amputation in the rural setting.
Background
Interdisciplinary rehabilitation has been proven the gold standard when considering patient outcomes, regardless of the population being studied.Citation1 Optimum rehabilitation of the person with an amputation is dependent on the cooperation and interaction of a number of different health care professionals commonly referred to as the multidisciplinary team (MDT).Citation2
Even though multidisciplinary rehabilitation has been hailed as the ideal for post-amputation prosthetic rehabilitation and accepted as the standard of care in most developed countries, it is still lacking in many developing countries.Citation2 Different health care professionals are involved in the rehabilitation of any person with a disability, but most often physiotherapists are in charge of the physical rehabilitation process in developing countries.Citation3 Prosthetic rehabilitation and service delivery in developing countries and especially in a rural setting are very challenging.Citation4–Citation6 Some of these problems include 1) inaccessibility of health care services, 2) systemic barriers, 3) lack of trained rehabilitation personnel to provide rehabilitation services, 4) inappropriate preparation of health care personnel for rural settings, 5) difficulty attracting and retaining staff, 6) lack of coordinated multidisciplinary services, 7) inappropriate assistive devices, and 8) lack of research and evidence-based practice.Citation4–Citation8
The MDT involved in amputation rehabilitation in an urban setting usually includes the surgeon, therapists, social worker, and prosthetists.Citation9 In traditional rural areas, the traditional healers and community caregivers (CCGs) are also involved in the management of a patient’s health and can be considered part of the MDT.Citation10 An increasing number of the poorest people living in rural areas in South Africa (SA) are using at least 10% of their monthly income seeking health care from traditional healers.Citation11 Currently, there is a paucity of literature on the roles and challenges of the MDT involved in trans-tibial amputation rehabilitation in a rural setting, and no study has explored the roles of traditional healers as part of the MDT in any type of rehabilitation.Citation12
Statement of the problem
Coordinated multidisciplinary rehabilitation is rarely practiced in developing countries.Citation13 In order to explore the reasons for the lack of MDT rehabilitation in this setting, the challenges that the members of the MDT face with providing MDT rehabilitation had to be identified. The MDT involved in rural rehabilitation in this specific setting also includes traditional healers and at times midlevel therapy workers such as CCGs and community health workers (CHWs). However, the roles of these members of the MDT have not been explored and need to be clarified in order to recognize them as members of the MDT.
Aim of the study
The aim of this study was to identify the different roles and challenges experienced by the members of the MDT involved in lower limb prosthetic rehabilitation in a rural setting in SA.
Methodology
Design
A qualitative, sequential explorative study design was used to collect data for this study.
Population and sampling
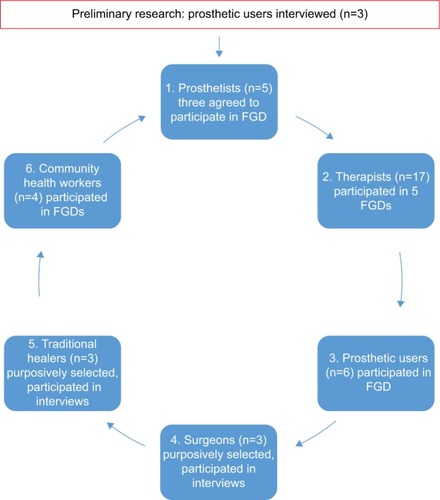
The study population included persons with a lower limb amputation and all the health care professionals (physiotherapists, occupational therapists, surgeons, prosthetists, care workers, and traditional healers) who provided prosthetic services to this specific rural district. Persons with a lower limb amputation were conveniently sampled, while a purposive sampling strategy, based on their involvement in prosthetic service delivery, was used to recruit the members of the MDT. The sample size of each population group is illustrated in . This study was approved by the University of the Western Cape’s ethics committee (Reg nr. 11/4/3). Written informed consent was obtained from all participants to use their data in this study.
Data collection procedure
In order to obtain some indication of the current process of postamputation prosthetic rehabilitation that was followed in this district, three prosthetic users were conveniently sampled and interviewed by the researcher prior to the commencement of the study. These interviews verified that there are some challenges with prosthetic rehabilitation and service delivery in this specific rural setting. Following these interviews, the researcher conducted focus group discussions (FGDs) and interviews with all the relevant members of the MDT involved in prosthetic rehabilitation (prosthetic users, prosthetists, therapists, surgeons, traditional healers, and CCGs) in this area.
FGDs were utilized to collect data from the persons with a lower limb amputation, prosthetists, therapists, and CCGs. The medical staff and CCGs were all faced with one grand question in FGDs, “Can you please tell me more about your experiences working as a prosthetist/therapist/CCG in this rural setting?” Probing questions were then used to explore roles and challenges that were discussed in more depth. The participants with lower limb amputation were asked the question: “Can you please tell me more about your experiences of the rehabilitation process after your amputation?”
It was not possible to get the surgeons or traditional healers together in one location to conduct an FGD, and hence semistructured interviews were more appropriate. Some of the prosthetic patients needed a translator while others did not, so an FGD would not have been the most appropriate or convenient method of data collection for the patients involved. Therefore, semistructured interviews were used to interview the prosthetic patients, the surgeons, and traditional healers. Semistructured interviews were specifically chosen because of logistical as well as language difficulties experienced in the rural setting.
Data analysis
The qualitative data were analyzed using Cresswell’s process of thematic analysis.Citation14 Following these steps from working with raw data to interpreting the meaning of themes assists in validating the accuracy of the information obtained in qualitative research studies.Citation14 The interviews were transcribed verbatim and checked for any mistakes or missed words against the audio recording. Checking of transcripts improves the reliability of the findings.Citation15 All the interviews were conducted in English. The transcriptions were read and reread several times by the researcher in order to gain an overall understanding of the data before commencing with the coding process. Transcripts were coded making use of open and axial coding,Citation14 identifying common concepts in the participants’ responses. Codes were grouped into categories, similar categories were analyzed, and then emerging themes were identified.
Findings and discussion
Preliminary research: interviews with prosthetic users
From the three interviews that were conducted with persons with a lower limb amputation, three themes arose namely: 1) lack of rehabilitation, 2) difficulty accessing public transport, and 3) improved functionality with the use of a prosthesis.
Lack of rehabilitation
Of the three prosthetic limb users who were interviewed at the prosthetic clinic, two did not receive any rehabilitation in hospital after the amputation, before receiving a prosthesis, or after being fitted with the prosthesis. One participant received some “exercises” while in hospital, but no outpatient rehabilitation or prosthetic rehabilitation. The participant who did receive inpatient rehabilitation stated that he probably could have come back for therapy, but that he chose not to, because he “disliked hospitals”. The other two participants stated that they did not receive any information or rehabilitation after discharge from hospital, but that they came to the hospital to ask about receiving a prosthetic limb and were then referred to the monthly prosthetic clinic. They reported that after the initial fitting of the prosthesis, the prosthetist just checked that they were able to walk with the prosthesis and then they went home and did not return to hospital unless there was a problem with their prosthesis. In response to the question whether the persons with a lower limb amputation had received any therapy, exercise, or training from the hospital, they answered as follows:
Patient 1: “Yes, I had to go to hospital because there was something wrong with the leg, they tried to fix it.”
Patient 2: “No one told me to come for any training or exercise.”
Patient 3: “No one except you.”
Difficulty accessing public transport
Two participants who did not receive any rehabilitation also noted that difficulty accessing public transport would have made it difficult to come back to hospital for therapy if they were asked to come back for prosthetic rehabilitation.
Patient 2: “Yes you sometimes find that seats are not open enough, I have to wait for another one or must I hire a car to take (me) home.”
Patient 1: “It was difficult but I decided to buy a car.”
Improved functionality with the use of a prosthesis
All three prosthetic users felt that even though they did have some difficulty with their prostheses at times, it did help them to become functionally more independent.
Patient 3: “It’s easy because I can now do things myself, I do my washing, I am able to hang the washing on the wire, I do a lot of things.”
Patient 2: “I can go to the garden and do fencing”
Patient 1: “…even now I can cook”
From the interviews, it was clear that there was a definite challenge with prosthetic rehabilitation in this setting, and the specific roles and challenges experienced by the members of the MDT involved in prosthetic rehabilitation were subsequently explored.
Patient journey and referral pattern
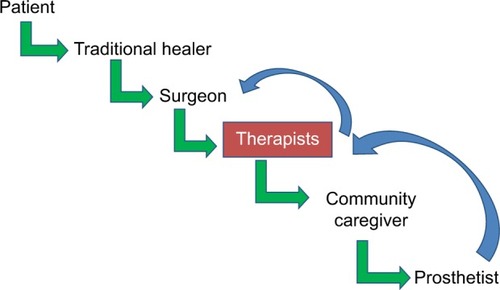
demonstrates the referral pattern of persons with a lower limb amputation.
The roles of the different members of the MDT involved in trans-tibial amputation were clarified and are presented in .
Table 1 Roles and referral pattern of members of the multidisciplinary team
The traditional healers were often the patient’s first point of contact when seeking medical attention. Traditional healers would then try and “treat” the patient with diabetic sepsis up to a point where the patient was systemically ill and then refer the patient to the hospital. The patient would be admitted to the hospital, and the general surgeon would perform the amputation in two stages (initial amputation and revision surgery). The surgeon would then refer the patient for inpatient therapy, where the therapists would do basic rehabilitation in the wards. This fact was confirmed by persons with a lower limb amputation. Patients were generally discharged before the residual limb was healed, so no stump bandaging or coning of the stump could take place. In some cases, therapists gave the patient a date to be followed up at their nearest clinic (serviced once a month). The patient would then be discharged and the CCGs (in areas where they were active) would follow up the patients, and try and do some counseling, and ensure (to some extent) that they took their diabetic medication. Because of poor socioeconomic circumstances and often cultural factors, patients would seldom return for follow-up, or a different therapist might see the patient, affecting the continuity of care. If the CCG or the therapist managed to follow up the patient, they might be referred to the prosthetic clinic (once a month) at the hospital, where they would inevitably be turned away because of lack of stump preparation and prosthetic rehabilitation, or they might be measured for a prosthesis, but then wait another 3 years to be fitted. This inadequate process of rehabilitation leads to extremely poor functional outcomes for patients who suffer a lower limb amputation in this rural setting. In order to identify the reasons for this inadequate process, the roles and challenges experienced by the MDT were explored in more depth qualitatively.
Roles of the members of the MDT
Persons with a lower limb amputation
The persons with a lower limb amputation were not included and recognized for their role as members of the MDT by most health professionals in this study. This finding is common in the disability literature where people with disabilities are not included in the planning of their own rehabilitation.Citation16 If people with disabilities were more involved in the decision-making process relating to their own health, it would empower them and improve patient buy-in and compliance with rehabilitation, which could result in improved rehabilitation outcomes.Citation17 A possible reason for not including the patient as part of the MDT could be the challenges raised by the therapists with regard to language barriers and the lack of appropriately trained translators.
Traditional healers
In this study, the role of the traditional healers was explored and clarified as the first point of contact for some patients in the community, especially those struggling to access health services. This finding confirms the National Department of Health’s suggestion that traditional healers might be the first point of contact for patients living in rural areas.Citation13 According to a recent study conducted on the feasibility of the use of mobile clinics in rural Mozambique, the need to recognize the role of traditional healers and for cooperation between Western and traditional medicine was also highlighted.Citation18 In this specific study, patients with HIV often sought help from traditional healers initially because of an environmental barrier to access health care, but traditional healers referred these patients to hospital, since they were trained to recognize the symptoms of HIV.Citation18 In a study conducted in SA, the traditional healers did not have any training in the signs or complications of diabetes mellitus that could result in lower limb amputation and continued to treat their patients to the best of their ability. They only eventually referred the patient to a hospital if the patient did not improve under their care. The implication of this finding is that patients often arrived at the hospital too late in order for their limbs or sometimes their lives to be saved.
CCGs
The CCGs are the closest link that the hospitals have to the community, and they refer patients with various disabilities to therapy or to the hospital. CCGs are a joint initiative by the South African Department of Health (DoH), Department of Social Development, the Office of the Premier and funded by the United States Agency for International Development (USAID). The CCGs fall under a project named “Operation Sukuma Sakhe” that was initiated by the provincial government of KwaZulu Natal (KZN) and aimed to improve health, reduce poverty, and empower vulnerable women and children. According to the BroadReach Healthcare initiative (which partners with the South African DoH on CCG training), the role of the CCG is to “connect households with service delivery entities to ensure that citizens are provided with health care and social services in their communities”.Citation19 Caregivers go through a 10-day training course in order to qualify as a CCG and are trained in basic health screening and education and referral to health services. The training addresses the needs of adults and children across the spectrum of diseases and disabilities.Citation19 Ideally, the CCGs would be the best situated to do the basic rehabilitation and stump bandaging required for prosthetic fitting, but it does not fall within the scope of practice of the CCGs. It should be done by CHWs or rehabilitation care workers. The roles and titles of CHWs are also not clearly defined and are very contextual.Citation20 CHWs are generally trained to assist health care professionals with the decentralization of health services away from the hospitals and provide home-based care.Citation20 Unfortunately, due to the poorly defined roles, lack of training, and low remuneration, there is a high turnover of CHWs, and retention is a problem.Citation20 This is consistent with the situation in this study where, for example, at one of the district hospitals, only one CHW was employed by the hospital, and he is also blind.
Surgeons
The role of the surgeons is clearly defined, and they are responsible for performing amputation surgery and refer the person with a lower limb amputation to the other members of the MDT for rehabilitation and counseling. Currently, all the members of the MDT in this study worked independently, and no planning or mutual rehabilitation goal setting was done. The reason for this lack of interdisciplinary teamwork that was clearly stated by the surgeons was lack of time due to shortage of surgical staff to perform all the procedures in a rural setting. If surgeons spent more time discussing patient goals and rehabilitation outcomes, they would not be able to perform the number of required surgeries.
Therapists
In this rural setting, the roles of the physiotherapists and occupational therapists were not clearly defined, and a transdisciplinary approach was mostly followed among therapists. This led to some difficulties relating to professional identity, especially among younger community service therapists. There is currently no other published study that explores the impact of transdisciplinarity on the professional identity of young therapists. This finding is concerning and should be explored in more depth in future research.
Prosthetists
There was a significant overlap between the roles of the prosthetists and that of the physiotherapists. In this rural area, prosthetists had to perform the coning of the stump and the prosthetic rehabilitation of the patients once patients were fitted with prostheses. This overlapping of roles or transdisciplinary approach in this setting is largely necessitated by the shortage of therapy staff as well as resources such as stump bandaging. The implication of this finding is that it adds to the workload of the prosthetists who are already also severely understaffed, leading to decreased productivity and an increased waiting time for patients awaiting prostheses. Prosthetists would ideally refer patients back to the therapists for prosthetic training once the person with a lower limb amputation had been fitted with a prosthesis, but due to the many challenges related to accessing health care services in this setting, patients rarely returned for follow-up or rehabilitation. The implication of this finding is a reduced rehabilitation outcome or often a prosthesis that is rendered useless owing to lack of rehabilitation and prosthetic training.
Challenges to prosthetic rehabilitation experienced by the MDT in a rural setting
A number of different discipline-specific challenges were highlighted by the different members of the MDT involved in trans-tibial amputation rehabilitation in this rural setting. However, only the common themes that were identified across all the disciplines of the members of the MDT will be presented in this paper. The four common challenges or themes that arose from across all the data were 1) effect on quality of care due to difficulty accessing health services, 2) lack of MDT rehabilitation, 3) cultural factors, and 4) staff shortages and lack of resources.
Impact of access to health services on quality of care
Prosthetists only visited some of the district hospitals on a monthly basis and were often not even able to do that owing to unforeseen circumstances such as bad weather. This often inconsistent service delivery affected the continuity of prosthetic patient care. The high cost of accessing health care services in rural areas is documented in a paper on the inequalities in access to health services in SA.Citation21 The high cost, coupled with poor service delivery, results in the disempowerment of patients as well as worse health outcomes in rural areas.Citation21
Therapists did provide inpatient rehabilitation with limited resources, but once the patients were discharged from hospital, they struggled to follow them up for prosthetic rehabilitation. Patients were often required to either rent a private car or try to make use of public transport to attend clinics or follow-up at the hospital. In a very poor rural community where the majority of people are unemployed and rely on social assistance grants, the cost of transport for rehabilitation services makes it inaccessible for the majority of the population.Citation21,Citation22
The environmental demands of the rough terrain that therapists have to accommodate in order to provide therapy also pose a significant challenge. In order to do clinic visits, therapists have to travel long distances (often more than 2 hours of driving in one direction) over rough terrain. Even though most hospitals do have a fleet of cars available for staff, not enough 4×4 vehicles or “bakkies” are available to accommodate various departments attempting to service all the rural clinics (Anonymous therapist, personal communication, June 11, 2012). This finding relating to the difficulty providing and accessing health care as a result of lack of transport in rural areas is also highlighted in the recent South African Health Review.Citation23 Late admission to hospital reported by the surgeons could also be attributed to the difficulty accessing public transport, as reported by persons with a lower limb amputation who were interviewed in this study.
Lack of MDT rehabilitation
Patients, prosthetists, therapists, surgeons, and traditional healers all highlighted lack of MDT rehabilitation. In this study, there was no coordination of efforts between the different team members. This finding corresponds with the findings of the only other South African study on amputation rehabilitation, which also stressed a lack of multidisciplinary rehabilitation.Citation3 The lack of an MDT approach negatively affects the rehabilitation outcomes of the patient and could explain the prosthetists’ problem related to inadequate rehabilitation for prosthetic fitting.Citation24,Citation25 Traditional healers were also asked to be recognized as part of the MDT and would like to work more closely with the hospitals. If the traditional healers could be recognized as part of the MDT and trained to know when to refer the patients to hospital, many lower limbs could potentially be saved. An MDT approach to the treatment of diabetes mellitus could also assist in the prevention of lower limb amputation in this setting.
Cultural factors
Health-seeking behavior
Therapists, prosthetists, and surgeons all reported on the difficulties caused by cultural factors affecting rehabilitation services in this rural setting. Therapists reported on how the belief regarding the cause of disease and illness affects health-seeking behavior as well as the quality of the therapy that therapists provided. Many patients still believed that illness was related to bewitchment and sought help from “Sangomas” (traditional healers) in order to appease their ancestors and remove the “curse”. This belief affected their trust in Western medicine and rehabilitation and could potentially have decreased adherence to rehabilitation.Citation11,Citation26 The surgeons involved in the study raised concerns that patients were usually admitted to hospital too late to save their limbs. One possible reason they provided (other than difficulty accessing health services) was that patients were managed by traditional healers and referred to hospital very late. This suggestion corresponded with the findings reported by another South African study in a rural context who noted that patients often sought out the services of traditional healers in rural areas.Citation11 It is also confirmed by the National DoH’s Human Resources for Health (HRH) policy document that recognizes traditional healers as the first point of contact for patients in rural areas.Citation13 The possible reasons for this are a strong influence of cultural beliefs on the cause of illness and travel distance from hospitals.Citation11 Care workers noted that sometimes family members of patients put pressure on the patient rather to consult a traditional healer before seeking Western health care. This could be due to a fear that the patient’s “curse” could be transferred to them if the patient does not adhere to cultural practices. The whole situation seemed to be worsened by the fact that the traditional healers believed that they were better at preventing amputations than the hospitals were.
Choice of service provider
In some hospitals, culture also affected the patients’ choice of service provider, where patients refused to be treated by therapists from their own area and race. This finding has not been reported in the literature, but can potentially be explained by the fact that historically hospitals in the rural settings of SA were run by European missionaries.Citation27 Today, still patients in these areas seem to believe that European doctors or therapists are better qualified to treat them than people who grew up in their own communities. This finding is just based on discussion from the therapists’ perspectives and should be further explored from the patients’ perspectives.
Language barriers
Another cultural factor that challenged the prosthetists as well as the therapists was the language barrier experienced by most of the health professionals working in this setting. The majority of medical professionals in this district at the time of data collection were English-speaking and could not speak isiZulu (the local language) fluently. This language barrier negatively affected the rehabilitation team’s ability to diagnose (in some instances), counsel, educate, and provide quality rehabilitation services. This finding is echoed by the findings of a study on assessing and treating patients with back pain in a rural community in SA.Citation11 The clinical implication of this finding is that medical staff who aspire to work in rural areas should have an understanding of the cultural beliefs that will affect the services that they provide and be competent in the local language of the area in which they want to work.
Staff shortages and lack of resources
Prosthetists noted that severe staff shortages hampered their ability to provide a quality service to persons with a lower limb amputation in the rural areas. This finding corresponds with an earlier study that declared prosthetic service delivery in developing countries a problem owing to lack of a sufficient number of prosthetists being trained to meet the growing demands of persons with a lower limb amputation in developing countries.Citation28 It also corresponds with the recent guidelines on “rural-proofing policy and resourcing for health in rural areas” that highlight the severe shortage of HRH care in rural areas.Citation29,Citation30
Therapists were understaffed and did not have enough equipment or vehicles to provide the Comprehensive Community-Based Rehabilitation services that rural settings call for.Citation31 At a certain hospital, there were only two permanent physiotherapy posts to service the whole hospital, as well as a community of ~100,000 people spread over a surface area of 3,000 km2. They also had two community service posts that were not filled every year, but even with four physiotherapists, it would still be a ratio of one therapist to 25,000 patients over 750 km2. At another hospital in this district, one physiotherapist and one occupational therapist serviced the hospital, 17 rural clinics as well as a population of 200,000 people. This finding is important because therapy staff can be overwhelmed by the size of their workload in this setting and either be discouraged to continue working in rural settings or suffer burnout. Shortage of therapy staff working in rural areas is a common problem worldwide and corresponds with an Australian study that reported that very few rehabilitation therapists were employed in rural areas to meet the demands of the population that they served.Citation32 Considering the increased demand for rehabilitation services in rural settings owing to the increased incidence of disabilities, these immense staff shortages should be seriously considered and addressed by the National Department of Health. However, some measures such as the employment of community service officers have been taken in order to address the staff shortages in rural areas. The retention of community service officers in rural areas is vitally important to assist in solving the lack of medical staff servicing rural areas.Citation22 A major problem experienced by the therapists was that even though the majority of the current community service therapists reported that they would be willing to stay in the rural setting if they were offered a permanent position, no new posts for therapists were being created. This could be due to a “freezing” of posts as a result of overspending in rural hospitals as is advised against in Objective 8.1 of the National DoH’s HRH strategy for human resource attraction and retention in rural areas.Citation13 This finding is contrary to the recommendations made by the DoH to improve the retention of medical staff in rural areas.Citation22
Therapists also reported feeling the burden of transdisciplinarity and being viewed as a therapist without a specific professional identity. Transdisciplinarity within a discipline-specific scope of practice can be considered a positive learning experience for experienced therapists, but for younger inexperienced therapists who have not formed a professional identity (such as community service therapists), transdisciplinarity can be confusing. If their roles are confusing and they are not sure about their scope of practice, it could result in difficulty for community service therapists once they have completed their community service and enter the job market again. Crossing the boundaries of the discipline-specific scopes of practice could also have negative legal implications if therapists are practicing outside of their scope of practice and an injury to the patient occurs. A negative community service experience also discourages medical professionals from remaining in the public health system.Citation22 The rural communities rely heavily on the services of community service medical staff, and staff attraction and retention in rural areas should be of utmost importance to the National DoH.Citation22
Study limitations
A minor limitation encountered in the data collected was the convenience sampling strategy that had to be used to select the traditional healers and CCGs who were involved in the study. Even though the total number of traditional healers and CCGs could only be estimated, the sample included in the study would not be representative of the total population they belonged to. Therefore, the findings based on the data obtained from them cannot be generalized to the total population they present. However, it is a small step toward recognizing the roles of the traditional healers and CCGs as part of the MDT involved in amputation rehabilitation and can provide a baseline for future interventions and better relationships between practitioners of traditional and Western medicine.
Conclusion
The aim of this study was to clarify the roles of the members of the MDT in prosthetic rehabilitation in a rural setting. In this study, the traditional healers were identified as the first point of contact; CCG’s referred potential patients to the hospital for further management; the surgeons performed the amputation (when required); and there was a significant overlap in the roles of the physiotherapists, occupational therapists, and prosthetists. The different members of the MDT all face very specific difficulties in providing quality rehabilitation services, but common challenges that arose across all disciplines were the effect of access to health services on quality of care, lack of MDT rehabilitation, the effect of cultural factors, staff shortages, and lack of resources.
Poor rehabilitation is a health systems problem, more than just an MDT problem. Addressing the challenges experienced by the members of the MDT and encouraging interdisciplinary rehabilitation could potentially solve some of the health system problems in this area.
Disclosure
The authors report no conflicts of interest in this work.
References
- MomsenAMRasmussenJENielsenCVIversenMDLundHMultidisciplinary team care in rehabilitation: an overview of reviewsJ Rehabil Med2012441190191223026978
- EsquenaziAAmputation rehabilitation and prosthetic restoration. From surgery to community reintegrationDisabil Rehabil20042614–1583183615497912
- KaplanSLOutcome Measurement and Management: First Steps for the Practicing ClinicianPhiladelphiaFA Davis Company2007
- EklundAImplementing P&O Services in Low-Income SettingsISPO Prosthetics and Orthotics programme guide2006
- StraitEProsthetics in Developing Countries2006 Available from: http://www.oandp.org/publications/resident/pdf/DevelopingCountries.pdfAccessed April 29, 2015
- WHOWorld Report on DisabilityGenevaWorld Health Organisation2011
- WHOJoint Position Paper on the Provision of Mobility Devices in Less-Resourced Settings: A Step Towards Implementation of the Convention on the Rights of Persons with Disabilities related to Personal MobilityGenevaWorld Health Organisation2011
- WHOGuidelines for Training Personnel in Developing Countries for Prosthetic and Orthotic ServicesGenevaWorld Health Organisation2005
- YinusaWUgbeyeMEProblems of amputation surgery in a developing countryInt Orthop200327212112412700939
- MaddenVJO’SullivanPFisherJMalambuleBOur training left us unprepared’ – two physiotherapists’ reflections after working with women with low back pain in a rural Zulu community in South AfricaJ Community Health Sci201382
- NxumaloNAlabaOHarrisBChersichMGoudgeJUtilization of traditional healers in South Africa and costs to patients: findings from a national household surveyJ Public Health Policy201132suppl 112413610.1057/jphp.2011.26
- Department of HealthHRH Strategy for the Health Sector:2012/13–2016/17South Africa2011 Available from: http://www.gov.za/sites/www.gov.za/files/hrh_strategy_0.pdfAccessed May 18, 2015
- FredericksJPVisagieSThe rehabilitation programme and functional outcomes of persons with lower limb amputations at a primary level rehabilitation centreS Afr J Occup Ther20134331828
- CreswellJWResearch Design: Qualitative, Quantitative and Mixed Methods Approaches3rd edLondon, EnglandSAGE Publications2009
- GibbsGRAnalyzing Qualitative DataSAGE publications2007 10.4135/97818492085749781849208574Accessed February 19, 2015
- WHOInternational Classification of Function, Disability and Health (ICF)GenevaWorld Health Organisation2001
- LusardiMMPostoperative and pre-prosthetic careLusardiMMJorgeMNielsenCCOrthotics and Prosthetics in Rehabilitation3rd edSt. Louis, MissouriElsevier2013532594
- SchwittersALedererPZilversmitLBarriers to health care in rural Mozambique: a rapid ethnographic assessment of planned mobile health clinics for ARTGlob Health Sci Pract20153110911625745124
- BroadReach HealthcareUSAID and US Embassy Officials Visit BroadReach Healthcare Community Caregiver Trainings in Ugu District, KZN – December 4–5, 20122012 Available from: http://www.broadreachhealthcare.com/gh/wp-content/uploads/2014/04/Article_Official-visits-in-Ugu.pdfAccessed March 26, 2015
- MwaiGWMburuGTorpeyKFrostPFordNSeeleyJRole and outcomes of community health workers in HIV care in sub-Saharan Africa: a systematic reviewJ Int AIDS Soc2013161858624029015
- HarrisBGoudgeJAtagubaJEInequities in access to health care in South AfricaJ Public Health Policy2011321102123
- CookeRCouperIVersteegMHuman resources for rural healthGrayAVawdaYJackCSouth African Health Review 2011DurbanHealth Systems Trust2011107117
- GaedeBVersteegMChapter 9: The state of the right to health in rural South AfricaSouth African Health Review2011
- ClarkeDJThe role of multidisciplinary team care in stroke rehabilitationProg Neurol Psychiatry2013174510
- NeumannVGutenbrunnerCFialka-MoserVInterdisciplinary team working in physical and rehabilitation medicineJ Rehabil Med201242148
- WegnerLRhodaAThe influence of cultural beliefs on the utilisation of rehabilitation services in a rural South African contextAfr J Disabil2015418
- Department of Health: KwaZulu Natal (DOH: KZN). [webpage on the Internet]A Brief History of Mosvold Hospital2001 Available from: http://www.kznhealth.gov.za/Mosvold/history.htmAccessed June 13, 2015
- PearlmanJCooperRAKrizackMLower-limb prosthesis and wheelchairs in low income countries. An overviewIEEE Eng Med Biol Mag20082721222
- Rural Health Advocacy Project (RHAP)Rural-Proofing for Health: Guidelines. A Guide to Accounting for Rural Contexts in Health Policy, Strategic Planning and Resourcing2015 Available from: http://www.rhap.org.za/wp-content/uploads/2015/02/2015-01-13-RHAP-Rural-Proofing-Guideline-A4-Email-1.pdfAccessed April 2, 2016
- Rural Health Advocacy Project (RHAP) and PartnersThe WHO global policy recommendations on increasing access to health workers in remote and rural areas through improved recruitment and retention: The South African Context, Version 2 Discussion document2013
- WHOCommunity Based Rehabilitation Guidelines: Health ComponentGenevaWorld Health Organisation2010
- WilsonRDLewisSAMurrayPKTrends in the rehabilitation therapist workforce in underserved areas: 1980–2000J Rural Health2009251263219166558